Abstract
Objectives
The purpose of this study was to review the current telemedicine of the Korea and the telemedicine of the other countries.
Methods
This study reviewed several documents on telemedicine and summarized the documents on the initiation of the telemedicine of the Korea, the recent regulations of the government, the analytical research results, and the telemedicine of foreign countries.
Results
One of recent demonstration trials of telemedicine began in July 2015 in the Korea. The plan was to conduct an emergency telemedical treatment trial among the cooperative medical service centers until the end of February 2016. No telemedical services were provided at the level of local primary care clinics, and there was 1.2% provision at the hospital level. The Europe Union and the United States had more active telemedical services in comparison to the Korea.
Demonstration trials using information and communication technology (ICT) for a variety of purposes, such as telemedicine, have expanded in line with increases in the aging population and chronic diseases as health issues have become an urgent concern of policy makers. Telemedicine is particularly necessary for citizens living in low medical service areas, such as islands and mountainous regions in the Korea. Telemedicine is also suitable for areas where the internet is available and citizens have mobile phones [1]. The adoption rates of Electronic Medical Record systems in the Korea medical centers are 100% at tertiary hospitals, 99% at general hospitals, 95.4% at local hospitals, and 91.9% at local primary care clinics [2]. Health and medical professionals are expecting that advances in ICT will lead to the further development of telemedicine [3].
Worldwide, there is a strong interest in telemedicine. Developed countries have a desire to provide high-quality health services for citizens living in remote rural or island areas, while developing countries wish to use limited medical infrastructures more effectively [4].
Telemedicine services between doctor and patient have been tried to assess clinical safety, effectiveness, and usefulness (satisfaction) [5]. Telemedicine has been proven particularly effective in psychological treatments of mental health and anxiety disorders as well as the home monitoring of certain diseases (cardiovascular and respiratory diseases) [5]. Although there are successes and potential advantages in advanced or developing countries regarding the broader aspects, the medical effectiveness and economical advantages of telemedicine have not been proven, so that it is still in the trial stage [67].
Difficulties in accessing necessary services due to increases in chronic diseases and the continuous increase in service management costs indicate that telemedicine could be a very useful tool. Studies have suggested that telemedicine may be effective for prevention, diagnosis, treatment, and rehabilitation as well as the fact that it is cost-effective [8]. The vitalization of telemedicine alongside other developments in the medical sector will have a large impact on the convenience of medical services and the improvement of public health. There is a lack of studies on the current status of telemedicine and its progress in the Korea in relation to the international community. Therefore, the purpose of this study was to review the recent telemedicine trial conducted by the government to promote telemedicine in the Korea and consider it in relation to the telemedicine systems of other countries.
This study reviewed several documents on telemedicine and summarized the documents on the initiation of the telemedicine of the Korea, the recent regulations of the government, the analytical research results, and the telemedicine of foreign countries.
The initiation of telemedicine is regarded as the transfer of electrocardiograph data through the telephone line at the beginning of the 20th century [3]. The discussion of telemedicine in Korea began with a demonstrative project on remote diagnostic imaging between Seoul National University (SNU) Hospital and Yeoncheon County Health Center in 1988. The next telemedicine trial began in October 1990 among three university hospitals (SNU Hospital, Hallym University, and Kyungpook National University Hospital) and three govern mental health centers (Yeoncheon, Hwacheon, Uljin). However, it came to a halt due to technical issues, including transfer speed, after a year.
As part of the national competitiveness policy based on the establishment of super-high-speed information communications network lines, telemedical diagnosis and medical examination by interview was introduced by tertiary hospitals (Kyungpook National University Hospital and Chonnam National University Hospital) and local medical centers in areas with low medical services (Uljin, Gurye) using the public communication network (public switched telephone network [PSTN]) in March 1993 for one year. However, there was no further development due to the information technology of the time, the social environment, and the inadequacy of the legal system. Since then, research and the introduction of telemedicine in visiting home nursing healthcare, health counseling, and health management were tried by SNU Hospital, Yonsei University Severance Hospital, and hospitals of the Catholic University, although most were completed at a project level [1].
The Korea revised the Medical Law in March 2002 and built the legal grounds for providing telemedicine services [5]. The revised Medical Law did not limit telemedicine to remote areas but included the aged with chronic diseases and the disabled for the provision of telemedicine services between patients and doctors. The prerequisite condition is that the doctor must face the patient for an initial consultation and then use telemedicine ICT to monitor (medical devices attached to the patient or observation of bedsores) the patient's pathogenesis and regular meetings with the patient [1].
The government could implement various demonstration trials based on other acts. The Base Act on Health and Medical Service Section 44 states that "the nation and the local government can begin the trial business in order to conduct various initiatives if they necessitate to test governmental programs on the health and medical system" [9]. Telemedicine demonstration trials have begun in various governmental sectors since the 1990s based on this act. One of the trials began in 2014 with the aim of strengthening the health of chronic patients, the elderly, and the disabled by overcoming the inconvenience of conventional health services for citizens living on islands and in other remote areas.
Expectations regarding telemedicine have risen, and some local hospitals or health centers have begun to provide services within the boundaries of the law with no legal restrictions since then. At the time, telemedicine was not discussed as a new health management or medical provision paradigm; rather, discussions centered on the technology that provides telemedicine and on service provision tools at the industrial level [10].
Telemedicine related businesses in the private sector include: the blood sugar management service by KT Corp., 'Touch Dr.' by LG CNS, the unconstrained biological signal measurement laboratory business of SNU, 'DreamCare TV' (consortium process with KT Corp., Bit Computer Inc., Gachon University Gil Medical Center, Samsung Electronics), 'TV Doctor' service (a model business by LG Dacom and Health Insurance Review and Assessment Service), and 'u-Chronic Care' (SNU Bundang Hospital, Yonsei University Severance Hospital). However, these are not nationwide programs, nor is there a systemized businesses model [1]. Since revising the Medical Law of 2013, the Korea government is now expanding its demonstration trial into various contexts, such as military camps, trans-Atlantic boats, and Korean private hospitals run in four international regions (Iraq, the United Arab Emirates, North Africa, and Latin America) in 2015.
There is little data for the current analysis of telemedicine services in Korea despite the internal and external interests in telemedicine. The implementation of telemedicine was 0.1% according a survey conducted by the Health Insurance Review and Assessment Service in 2013-2014. There were no telemedicine services offered at the primary care clinic level, and there was 1.2% provision at the hospital level [2] (Table 1).
One of the most recent demonstration trials of telemedicine began in July 2015 in the Korea, which was to provide telemedicine services to areas with low medical services [11]. The Korean government announced that emergency telemedicine cooperation treatment (ETCT) trial among the medical centres in low medical service areas will be conducted around these health centres until the end of February 2016. ETCT here refers to the action of receiving advice when doctors are faced with emergency patients in rural areas and they require and request support regarding treatment methods and transferability from their host hospitals in urban areas.
The participants are designated medical centers approved by the Minister of Health and Welfare, who are willing to participate and have signed the cooperative treatment contract with the partnering centers. The first purpose of the trial is to assess the validity of the program and the potential to expand application of the national health insurance fee model to establish a systemic foundation. A second purpose is for medical insurance to compensate the treatment costs incurred by emergency patients requiring appropriate treatment or quick transfer so that ETCT will be utilized more. In this way, the quality of medical services may be improved by the introduction of ETCT medical fee by health professionals [12].
The European Union (EU) has perceived telemedicine service expansion to be a very important area. With the increases in chronic diseases and rising medical expenditures, the effective use of the limited medical resources is particularly with an aging population [13]. It is common for chronic diseases to develop complications, so it is not appropriate to respond to them in the same way as for acute diseases that can be treated completely. Therefore, many countries are using a variety of disease management programs (DMPs) [1]. Several trials of DMPs were conducted in Germany in the late 1990s, and one of the programs was patient monitoring through telemedicine [1415]. Telehealth systems were provided in 31% of hospitals and 15% of clinics (based on doctor-patient consultation) according to research on telemedicine in the EU in 2012 [1617].
Telemedicine began in the United States to provide effective medical services to citizens in the vast land and remote areas [4]. Super-high-speed communication networks (SCN) were expanded nationwide under the Clinton administration, and telemedicine began to grow as a derivative part of SCN businesses.
The American Telemedicine Association was established in 1993, and the Health Insurance Portability and Accountability Act 1996 (HIPPA) was enacted in 1996 to allow the use of medical information. This legislation was made for the first time in the world, and it is the most comprehensive telemedicine law, which other states have been using as their model [5].
The Accountable Care Organization (ACO) of the Obama administration is the organization responsible for providing all medical services. University hospitals, clinics, doctors, and nursing homes are integrated into one group in the operation dimension and provide all medical services, such as high-level surgery, treat minor illnesses and provide telemedicine to patients [1]. In other words, service provision is not just face-to-face doctor and patient consultation; rather, treatments and consultations are provided through telemedicine using the internet and HIT technologies. A variety of providers participating in the ACO connect through HIT to share information and assess the level of the group and performance to reduce the duplication of treatments and tests to increase the quality of care and reduce costs.
Various demonstration trials in relation to telemedicine are in progress as projects in consortiums composed of state govern ments, universities, and companies in the United States. There are many known projects, and one example is a 2-year project to introduce medical body area networks (MBANs) conducted by the Federal Communications Commission (FCC). For MBAN, a separate mobile-frequency is designated to link medical equipment for monitoring a patient's condition more effectively. It is expected to provide a quick and convenient telemedicine treatment, including patient examination, prescription, and treatment. The introduction of MBAN means that data regarding the current condition of the patient with attached sensors is transferred to the doctor remotely. The doctor can check the health status of a patient at home, in a hospital, or anywhere. The FCC maintains that telemedicine using mobile equipment will allow a quick diagnosis and a response to provide more effective telemedicine treatments [18].
The basic principles of telemedicine and the appropriate recipients for telemedical services were first identified by the Department of Health and Human Services in Japan in December 1997. The principles were partially revised in 2011, and they now provide the basic guidelines for the implementation of telemedicine. Japanese telemedicine is divided into two categories: 1) between hospitals (doctor-to-doctor) and 2) between hospital and patient (doctor-to-patient) [5].
The limits are clearly defined for doctor-to-patient telemedicine. The telemedicine target patients are home patients requiring oxygen intake and people with incurable diseases, diabetes, high blood pressure, atopic dermatitis, and/or bedsores. First, acute patients must be treated by direct meeting with medical doctors. Only in situations in which conducting a face-to-face consultation or continuous treatment of chronic patients over a long time or when a patient's long-term care is proven to be improved, telemedicine treatment in combination with direct treatment can be conducted.
Japan uses telemedicine as a complement to face-to-face treatment. Medical insurance does not accept the prevention and health consultation claims of doctor-to-patient telemedicine except when the medical quality was proven to be improved through medical data [5]. A study found that 12.5% of hospitals with more than 400 inpatient beds use telemedicine for teleradiology diagnoses, 6.1% for telepathology, and 1.3% for home patients. The usage rate of small hospitals and clinics was 1% [13].
There are no more recent utilization statistics. Japanese telemedicine developed since the late 1990s, but it is difficult to say that it is actively being developed [5]. Hasegawa [19] suggested that the reasons are the lack of policy promotion and clinical research, as well as application problems for coverage by medical insurance.
This study reviewed the current state of telemedicine trials in the Korea and researched the adoption of telemedicine in other countries. Telemedicine is a very useful tool for providing high-quality medical services to low medical service areas for home care or preventative healthcare as well [1]. However, there are many issues to be resolved for the promotion of telemedicine in the Korea. First, there is a discrepancy in telemedicine establishment in different areas. Seoul has a well established medical infrastructure in comparison to remote areas such as Gangwon Province. Political support is required to establish telemedicine well in accordance with the features of various areas requiring telemedicine [20]. Secondly, the Korea has not established telemedicine law. It is partially mentioned in various sections of the current acts and laws. Therefore, telemedicine legislation needs to be enacted through societal agreement. Thirdly, the cost-effectiveness of telemedicine needs to be proven through research. Overall satisfaction was 77% for the telemedicine trial analysis of 5 health centers and 4 clinics conducted in September 2014 [9]. The analysis of the trial cases demonstrated that there were positive changes in patients' lifestyles for the management of the chronic diseases. However, there has been little discussion of the cost-effectiveness of domestic telemedicine. Fourth, there is a lack of standards regarding medical data and information and communication technologies, and this hinders the promotion of telemedicine [21]. For example, the support policy varies due to different implementations of telemedicine by the Ministry of Health and Welfare, the Ministry of Trade, Industry and Energy, and military camps of the Ministry of Defence in Gangwon Province [9]. Finally, ethical issues related to telemedicine should be considered so that human rights, privacy, and confidentiality of patients are legally protected. Telemedicine should be implemented under the legal guidelines of equity on accessing patients' data, maintianing human ethics, and respecting the dignity of man [1].
Telemedicine in line with the development of the information technology and health and medical technology can remove the limits of space and time to reduce the cost and time required to provide convenient services to patients. The effect is expected from the combination of the current medical provision system for convenience, improvement of medical service quality in remote areas and effectiveness of medical services to patients [3].
Figures and Tables
Table 1
Telemedicine introduction by hospital type
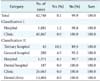
Adapted from the first author of the original study [2].
References
1. Lee KS. Theory of health policy. Seoul, Korea: Gyechuk;2015.
2. Park YT, Lee PH, Kim HS, Kim UN, Kang SJ, Han KS, et al. Survey on current status of the healthcare information and communication technology in Korea. Seoul, Korea: Health Insurance Review & Assessment Service;2014.
3. World Health Organization. Telemedicine in member states: opportunities and developments. Geneva, Switzerland: World Health Organization;2010.
4. Yoon YH. Enhance issues of the global competitiveness of telemedicine industry in Korea. Int Commer Inf Rev. 2011; 13(3):325–351.
5. Kim DJ. Tele-health around the world: history, current status, and implications. Sejong, Korea: Korea Institute for Health and Social Affairs;2015.
6. Hersh WR, Helfand M, Wallace J, Kraemer D, Patterson P, Shapiro S, et al. Clinical outcomes resulting from telemedicine interventions: a systematic review. BMC Med Inform Decis Mak. 2001; 1:5.

7. Wootton R. Telemedicine support for the developing world. J Telemed Telecare. 2008; 14(3):109–114.

8. Peetso T. Telemedicine: the time to hesitate is over! EuroHealth. 2014; 20(3):15–17.
9. Base Act on Health and Medical Service. Seoul, Korea: Ministry of Health and Welfare;2015.
10. Lee JH. u-Health trend and policy direction for the revitalization of its economy. KISDI Issue Rep. 2010; 9:1–48.
11. Korea Ministry of Health and Welfare. Patient satisfaction of telehealth raised up to 77% [Internet]. Sejong, Korea: Ministry of Health and Welfare;2015. cited at 2015 May 22. http://www.mw.go.kr/front_new/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&BOARD_ID=140&BOARD_FLAG=00&CONT_SEQ=322478&page=1.
12. Korea Ministry of Health and Welfare. Governmental guidelines on telemedicine of the cooperative emergency patient care demonstration trials among medical providers of the low medical service areas. Sejong, Korea: Ministry of Health and Welfare;2015.
13. Song TM. Trends and policy agenda of u-health. Sejong, Korea: Korea Institute for Health and Social Affairs;2013.
14. Busse R. Disease management programs in Germany's statutory health insurance system. Health Aff (Millwood). 2004; 23(3):56–67.

15. Pittman PM, Arnold SB, Schlette S. Care management in Germany and the U.S.: an expanded laboratory. Health Care Financ Rev. 2005; 27(1):9–18.
16. PwC EU Services. European Hospital Survey: benchmarking deployment of ehealth services (2012-2013): final report. Luxembourg: Publications office of the European Union;2014.
17. Maghiros I. Benchmarking information and communication technologies in health systems. In : Presented at Joint EC-OECD Workshop; 2013 Apr 18-19; Brussels, Belgium.
18. Park YR. Telemedicine time [Internet]. Seoul, Korea: inews24.com;2012. cited at 2015 Sep 15. Available from: http://news.inews24.com/php/news_view.php?g_serial=658734&g_menu=020800.
19. Hasegawa T. The promotion of telemedicine what is problem? Takasaki, Japan: Japanese Telemedicine and Telecare Association;2013.
20. Park SK. A study on the regional differences of telemedicine and digital divide. J Korean Geogr Soc. 2015; 50(3):325–338.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download