Abstract
Objectives
A patient accounting system is a subsystem of a hospital information system. This system like other information systems should be carefully designed to be able to meet users' requirements. The main aim of this research was to investigate users' requirements and to determine whether current patient accounting systems meet users' needs or not.
Methods
This was a survey study, and the participants were the users of six patient accounting systems used in 24 teaching hospitals. A stratified sampling method was used to select the participants (n = 216). The research instruments were a questionnaire and a checklist. The mean value of ≥3 showed the importance of each data element and the capability of the system.
In healthcare organizations, information is the foundation of decision-making, and it is essential for policy development, research, education and training, service delivery and financing. Diversity in healthcare activities is followed by different information needs of multiple users: policy-makers, managers, healthcare providers, etc. Therefore, information systems should be able to bring together all relevant partners to ensure that users of information have access to reliable, useable, understandable, and comparative data [1]. In fact, an important part of designing information systems is to understand users' requirements to increase efficiency, quality of work, and user satisfaction [2], and an information system which does not provide users with adequate information or does not have the necessary features is considered a weak system [3].
On the other hand, health information systems are very expensive. For example, in 2004, about 25.8 billion dollars were spent developing hospital information systems in the United States, and it was expected that this expenditure would lead to a significant improvement in healthcare quality and would increase the productivity and efficiency of healthcare organizations [4]. However, these systems were not able to meet users' requirements as expected, and this issue influenced justifying the investment made in this area. These problems were related to the inappropriate design of these systems [5].
In 2007, the American Hospital Association reported that only 6% of the hospitals in the United States were equipped with comprehensive hospital information systems. Some reasons for the reluctance of the hospitals to invest in information technology were a lack of fit between the systems' characteristics and users' requirements, a lack of data standards, and users' resistance towards using the technology [67]. Similarly, in developing countries, the literature [8] shows that the main reason for the failure of information systems in the healthcare sector is failure to meet managerial or operational needs. In these countries, translation of theoretical benefits into practice is difficult, and a number of contextual factors may influence these processes. Thus, even when ehealth technologies are successfully installed, the use of these technologies often faces challenges [9]. Therefore, system designers are responsible for obtaining a better understanding of users' needs to provide appropriate systems [6].
Currently, in Iran, a number of hospital information systems are used; however, due to the lack of national standards, various systems have been developed [10]. In addition, users' requirements have not been investigated in detail, and market criteria were considered in the development of the systems [11]. Investigating users' requirements and comparing their requirements with the systems' characteristics can help to identify the weaknesses of the systems, which can be improved in future versions.
One of the subsystems of current hospital information systems is the patient accounting system, which provides patients' billing information based on their medical records. This system is also very important for calculating hospital revenues and expenditures [12]. This system, like other information systems, should be carefully designed to be able to meet users' requirements, and to achieve this goal, it is necessary to involve users and improve it based on users' needs [13]. Therefore, the main aim of this research was to investigate users' requirements and to determine whether current patient accounting systems meet users' needs or not.
It is notable that despite the importance of the patient accounting system, few studies have been conducted in this area, and most of the studies related to accounting information systems have been completed in organizations other than hospitals and healthcare institutions. In addition, these studies have mainly focused on the factors influencing the success of accounting information systems in industry and not in healthcare [1415]. Therefore, it is expected that this study will contribute to knowledge related to the application of accounting information systems in healthcare organizations.
This was a survey study, and it was carried out in two phases. In the first phase, the information needs of system users who worked in 24 teaching hospitals were investigated. In the second phase, the results of the first phase were used to compare users' requirements with the characteristics of the patient accounting systems used in the above-mentioned hospitals (six systems). Before the research was conducted, the study was approved by the Institutional Review Board.
A stratified sampling method was used to select the participants of the study. In total, 216 potential participants were selected. In each hospital, nine participants were invited to take part in the study: four managers (hospital director, hospital manager, financial manager, and accounting manager) and five other employees (revenue department supervisor, two outpatient receptionists, and two inpatient receptionists).
In the first phase of the study, data were collected using a questionnaire. It was a 5-point Likert scale questionnaire, which was designed based on the literature [16171819], and the billing forms used in the teaching hospitals. It included a comprehensive set of data elements and features which might be required by the users. The questionnaire consisted of three parts (155 questions). Part 1 was related to a participant's personal information (7 questions). Part 2 was designed to investigate required data elements in an inpatient and outpatient accounting system (106 questions), and part 3 was related to required system features (42 questions). Part 2 included the following sections: patients' identification data, admission and discharge data, healthcare services data, healthcare provider's data, insurance data, patients' billing data, and traffic accident data.
The content validity of the questionnaire was checked by individuals who were experienced in the field of study. The reliability of the questionnaire was confirmed by calculating Cronbach's coefficient alpha (α = 0.95). The questionnaires were distributed to the system users and were collected after 2 weeks.
In the second phase of the study, a checklist was designed based on the results derived from the first phase. This means that after data analysis, some data elements and system features with mean values <3 were excluded, and the remaining items were used to form a checklist, which was regarded as a reference set. In the second phase, the items of the checklist were compared with the systems' characteristics. The face validity of the checklist was confirmed by the experts in the field.
The questionnaire items were measured on a 1–5 Likert scale as follows: very important (5), important (4), moderately important (3), of little importance (2), unimportant (1). The mean value of ≥3 showed the importance of each data element and system capability required by the participants. Therefore, the items with mean values <3 were not considered as important items and were excluded from the second part of the study. To compare users' views, the Mann-Whitney U test (α = 0.05) was used.
In the second phase of the study, a researcher (ZN) visited 6 teaching hospitals. The hospital information systems used in these hospitals were different and supported by different IT companies. The data related to the comparison between the users' requirements and the existing systems' characteristics were analyzed and reported using descriptive statistics.
In total, 153 participants responded to the questionnaire (70.83%). Among them, 38 participants were managers with the mean age of 42 years, and the highest frequency was related to men (n = 30; 81.1%). The mean age of the other users was 31.63 years, and the highest frequency was related to women (n = 73; 65.2%).
As data elements of a patient accounting system were different for inpatient and outpatient departments, the results of the study are reported separately for each of them.
The results showed that, among the patients' identification data and based on a 5-point Likert scale, the highest mean value was related to the patient's last name (3.56 ± 0.55), and the lowest mean value was related to the patient's occupation (2.47 ± 1.17). The admission and discharge data was the second group of data elements, among them the date of admission (3.39 ± 0.68), unique number of medical record (3.38 ± 0.62), and the date of death (3.33 ± 0.91) were reported as the most important data elements. The lowest mean value (2.90 ± 0.96) was related to the name of the medical center to which a patient was transferred.
The 'healthcare services data' was the next group of data elements in which the type of surgery (3.50 ± 0.68), the types of medical supplies used (3.45 ± 0.50), and the total cost of healthcare services/IRR. (3.41 ± 0.75) were found to be the most important ones. The lowest mean value was related to the patient's room number (2.69 ± 0.97).
The 'healthcare provider's data' was the fourth group of data elements with the highest mean value for the specialty of the healthcare provider (3.15 ± 0.87) and the lowest mean value (2.35 ± 1.34) for the provider's bank account number. In the next section, 'the insurance data', the highest mean value was related to the type of insurance (3.47 ± 0.66) and the insurance expiry date (3.47 ± 0.59), and the lowest mean value (2.74 ± 1.06) was related to the insurance representative's name.
Regarding 'patients' billing data' all data elements were important from the users' perspectives. In this section, the highest mean value (3.57 ± 2.50) was related to the total cost (in IRR), and the lowest mean value (3.13 ± 0.79) was related to the national ranking of the hospitals.
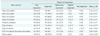
The last section was about 'traffic accident data'. In this section, most of the data elements were found to be important except the ICD-10 code for the cause of accident (2.98 ± 0.81) and the type of vehicle (2.83 ± 0.84). The highest mean value (3.34 ± 0.78) was related to the police report, and the lowest mean value (2.83 ± 0.84) was related to the type of vehicle (Table 1).
In the outpatients accounting system, most of the data elements were found to be important except the name of the employer (2.65 ± 1.12). Among the important data elements, the highest mean value (3.50 ± 0.64) was related to the name of the patient, and the lowest mean value (3.04 ± 0.91) was related to the age of the patient. To find out whether there was any difference between the perspectives of managers and other participants regarding the importance of data elements in the inpatient and outpatient accounting systems, the Mann-Whitney U test (α = 0.05) was used. The results showed that there was no significant difference between the perspectives of managers and other users in most areas of the study. However, their views were different regarding the importance of two items: the type of insurance to be included in an inpatient and outpatient accounting system, and the types of patients (emergency, inpatient, and outpatient) to be considered in an inpatient accounting system (Table 2).
As Table 2 shows, the above-mentioned data elements were less important from managers' perspectives.
All of the suggested features of the system were important to the participants. However, most of the participants (n = 138; 91.4%) believed that determining the access level for authorized users was the most important one (3.59 ± 1.63). The lowest mean value (3.03 ± 0.91) was related to updating a patient's sponsor data manually. No significant difference was found between the perspectives of managers and other participants regarding the importance of system features.
As mentioned before, six different hospital information systems were used in the settings of the study. To keep the names of the private IT companies confidential, the initials of their names have been reported in this study as follows: RA, TR, PSD, RR, KT, and FA.
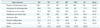
As Table 3 shows, among different groups of data in an inpatient accounting system, the highest mean value (88.38%) was related to healthcare services data, indicating that the highest fit between the users' requirements and systems' characteristics and the lowest mean value (23.79%) were related to traffic accident data. This indicates a gap between the users' information needs and the systems' characteristics. The highest degree of fit (80.83%) was found in the FA hospital information system, and the lowest degree of fit was related to the PSD hospital information system.
In the outpatient accounting system, the following degree of fit values between the users' information needs and the systems' data elements were found: the RA and RR hospital information system (100%), the TR, FA, and KT hospital information systems (95%), and the PSD hospital information system (90%). Regarding the systems' features, the results showed the following degree of fit values: the RR hospital information system (85.36%), the TR and FA hospital information systems (82.92%), the PSD hospital information system (80.5%), and the KT and RA (73.17%).
Financial information systems are the primary systems used in the hospitals to manage costs and to increase efficiency [20]. A patient accounting system is the subsystem of a hospital information system used for storing financial data, calculating healthcare costs, and providing patient billing information [21]. Since the process of financial data management influences a hospital's profitability cycle, it is necessary to use appropriate information systems to address users' requirements [8].
In the present study, users' requirements were investigated and compared with the characteristics of the existing patient accounting systems. The results showed that most of the suggested data elements and system's features were important to more than two-thirds of the participants (Figure 1). These findings are supported by other studies, in which, for example, patient identification data, admission and discharge data, and healthcare services data elements were found to be important for the subsystems of a hospital information system [212223].
In the current study, a national ID number was found to be an important data element, which has not been reported in other similar studies. Since precision is an important aspect of financial data management, healthcare organizations have to deal with precise data elements, such as the national ID number, to reduce the rate of errors. In particular, when patients' names are similar, the national ID number works as a unique code to recognize the right patient.
The results showed that among the insurance data, type of insurance, expiry date, and the name of the insurer were considered very important. In some hospital information systems, the patient accounting system is a part of the "admission and discharge system" or the "admission, discharge and transfer system", in which various sets of data, such as patients' identification data, admission and discharge data, patients' billing data, and insurance data, are considered necessary data elements [22]. The findings also showed that patients' billing data were the most important data compared to other data groups. These findings are in line with those of other studies [3], in which financial data are were found to be the most important data for hospital managers.
The importance of recording traffic accident data in a patient record has been acknowledged by other researchers [24]. Similarly, in the current study, traffic accident data were considered important to provide a precise record for insurers and to help calculate the direct costs resulting from traffic accidents.
The results also showed that all system features suggested in this research were important from users' perspectives. Among the system features, determining the access level of authorized users was the most important one, and users expected to be able to send patients' bills to insurance companies electronically. According to Vawdrey et al. [25], one of the most frustrating aspects of transition to an EHR system is the system's failure to support the existing electronic billing workflow. Moreover, because of poor system integration, it is difficult to identify the supporting documentation for each bill, and users have to manually manage both paper and electronic records. Since the patient accounting system is responsible for patient cost management and financial matters, the system features should be regularly updated based on users' requirements. This can help to meet users' expectations, and the process of cost control will be optimized.
As the research findings showed, the perspectives of mangers and other users were similar regarding the importance of data elements and system features. However, their opinions differed significantly regarding the importance of types of insurance and types of patients. These data elements were less important from managers' perspectives. Such a disagreement might be due to the practical experience of other users in communicating with insurance companies.
The study results also revealed that the highest degree of fit between the users' expectations and system's characteristics was related to the FA hospital information system, and the lowest degree of fit was related to the DPS hospital information system. It is notable that the FA hospital information resulted from using an in-house development approach, and this might be the reason users' expectations were met at a high level. Overall, the inpatient accounting systems investigated in this study were able to meet 70%–80% of user' expectations. The outpatient accounting systems were able to meet more than 90% of users' needs, and the system features showed a more than 70% fit with users' requirements. In another study, the degree of fit between an accounting system's characteristics and users' needs was reported as 65.4%, which shows the system's limitations [26]. Therefore, we can conclude that, although patient accounting systems are the oldest subsystems of hospital information systems, they may not be able to meet users' requirements completely, and there are still many opportunities to improve them.
In this study, due to resource and time constraints, only hospital information systems used in the teaching hospitals of one city were investigated. As a result the numbers of systems and system providers were limited. However, designing a comprehensive questionnaire for investigating users' requirements provided a relatively complete picture of what they needed and to what extent systems were able to meet their requirements. In addition, the current study focused on investigating the needed data elements and features of an ideal patient accounting system. Therefore, other areas of research, such as factors influencing the success of these systems were not studied.
In conclusion, prior to designing information systems, identifying users' requirements is necessary. The benefits of information system will not be achieved unless systems' characteristics and users' requirements can fit each other. The results of the present study showed that, although patient accounting systems are the oldest subsystem of hospital information systems, there are still some opportunities to improve them to meet users' requirements. As user involvement is an important part of the process of system design, the main users' of the system should be identified, and their requirements should be addressed properly. This will help to realize successful systems and to achieve the promised benefits of such systems.
Figures and Tables
Acknowledgments
This study was funded and supported by Tehran University of Medical Sciences (Grant No. 523).
References
1. Word Heath Organization. Heath information systems: toolkit on monitoring health systems strengthening [Internet]. Geneva, Switzerland: Word Heath Organization;2008. cited at 2015 Dec 20. Available from: http://www.who.int/healthinfo/statistics/toolkit_hss/EN_PDF_Toolkit_HSS_InformationSystems.pdf.
2. Maguire M, Bevan N. User requirements analysis: a review of supporting methods. In : Hammond J, Gross T, Wesson J, editors. Usability. New York (NY): Springer;2002. p. 133–148.
3. Dwivedi YK, Wastell D, Laumer S, Henriksen HZ, Myers MD, Bunker D, et al. Research on information systems failures and successes: status update and future directions. Inform Syst Front. 2015; 17(1):143–157.

4. Metfessel BA. Financial and clinical features of hospital information systems. In : Marcinko DE, Hertico HR, editors. Financial management strategies for hospitals and healthcare organizations: tools, techniques, checklists, and case studies. Boca Raton (FL): Taylor & Francis;2014.
5. Meyer R, Degoulet P, Omnes L. Impact of health care information technology on hospital productivity growth: a survey in 17 acute university hospitals. Stud Health Technol Inform. 2007; 129(Pt 1):203–207.
6. Hasri M, Zulkarnain MS, Ayoib CA, Norlida M. A study of user information satisfaction on financial management information system. Int Res J Finance Econ. 2010; (36):121–132.
7. Bhattacherjee A, Hikmet N, Menachemi N, Kayhan VO, Brooks RG. The differential performance effects of healthcare information technology adoption. Inform Syst Manag. 2006; 24(1):5–14.

8. Hammad SA, Jusoh R, Oon E. Management accounting system for hospitals: a research framework. Ind Manag Data Syst. 2010; 110(5):762–784.

9. Cohen JF, Coleman E, Abrahams L. Use and impacts of e-health within community health facilities in developing countries: a systematic literature review. In : Proceedings of the 23rd European Conference on Information Systems (ECIS); 2015 May 26-29; Munster, Germany.
10. Ayatollahi H, Mirani N, Haghani H. Electronic health records: what are the most important barriers? Perspect Health Inf Manag. 2014; 11:1c.
11. Riazi H. History of electronic medical records in Iran. Tehran: Ministry of Health and Medical Education, Statistical and Information Technology Office;2010.
12. BE Software Solution. Hospital information systems [Internet]. Hounslow, UK: BE Software Solution;2006. cited at 2015 Dec 20. Available from: http://www.besoftware.co.uk/products-services/hospital-informations.html.
13. Hadianfard A. The survey of hospital information system structure in Shiraz hospitals [dissertation]. Tehran: Shahid Beheshti University of Medical Sciences;2002.
14. Al-Qudah G. The impact of accounting information systems on effectiveness of internal control in Jordanian commercial banks "Field Study". Interdiscip J Contemp Res Bus. 2011; 2(9):365–372.
15. Sajady H, Dastgir M, Nejad HH. Evaluation of the effectiveness of accounting information systems. Int J Inform Sci Manag. 2008; 6(2):49–59.
16. Riazi H, Fathi B, Bitaraf A. Hospital information system. Tehran: Ministry of Health and Medical Education, Statistical and Information Technology Office;2006.
17. Statistical and Information Technology Office. Evaluation framework for hospital information systems. Tehran: Ministry of Health and Medical Education, Statistical and Information Technology Office;2011.
18. Avelino JN, Hebron CT, Laranang AL, Paje PN, Flodalyn Bautista MM, Caro JD. Requirements gathering as an essential process in customizing Health Information Systems for small scale health care facilities. In : Proceedings of the 5th International Conference on Information, Intelligence, Systems and Applications (IISA); 2014 Jul 7-9; Chania, Greece. p. 184–189.
19. Riazi H, Bitaraf A, Fathi B. Electronic Health Record: concepts, standards and development methods. Tehran: Ministry of Health and Medical Education, Statistical and Information Technology Office;2011.
20. Borzekowski R. Measuring the cost impact of hospital information systems: 1987-1994. J Health Econ. 2009; 28(5):938–949.

21. Hosseini A. Designing a conceptual model of hospital information systems for hospitals affiliated with universities of medical sciences in Tehran [dissertation]. Tehran: Iran University of Medical Sciences;2006.
22. Babaie R. A study on the electronic health records of dialysis patients [dissertation]. Tehran: Tehran University of Medical Sciences;2011.
23. Levy S, Heyes B. Information systems that support effective clinical decision making. Nurs Manag (Harrow). 2012; 19(7):20–22.

24. Kahouie M. Designing of emergency information system (EIS) logical schema for Iran [dissertation]. Tehran: Iran University of Medical Sciences;2010.
25. Vawdrey DK, Walsh C, Stetson PD. An integrated billing application to streamline clinician workflow. AMIA Annu Symp Proc. 2014; 2014:1141–1149.
26. Farzandipour M, Sadoughi F, Meidani Z. Hospital information systems user needs analysis: a vendor survey. J Health Inform Dev Ctries. 2011; 5(1):147–154.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download