Abstract
Objectives
This study aimed to compare nurses' satisfaction with, and expectations of, hospital information systems in two teaching hospitals.
Methods
This was a survey study, which was completed in 2014. The potential participants were 267 nurses who worked in two teaching hospitals and used the same hospital information system. Data were collected using two questionnaires. Both questionnaires were examined in terms of content validity and reliability.
Results
The results showed that, for a majority of nurses, their expectations of the system were not met in either hospital. Moreover, there was a significant association between the nurses' expectations and the perceived usefulness of the systems (p < 0.001), between the nurses' expectations and their satisfaction with the systems (p < 0.001), and between the perceived usefulness and nurses' satisfaction with the systems (p < 0.001).
Conclusions
The results suggested that, apart from the technical issues of implementing clinical information systems, non-technical factors should be taken into account. Among them, the nature of clinical tasks and the organizational culture require more attention to allow a successful system to be designed and implemented.
Electronic nursing documentation systems are part of larger clinical or hospital information systems, and they have been designed to support nurses in their daily practices [12]. Generally, the successful implementation of an information system or its subsystems depends upon the system design, which has to be technically in a good condition, and the willingness of the users to use the new technology [3]. While nurses' acceptance of, or satisfaction with computerized systems is a critical factor for the successful implementation of clinical information systems [4], sometimes nurses resist using such technology. Their reluctance might be due to a number of technical issues that need to be considered to integrate such systems with clinical practices, and the non-technical aspects, such as nurses' perspectives on the advantages of using the systems, compatibility of the new technology with their values, and system flexibility and usability [45].
Apart from the factors noted above, age, educational level, work experience, and computer skills have frequently been described as factors influencing nurses' attitudes towards computerisation [6]. Moreover, the relationship between users' expectations and their experiences of information systems has been discussed in many studies. The literature shows that unknown or unrealistic expectations of users are still among the main hurdles to the success of information system implementation [7]. Therefore, understanding the expectation–experience gap will be of great value to both research and practice. Furthermore, an understanding of factors that can influence the use of a clinical information system can help to improve user acceptance and may lead to effective use of the technology [89].
Another determinant of success or failure of hospital information systems is user satisfaction [10]. The literature shows that there is a significant positive relationship between 'system usage' and 'user satisfaction' [11]. Moreover, based on the expectation confirmation theory, user's expectations before and after using the technology play an important role in determining the level of user satisfaction [12]. User satisfaction determines how much an information system matches the requirements of a user [13]. Since nurses are a great part of the workforce in hospitals and deal with a huge volume of information, investigating their expectations is quite important to ensure that a nursing or hospital information system is able to meet their requirements [14].
Iran is a developing country in which the use of clinical information systems began 30 years ago. However, hospital information systems are developed by private information technology (IT) companies and they are not consistent [15]. While e-health and Electronic Health Records (EHRs) have received particular attention in the country since 2000, few studies have been conducted in relation to nurses' expectations of and satisfaction with information systems [41617]. In the current study, we aimed to investigate these two determinants of system success among nursing staff. As nurses are the largest group of system users in healthcare organizations, it is important to consider their requirements in future system development and implementation.
This was a survey study completed in 2014 in Tehran, Iran. Before the study was conducted, the research proposal was reviewed by the Institutional Review Board, and the ethics approval was obtained. The potential participants of the study were nurses who worked in two selected teaching hospitals. A sample of 267 nurses was selected using a sampling formula (n = z2pq/d2). The sample included 126 nurses from hospital A and 141 nurses from hospital B. Nurses were selected from all wards of the hospitals and from various shifts by using convenience sampling method (3 nurses from the day shift, 2 nurses from the evening shift, and 1 nurse from the night shift).
The research setting included two general teaching hospitals in which two different hospital information systems were used. Hospital A had 450 beds, and hospital B, which was one of the largest and oldest hospitals in the city, had 1,000 beds. The total numbers of nurses who worked in hospital A and hospital B were 224 and 250, respectively. In terms of the hospital wards, hospital A included 22 wards, and hospital B consisted of 24 wards.
To evaluate nurses' satisfaction with and expectations of hospital information systems, two questionnaires were designed based on the literature review [1819202122]. Both questionnaires employed a 5-point Likert scale which ranged from strongly agree (5), agree (4), no idea (3), disagree (2), strongly disagree (1). The first questionnaire included 56 questions and was designed to determine the nurses' expectations of the hospital information system before using the system. In this questionnaire, simple past tense was used to identify nurses' expectations. The questionnaire included two main parts: personal information (12 questions) and nurses' expectations of the system (9 subsections, 44 questions).
The second questionnaire was designed to identify nurses' perceptions after system implementation. The second questionnaire included four main sections, intention to use (3 questions), users' satisfaction (3 questions), perceived usefulness (7 questions), and nurses' expectations of the system (9 subsections, 44 questions). The last section of this questionnaire included the same questions as the first questionnaire. However, simple present tense was used to form questions in order to identify nurses' perceptions about the current status of the system. The content validity of the questionnaires was checked by four experts in the field of medical informatics and health information management. The reliability of the questionnaire was calculated by using Cronbach's α correlation coefficient. The reliability scores of the first and the second questionnaires were α = 0.80 and α = 0.70, respectively.
Data were analyzed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). In this study, each participant was asked to complete two questionnaires, the first one was related to the expectations of the system, and the second one was related to satisfaction with the system. After the data were collected, mean values were calculated for both questionnaires completed by a participant. If the difference between the mean values of the questionnaires was a positive number, it meant that the expectations of nurses were met, and if the difference between the mean values was a negative number, it showed that the nurses' expectations were not met. In addition, t-test and Pearson correlation coefficient were used to identify any significant difference before and after system implementation.
In total, 95 nurses (75%) from hospital A and 83 nurses (59%) from hospital B took part in this research. In hospital A (62.1%) and hospital B (47%), the highest frequency was related to the age group of 23–29 years, and most of the participants in hospital A (92.6%) and hospital B (95.2%) were women. In hospital A (76.8%) and hospital B (60.2%), the highest frequency was related to working experience of 1–6 years (Table 1).
Regarding computer skills, in hospital A, the greatest frequency (38.9%) was related to those nurses that assessed their skills at a good level, whereas in hospital B, (41%) the greatest frequency was related to those nurses who believed that their skills were at a medium level. Most of the nurses in hospital A (71.6%) and in hospital B (72.3%) believed that their knowledge about hospital information systems was at a medium level. Also, regarding nurses' satisfaction with the computer training that they had received, the highest frequency in hospital A (60%) and in hospital B (63.9%) was related to those nurses who expressed their satisfaction at a medium level.
The results showed that, before using the system in hospital A, most nurses (77.9%) expected that the nursing information system would be designed based on the users' requirements, fit between the tasks and technology would be considered (85.2%), the output of the system would be in an appropriate format (84.2%), and they would receive adequate training in the use of the system (92.6%). Moreover, nurses expected to use an easy to learn system (84.2%), to use their skills in the future and in relation to other systems (85.3%), and to feel satisfaction when using a new system (76.9%). Regarding the system's quality, a majority of nurses expected that the system would help to reduce medical errors during patient care (87.4%), to increase the accessibility of information (87.4%), and to facilitate the process of documentation (90.5%). Generally, before system implementation, nurses' attitudes towards using the system were positive, and they expected that learning the system should be a necessary part of their profession (91.5%).
In hospital B, the results showed that, before using the system, most nurses expected that the system would accelerate their daily tasks (84.3%), fit between the tasks and technology would be considered (90.4%), information needs of nurses would be met (90.4%), and they would receive adequate training in the benefit of the system (90.4%). Other expectations included ease of learning (84.3%), positive impact of the system usage on their job promotion (85.7%), and satisfaction when using a new system (74.7%). In terms of the system quality, a majority of nurses expected reduction of errors in the documentation processes (89.1%), acceleration of documentation (89.1%), and facilitation of drug administration (90.4%). Generally, before system implementation in hospital B, nurses' attitudes towards using the system were positive, and they expected to see a useful system (92.8%).
Regarding nurses' perceptions after using the system, most nurses in hospital A expressed that they intended to continue using the system (85.2%). In comparison with the manual system, they were satisfied with the electronic one (67.4%), and in terms of the perceived usefulness, they assumed that the system had improved their efficiency (68.4%).
Similarly, most nurses in hospital B intended to continue using the system (85.5%), and they were satisfied with the system (68.7%). Regarding the perceived usefulness, about half of the participants assumed that the system had helped them to speed up the completion of their daily tasks (51.8%).
To investigate the extent that the system has been successful in meeting nurses' expectations, their expectations were compared with their perceptions of the current system (Table 2).
As shown in Table 2, in both hospitals, the highest frequency was related to those nurses whose expectations of the system were not met. The results also showed that there was no significant difference between the perceived usefulness of the system (p = 0.09), users' satisfaction with the system (p = 0.65), and meeting users' expectations (p = 0.09) for the two hospitals.
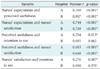
In this study, the correlations between selected variables were examined using Pearson correlation coefficient (Table 3).
As shown in Table 3, meeting nurses' expectations could result in improving perceived usefulness of the system and nurses' satisfaction with the system. The perceived usefulness of the system could positively influence nurses' intention to use the system in hospital A. However, there was no significant relationship between these two variables in hospital B. The results also showed that the perceived usefulness of the system could positively influence nurses' satisfaction with the system in both hospitals. While nurses' satisfaction with the system could positively influence intention to use the system in hospital A, no significant relationship was found between these two variables in hospital B.
The integration of IT into clinical processes must be analyzed and evaluated during the different phases of deployment of a clinical information system in order to improve system's quality and effectiveness [23]. This evaluation should occur pre-implementation, during implementation, and post-implementation to identify various technical and non-technical factors influencing the use of the clinical information system [24].
Nursing information systems can enhance the efficiency and quality of nursing practice. However, a lack of alignment between users' perceptions and systems' functionalities may lead to users' dissatisfaction [25]. In the current study, nurses' expectations of and satisfaction with hospital information systems were investigated. Although nurses used the same system in two teaching hospitals, the results showed that their expectations and the level of meeting their expectations were different in both hospitals. In both hospitals, the common expectations included fit between the tasks and technology, ease of learning, satisfaction when using a new system, and facilitation of the process of documentation. Similarly, in the study conducted by Lapinsky et al. [26], nurses expected an ICU clinical information system to reduce the time that a nurse spends on documentation and to allocate more time for patient care. Banner and Oleny [27] found that the hospital information system had improved nurses' efficiency and they could spend more time on patient care. Moreover, the system had improved documentation processes and accessibility of patients' information. In another study, the amount of data that must be entered into the computer by nurses and the nature of their work were reported as possible factors influencing satisfaction with the information system [4].
According to the results of the present study, nurses' expectations of the system had not been fully met in either hospital. In particular, in hospital B, the number of nurses who felt their expectations were not met was greater than in hospital A. It seems that the difference between the nurses' expectations and satisfaction reported in this study might be related to the nature of their clinical work and their organizational culture [24]. As hospital B was one of the largest teaching hospitals in the city, the nurses' clinical work might be more complex than the clinical tasks in hospital A, and as a result, the system was less successful in meeting their expectations.
Interestingly, despite the unmet expectations, most nurses of both hospitals intended to continue using the system. They were satisfied with the current electronic system compared to the previous paper-based system, and in terms of the perceived usefulness, most of them assumed that the system had improved their efficiency. It is notable that primary acceptance of information systems is regarded as the first step to successful deployment of the systems. However, an overall system's success depends upon the continuance of the system's usage [18].
The results showed that there was a positive association between meeting nurses' expectations and the perceived usefulness of the system and nurses' satisfaction with the system. Similarly, Palm et al. [23] found that users' expectations were strongly associated with perceived usefulness. In their study, nurses' satisfaction was significantly determined by support (training in the use of the system), perceived ease of use, and expectations. The results of the current study are also in line with the findings reported by Lin [25].
In the present study, the results suggest that the perceived usefulness of the system could have positively influenced nurses' satisfaction with the system in both hospitals. The perceived usefulness of the system also could have positively influenced nurses' intention to use the system in hospital A. However, there was no significant association between these two variables in hospital B. Moreover, no significant association was found between nurses' satisfaction and intention to use the system in hospital B; however, in hospital A, nurses' satisfaction with the system could positively influence their intention to use the system. According to the literature, the perceived usefulness of clinical information systems is an important factor in explaining and foreseeing users' intention to use the systems [2628]. In another study, Tabibi et al. [29] showed that there was a positive association between users' satisfaction with a hospital information system and their intention to continue using the system. It means that the more users are satisfied with a hospital information system, the more they intend to continue using the system.
In the current study, the results for the two hospitals were different. It seems that in hospital B, the use of the system was mandatory, and the organizational culture was strict. Therefore, nurses' satisfaction and perceived usefulness of the system did not influence system usage. However, in hospital A, although the use of the system was mandatory, the organizational culture was flexible enough to respect nurses' satisfaction with and perceptions of the system, and nurses could express their feelings and attitudes towards using the system. The results are also in line with the literature on the implementation of clinical information systems in which the socio-technical nature of clinical information system implementations and the interactions between technology, people, and organizational routines and culture have been emphasized [24].
It is notable that the current study had some limitations. First of all, the convenience sampling method was applied, and the sample was limited to those nurses who worked in two teaching hospitals and used the same hospital information system. Although nurses who completed the questionnaires worked in different departments, the study would benefit if the results could be generalized to a bigger sample size.
Moreover, this study aimed to investigate nurses' expectations of and satisfaction with hospital information systems; however, the system had been implemented in both hospitals a few years ago. Therefore, conducting a before-after study was not possible and the researchers decided to find an alternative solution which was investigating users' perceptions. Obviously, conducting a before-after study where possible can help to present more realistic perceptions. Furthermore, the impact of using nursing information systems, in terms of saving time, increasing work efficiency and effectiveness, and improving quality of care can be investigated in future studies by using objective evaluation methods.
In conclusion, the results obtained by the current study support the results of previous studies regarding the system's implementation. According to the study findings, apart from the technical issues of clinical information systems, non-technical factors are of high importance in successful implementation of these systems. Among them, the nature of clinical tasks and the organizational culture require more attention to ensure that systems are designed to meet users' expectations. Expectation disconfirmation may lead to users' dissatisfaction with a system, which can be followed by resistance to using the system and the system's failure. Therefore, conducting evaluation studies at any point of before, during, or after system implementation is necessary to identify the strengths and weaknesses of a system from the users' perceptions. This approach can help an implementation team to set appropriate expectations regarding what a system will and will not do, and thereby set the implementation up for success rather than a potential mismatch of user expectations and reality.
Figures and Tables
Table 2
Nurses' expectations before and after using hospital information systems

Values are presented as number (%).
If the difference between the mean values of the questionnaires for each participant was a positive number, it wasconcluded that his/her expectations were met and if the difference between the mean values was a negative number, it was concluded that the nurse's expectations were not met.
References
1. Ammenwerth E, Rauchegger F, Ehlers F, Hirsch B, Schaubmayr C. Effect of a nursing information system on the quality of information processing in nursing: an evaluation study using the HIS-monitor instrument. Int J Med Inform. 2011; 80(1):25–38.

2. Wang N, Yu P, Hailey D. Description and comparison of documentation of nursing assessment between paper-based and electronic systems in Australian aged care homes. Int J Med Inform. 2013; 82(9):789–797.

3. Hsiao JL, Chang HC, Chen RF. A study of factors affecting acceptance of hospital information systems: a nursing perspective. J Nurs Res. 2011; 19(2):150–160.

4. Kahouei M, Baba Mohammadi H, Askari Majdabadi H, Solhi M, Parsania Z, Said Roghani P, et al. Nurses' perceptions of usefulness of nursing information system: module of electronic medical record for patient care in two university hospitals of Iran. Mater Sociomed. 2014; 26(1):30–34.

5. Vezyridis P, Timmons S, Wharrad HJ. Implementation of an emergency department information system: a qualitative study of nurses' attitudes and experience. Comput Inform Nurs. 2012; 30(10):540–546.
6. Kipturgo MK, Kivuti-Bitok LW, Karani AK, Muiva MM. Attitudes of nursing staff towards computerisation: a case of two hospitals in Nairobi, Kenya. BMC Med Inform Decis Mak. 2014; 14:35.

7. Brown SA, Venkatesh V, Goyal S. Expectation confirmation in technology use. Inf Syst Res. 2012; 23(2):474–487.

8. Ayatollahi H, Bath PA, Goodacre S, Lo SY, Draegebo M, Khan FA. What factors influence emergency department staff attitudes towards using information technology? Emerg Med J. 2013; 30(4):303–307.

9. Ayatollahi H, Bath PA, Goodacre S. IT in the emergency department: what is the impact of technology? In : Proceeding of the 2nd International Conference on Health Informatics; 2009 Jan 14-17; Porto, Portugal. p. 454–457.
10. Pourasghar F, Tabrizi JS, Ala A, AsghariJafarabadi M, Daemi A. Satisfaction and perception of emergency department personnel on electronic triage system. Iranian J Med Inf. 2015; 4(1):1–5.
11. Bokhari RH. The relationship between system usage and user satisfaction: a meta-analysis. J Enterp Inf Manag. 2005; 18(2):211–234.

12. Aggelidis VP, Chatzoglou PD. Hospital information systems: measuring end user computing satisfaction (EUCS). J Biomed Inform. 2012; 45(3):566–579.

13. Delone WH, McLean ER. The DeLone and McLean model of information systems success: a ten-year update. J Manag Inf Syst. 2003; 19(4):9–30.

14. Lu CH, Hsiao JL, Chen RF. Factors determining nurse acceptance of hospital information systems. Comput Inform Nurs. 2012; 30(5):257–264.

15. Ayatollahi H, Mirani N, Haghani H. Electronic health records: what are the most important barriers? Perspect Health Inf Manag. 2014; 11:1c.
16. Sharifian R, Askarian F, Nematolahi M, Farhadi P. Factors influencing nurses' acceptance of hospital information systems in Iran: application of the Unified Theory of Acceptance and Use of Technology. HIM J. 2014; 43(3):23–28.

17. Kahouei M, Zadeh JM, Roghani PS. The evaluation of the compatibility of electronic patient record (EPR) system with nurses' management needs in a developing country. Int J Med Inform. 2015; 84(4):263–270.

18. Bhattacherjee A. Understanding information systems continuance: an expectation-confirmation model. MIS Q. 2001; 25(3):351–370.

19. Davis FD, Venkatesh V. Toward preprototype user acceptance testing of new information systems: implications for software project management. IEEE Trans Eng Manag. 2004; 51(1):31–46.

20. Larsen TJ, Sorebo AM, Sorebo O. The role of task-technology fit as users' motivation to continue information system use. Comput Human Behav. 2009; 25(3):778–784.

21. Beaudry A, Pinsonneault A. The other side of acceptance: studying the direct and indirect effects of emotions on information technology use. MIS Q. 2010; 34(4):689–710.

22. Jasperson JS, Carter PE, Zmud RW. A comprehensive conceptualization of post-adoptive behaviors associated with information technology enabled work systems. MIS Q. 2005; 29(3):525–557.

23. Palm JM, Dart T, Dupuis I, Leneveut L, Degoulet P. Clinical information system post-adoption evaluation at the georges pompidou university hospital. AMIA Annu Symp Proc. 2010; 2010:582–586.
24. Callen JL, Braithwaite J, Westbrook JI. Contextual implementation model: a framework for assisting clinical information system implementations. J Am Med Inform Assoc. 2008; 15(2):255–262.

25. Lin HC. Nurses' satisfaction with using nursing information systems from technology acceptance model and information systems success model perspectives: a reductionist approach. Comput Inform Nurs. 2016; 09. 09. DOI: 10.1097/CIN.0000000000000293.
26. Lapinsky SE, Holt D, Hallett D, Abdolell M, Adhikari NK. Survey of information technology in Intensive Care Units in Ontario, Canada. BMC Med Inform Decis Mak. 2008; 8:5.

27. Banner L, Olney CM. A step in the right direction: Electronic clinical documentation improves nurse charting, efficiency, and satisfaction. Comput Inform Nurs. 2007; 25(5):312–321.
28. Legris P, Ingham J, Collerette P. Why do people use information technology? A critical review of the technology acceptance model. Inf Manag. 2003; 40(3):191–204.

29. Tabibi J, Nasiripour AA, Kazemzadeh RB, Farhangi AA, Ebrahimi P. Effective factors on hospital information system acceptance: a confirmatory study in Iranian hospitals. Middle East J Sci Res. 2011; 9(1):95–101.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download