Abstract
Objectives
This study analyzed the incidence and characteristics of in-hospital cardiac arrest (IHCA) in Korea based on a sample group of patients that is representative of the population.
Methods
The incidence of IHCA in adults was extracted from HIRA-NIS-2009, a sample of all patients using medical services in Korea. IHCA patients were analyzed according to gender, age, type of medical institute, and classification under the 6th revision of the Korean Standard Classification of Diseases (KCD-6). In addition, to assess the differences arising from the size of medical institutes, the IHCA incidence was analyzed in relation to the number of inpatient beds.
Results
Based on the sample data, the total incidence of IHCA in Korea was found to be 2.46 per 1,000 admissions (95% confidence interval [CI], 2.37–2.55). A higher incidence was found among men at 3.18 (95% CI, 3.03–3.33), compared to women at 1.84 (95% CI, 1.74–1.94). The incidence of IHCA was also higher in hospitals that had more than 600 inpatients beds at 5.40 (95% CI, 5.16–5.66) in comparison to those that had less than 600 inpatients beds at 4.09 (95% CI, 3.76–4.36) (p < 0.001). By primary disease, the incidence was the highest for infectious diseases.
In-hospital cardiac arrest (IHCA) is a major cause of death among patients [12]. Extensive research has been performed regarding out-of-hospital cardiac arrest (OHCA) [34], and efforts to improve prognosis have led to a dramatic increase in survival [5]. However, IHCA has not been widely studied, and even basic data, such as incidence, has only been covered in a few reports. Previously, the IHCA incidence of elderly patients was analyzed using Medicare data [67], and that of adults was based on the United Kingdom National Cardiac Arrest Audit database [8]. Another study compared the incidence rates of IHCA and OHCA in specific hospitals in the United Kingdom [9]. The IHCA incidence rates in Australia and New Zealand were found [10]. In Korea, research has been limited to a small number of hospitals [1112]. To date, the incidence of IHCA has not been studied using a national representative sample.
From 1977, Korea has started to partially adopt medical insurance and gradually widened the limit of applications. In 2000, medical insurance was integrated into the National Health Insurance Service (NHIS). All people who resided in Korea were provided with a fee-for-service system by a single healthcare agent, the NHIS. Every detail about the medical treatment, medication, and diagnosis of all patients was coded, and then input to the Health Insurance Review and Assessment Services (HIRA) [131415]. In May 2012, the National In-patients Sample (NIS) data of about 13% of the in-patients and 1% of outpatients with national representativeness from the year 2009, named HIRA-NIS-2009, was provided [1617]. HIRA-NIS-2009 was extracted by stratified and systematic sampling methods according to gender and age group among all patients who used medical services in 2009. It included every detail of the medical treatments and medications of the sample patients. The representativeness of the HIRA-NIS-2009 was verified by HIRA and five other medical associations in Korea [17].
Before national insurance claims were accessed, a pilot study was performed to check whether the IHCA incidence could be obtained by analyzing HIRA-NIS-2009, which was verified to have national representativeness. This study is the first to examine IHCA incidence among hospitalized patients in Korea, and it is the only one of its kind involving a national representative sample.
HIRA-NIS-2009 consists of five tables, each with a unique key, called a KEYCODE. TABLE20 provides basic information on patients (unique identification number of HIRA-NIS-2009, age, gender, institution number, department, total costs, KEYCODE, etc.), while TABLE30 contains detailed medical claim data (procedure, surgery, medical supply, or drug identification code, price, counts, KEYCODE, etc.). TABLE40 gives the disease code, while TABLE53 contains details of drug prescriptions. Finally, TABLE YKIHO is the table for institutional information (institution number, classification code of the institute, inpatient bed numbers of the institute, computerized tomography availability, magnetic resonance imaging availability, etc.).
HIRA-NIS-2009 contains about 13% of the in-patient data and 1% of outpatient data of all patients who used medical services from January1, 2009 to December 31, 2009.
To pick out IHCA patients from HIRA-NPS-2009-001, key values corresponding to claim codes for cardiopulmonary resuscitation (CPR) were extracted from TABLE30. The claim codes include M5873, M5874, M5875, M5876, and M5877.
In-patient cases of tertiary-care hospitals, secondary-care hospitals, hospitals, geriatric hospitals, and clinics was extracted from TABLE20. From this procedure, basic patient information was obtained from TABLE20 for the identified IHCA patients.
Cases extracted from TABLE20 and TABLE30 through the above two steps were joined and IHCA cases were finally extracted.
Since Korea's health insurance considers hospitalization as more than 6 hours since admission to the emergency departments, OHCA patients who did not recover or died shortly after recovery were mostly excluded. This would minimize confusion over OHCA. However, some may have been included as the proportion of patients admitted after surviving OHCA is approximately 5.7% [20].
From TABLE30, cases with very few claim codes other than those for CPR were excluded from the count as they were unlikely among hospitalized patients.
Among the cases classified as IHCA, the patients were analyzed according to gender, age, type of medical institute, and primary diagnosis classified under the 6th revision of the Korean Standard Classification of Diseases (KCD-6). In addition, to assess the differences arising from the size of medical institutes, the IHCA incidence was analyzed in relation to the number of inpatient beds.
Using the disease codes of KCD-6, the frequency of diagnosis was analyzed for patients with prescriptions for CPR. To determine differences in IHCA incidence arising from the number of inpatient beds, tertiary and secondary-care hospitals were categorized into hospitals with more than 600 beds and those with less than 600. The number of hospitalizations and IHCA incidence were then compared. There were only two tertiary hospitals with less than 600 beds, and secondary-care hospitals with more than 600 beds were considered as being closer to tertiary hospitals.
Fischer exact test was employed, and a p-value less than 0.05 was regarded as statistically significant. All of the calculations were performed in SAS ver. 9.4 (SAS Institute, Cary, NC, USA).
In the sample data of HIRA-NIS-2009-001, there were 3,393 cases with insurance claim codes corresponding to CPR (M5873–5877) among the 1,212,982 inpatients. Out of these cases, 2,978 were finally considered to be IHCA patients.
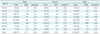
Based on the sample data, the total incidence of IHCA in Korea was found to be 2.46 per 1,000 admissions (95% confidence interval [CI], 2.37–2.55). A higher incidence was found among men at 3.18 (95% CI, 3.03–3.33) compared to women at 1.84 (95% CI, 1.74–1.94). By age group, the highest incidence was observed among patients aged 80–89 at 5.19. Men aged 90 and above had the highest incidence of 8.90, while women aged 80–89 recorded 4.25 (Table 1).
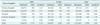
By medical institute, the incidence of IHCA in tertiary-care hospitals was the highest at 5.17, followed by secondary-care hospitals at 4.76, geriatric hospitals at 1.18, hospitals at 0.99, and clinics at 0.03 (Table 2).
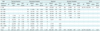
Patients diagnosed as suffering from certain infectious and parasitic diseases (A00–B99) as defined in KCD-6 had the highest incidence of 10.87. This was followed by diseases of the respiratory system (J00–J99) at 7.25, and diseases of the circulatory system (I00–I99) at 5.30 (Table 3).
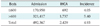
Excluding hospitals with a low incidence of IHCA, long-term-care hospitals and clinics, tertiary and secondary-care hospitals combined were categorized into hospitals with more than 600 beds and those with less than 600. The number of admissions and IHCA incidence were then compared. The incidence was 4.09 (95% CI, 3.76–4.36) for hospitals with less than 600 beds, and 5.40 (95% CI, 5.16–5.66) for those with more than 600 beds, indicating a significant difference in IHCA incidence between the two hospital groups (p < 0.001) (Tables 4, 5).
There are very few countries with a national insurance policy provided by a single insurer. Korea has a special system in which medical claims are made to the NHIS based on the resident registration number of each citizen [1314]. The health insurance claim data contains extensive information on the use of medical services, but it may be distorted in order to receive more compensation [15]. The scale of data also makes it difficult to identify the desired clinical data for analysis. HIRA-NIS-2009, verified as having national representativeness, was obtained from the health insurance claims of 2009 [171819], and it is being used in some studies [15]. Based on HIRA-NIS-2009, this study found that the incidence of IHCA was 2.46 per 1,000 admissions. Since most countries do not have data on the use of medical services by all citizens, research on the IHCA incidence has been mostly limited to certain age groups or a few hospitals. Such studies have been carried out based on data provided by the Medicare Provider Analysis and Review (MedPAR) [7], the United States National Registry of Cardiopulmonary Resuscitation (NRCPR) [6], and the United Kingdom National Cardiac Arrest Audit (NCAA) [8].
Recently, an NCAA audit report found that there were 1.6 IHCA patients per 1,000 admissions in 144 hospitals [8]. This is significantly different from the incidence reported in the present study. In a review on hospitals in Australia and New Zealand, the IHCA incidence ranged from 1.31–6.11 per 1,000 admissions in four population studies, and 0.58–4.59 in 16 cohort studies from 1964 to 2014 [10]. This study showed a difference in IHCA between hospitals with a rapid response system and those without [10].
The incidence reported by the study based on MedPAR insurance claims of patients aged 65 and older was 2.73 per 1,000 admissions, which is similar to the results of this study [7]. The study based on NRCPR found 14,720 cases of IHCA in a year among 287 hospitals in the United States, or 0.175 cases/bed [6].
Age was found to be an important variable in IHCA incidence. The higher the age, the greater the incidence of IHCA. The higher incidence in the 80–89 age group compared to the 90 or older age group can be traced to other factors, such as severity of disease and DNAR (do not attempt resuscitation) orders.
Previous research found gender did not have any significant influence on IHCA incidence [67]. However, in this study, a higher incidence was found among men at 3.18 per 1,000 admissions (59.47%), compared to women at 1.84. This is similar to the results of a Korea-based study on OHCA that excluded cases associated with non-cardiac reasons, where men accounted for 58.9% and women for 41.1% [20]. In the NCAA report, men accounted for 57.2% of all IHCA cases, which is consistent with the findings of the present study [8]. The variation in results can be traced to differences in average life span, gender differences in use of medical services, and causes of cardiac arrest.
The incidence of IHCA also differed according to the size of hospitals, or more specifically, the number of inpatient beds. A US study based on NRCPR data reported a lower incidence of cardiac arrest in hospitals with more than 500 beds [6], whereas this study found a higher IHCA incidence in hospitals with more than 600 beds. This reflects Koreans' preference for major hospitals, which have more inpatient beds, when seeking treatment for diseases with high severity.
The incidence of IHCA in tertiary-care hospitals and secondary-care hospitals was 4 to 5 times the incidence in hospitals and long-term-care hospitals. This can be explained by the higher proportion of critical patients among the hospitalized patients in tertiary-care hospitals and secondary-care hospitals. The slightly higher incidence in long-term-care hospitals over hospitals is due to patients being older and at the end stage of life.
Further research is needed because the differences may have resulted from the hospital's response to cardiac arrest, the medical staff 's level of training on basic and advanced life support, and the availability of the medical emergency teams (MET) and rapid response teams (RRT) [212223].
In previous research, the primary diseases suffered by patients before cardiac arrest were myocardial infarction (36%), respiratory failure (35%), heart failure (34%), arrhythmia (29%), renal failure (29%), diabetes (28%), and infection (24%) [6]. More patients were admitted for conditions associated with internal medicine than for external injuries or surgical problems [7]. In this study, the primary diseases of IHCA were in the order of infection, respiratory, and circulatory, indicating that patients had experienced similar primary diseases before IHCA. The United States has a smaller proportion of IHCA patients with infections because CPR is not required for progressive septic shock-induced cardiac arrest under the guidelines of the American Heart Association [24], whereas it is frequently performed in Korea.
With more than half of OHCA patients suffering from circulatory diseases [25], it is evident that different approaches are needed for IHCA and OHCA. In a study aimed at improving the survival rate of IHCA, which was limited to a single domestic hospital, some possible solutions mentioned were training in basic and advanced life support, CPR by experienced medical staff, and MET utilization [12].
This study, based on health insurance claim data, had the following limitations: first, the health insurance claims only contained coded titles of diagnosis, procedures, surgery, and drug administration, but not the detailed responses and test results. An in-depth examination of the causes behind cardiac arrest was not possible. Second, the condition of patients at the time of cardiac arrest could not be determined without access to medical records. Third, the state of patients at the time of transfer, return, and discharge was not available as health insurance claim data only classified treatment results as continued, transfer, return, death, discharge, or other. Analysis using the Cerebral Performance Categories Scale [2627], which is needed in the prognosis evaluation of IHCA patients, could not be performed. Fourth, patients and hospitals were anonymous. Analysis according to seasonal/annual/regional characteristics and institutional characteristics could not be performed.
In conclusion, using health insurance claim data of HIRA-NIS-2009, this study found an IHCA incidence of 2.46 per 1,000 admissions among adults hospitalized in 2009. The results of this study, based on data having national representativeness, are expected to serve as a valuable reference in the multi-faceted analysis of IHCA. In addition, various indicators, such as MET, RRT system enhancement, IHCA prevention, and improvement of survival rate can be derived by comparing the total incidence of IHCA and the incidence at each hospital.
Figures and Tables
Acknowledgments
We used the HIRA-NIS-2009 data that the Health Insurance Review and Assessment Service (HIRA) provided but declare that the results do not in any way reflect the positions of either HIRA or the Ministry of Health and Welfare of the Republic of Korea.
The results of this work were included in the thesis for the Master of Medicine by Yuri Choi of the Graduate School of Dong-A University.
This work was supported by the Dong-A University research fund.
References
1. Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007; 33(2):237–245.

2. Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, et al. Heart disease and stroke statistics: 2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006; 113(6):e85–e151.
3. Bagai A, McNally BF, Al-Khatib SM, Myers JB, Kim S, Karlsson L, et al. Temporal differences in out-of-hospital cardiac arrest incidence and survival. Circulation. 2013; 128(24):2595–2602.

4. Song KJ, Oh DJ. Current status of CPR in Korea. Korean J Med. 2007; 73(1):4–10.
5. Rea TD, Page RL. Community approaches to improve resuscitation after out-of-hospital sudden cardiac arrest. Circulation. 2010; 121(9):1134–1140.

6. Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003; 58(3):297–308.

7. Ehlenbach WJ, Barnato AE, Curtis JR, Kreuter W, Koepsell TD, Deyo RA, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009; 361(1):22–31.

8. Nolan JP, Soar J, Smith GB, Gwinnutt C, Parrott F, Power S, et al. Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation. 2014; 85(8):987–992.

9. Tunstall-Pedoe H, Bailey L, Chamberlain DA, Marsden AK, Ward ME, Zideman DA. Survey of 3765 cardiopulmonary resuscitations in British hospitals (the BRESUS Study): methods and overall results. BMJ. 1992; 304(6838):1347–1351.

10. Fennessy G, Hilton A, Radford S, Bellomo R, Jones D. The epidemiology of in-hospital cardiac arrests in Australia and New Zealand. Intern Med J. 2016; 02. 10. [Epub]. DOI: 10.1111/imj.13039.

11. Chon GR, Lee J, Shin Y, Huh JW, Lim CM, Koh Y, et al. Clinical outcomes of witnessed and monitored cases of in-hospital cardiac arrest in the general ward of a university hospital in Korea. Respir Care. 2013; 58(11):1937–1944.

12. Shin TG, Jo IJ, Song HG, Sim MS, Song KJ. Improving survival rate of patients with in-hospital cardiac arrest: five years of experience in a single center in Korea. J Korean Med Sci. 2012; 27(2):146–152.

13. Jeong HS. Designing an effective pay-for-performance system in the Korean National Health Insurance. J Prev Med Public Health. 2012; 45(3):127–136.

14. Jeong HS. Korea's National Health Insurance: lessons from the past three decades. Health Aff (Millwood). 2011; 30(1):136–144.
15. Kim KH, Kwon IH, Lee JY, Yeo WH, Park HY, Park KH, et al. Clinical significance of national patients sample analysis: factors affecting mortality and length of stay of organophosphate and carbamate poisoned patients. Healthc Inform Res. 2013; 19(4):278–285.

16. Park YT, Yoon JS, Speedie SM, Yoon H, Lee J. Health insurance claim review using information technologies. Healthc Inform Res. 2012; 18(3):215–224.

17. Kim RY. Introduction of Health Insurance Review and Assessment Services' National Patients Sample. HIRA Policy Trend. 2012; 6(5):37–47.
18. Chun CB, Kim SY, Lee JY, Lee SY. Republic of Korea: health system review. Health Syst Transit. 2009; 11(7):1–184.
19. Song YJ. The South Korean health care system. Japan Med Assoc J (JMAJ). 2009; 52(3):206–209.
20. Cho H, Moon S, Park SJ, Han G, Park JH, Lee H, et al. Out-of-hospital cardiac arrest: incidence, process of care, and outcomes in an urban city, Korea. Clin Exp Emerg Med. 2014; 1(2):94–100.

21. Sorensen EM, Petersen JA. Performance of the efferent limb of a rapid response system: an observational study of medical emergency team calls. Scand J Trauma Resusc Emerg Med. 2015; 23:69.

22. Hodgetts TJ, Kenward G, Vlackonikolis I, Payne S, Castle N, Crouch R, et al. Incidence, location and reasons for avoidable in-hospital cardiac arrest in a district general hospital. Resuscitation. 2002; 54(2):115–123.

23. Sandroni C, Ferro G, Santangelo S, Tortora F, Mistura L, Cavallaro F, et al. In-hospital cardiac arrest: survival depends mainly on the effectiveness of the emergency response. Resuscitation. 2004; 62(3):291–297.

24. ECC Committee, Subcommittees and Task Forces of the American Heart Association. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005; 112:24 Suppl. IV1–IV203.
25. Bayes de Luna A, Coumel P, Leclercq JF. Ambulatory sudden cardiac death: mechanisms of production of fatal arrhythmia on the basis of data from 157 cases. Am Heart J. 1989; 117(1):151–159.

26. Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style: a statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991; 84(2):960–975.

27. Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa). Resuscitation. 2004; 63(3):233–249.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download