1. Costs
As described in the Methods section, costs were divided into 2 categories; the system costs and the induced costs. Among the system costs, the purchase cost of the system infrastructure in 2006 was US$1,241 thousand with a 5-year warranty included. Maintanence costs have been incurred since 2010. The development costs of the EMR viewer and the medical device interface system (MDIS) were US$1,006 thousand in 2006, US$1,274 thousand in 2007, and US$315 thousand in 2008. Maintanence costs for these applications have been incurred since 2009, and increased by 5.5% every year under Korean government guidelines. Office supplies, such as PCs, monitors, printers, etc., were purchased and the financial costs were US$306 thousand in 2006 and US$286 thousand in 2007. Maintaning these items costs 10% of the initial investment after the 1-year free warranty. Among the induced costs, the cost of investing in the existing paper-chart scanning system was US$724 thousand in 2008 and US$519 thousand in 2009. The personnel costs for MT support also have been incurred since September 2006. The cost for MT support was US$166 thousand in 2006. The PV of all accrued costs was US$16,054 thousand.
2. Benefits
To assess the benefits of cost reduction, we measured the supply consumption of September 2008 and compared it to the equivalent figures for 2006 and 2007. The supplies included paper-chart holders, labels, A4-size paper, gloves, etc., which were used to build and maintain the paper-charts. As a result, about 1.3 million pieces of A4-size paper were saved in 2008. The transportation cost of the paper-charts to the outside storage facilities and the building costs related to the automated cabinets and carousel facility were also saved. The PV of the supply savings was US$1,076 thousand.
Scanning existing paper-charts helped to eliminate 495 m2 of indoor storage and 627 m2 of outside warehouse space. According to our analysis, about 1 m2 was needed to store the paper-charts of about 910 new outpatients, and an additional 150 m2 per year were needed. Thus, the rental fees for the storage space were converted into a financial benefit. The PV saved from storage was US$703 thousand.
The paper-chart management FTEs built, delivered, and collected the paper-charts. After adoption of the EMR system, the number of the FTEs was greatly decreased from 28 in 2007 to 1 in 2009, whereas the number of outpatients per day significantly increased. The actual decrease in 2009 was 27. However, this study applied 32 FTEs since this study had to consider the growth of outpatients, which would have affected the number of the paper-charts to be delivered. The figure for the 32 FTEs was not recorded in the accounting records, but it was a conservative estimate from the chief of the department of medical records, who had vast experience in administration of the paper-charts. She expressed that the number depended only on the linear relationship to the growth of outpatients, but it did not consider the expansion of the buildings and the distance between them. There were only 7 actual reduced FTEs in 2008, but it was estimated that up to 36 FTEs would have been reduced in 2013. The only job left is to scan the signed consent forms into the EMR system. The PV of the FTE reduction was US$4,231 thousand.
Registered nurses in charge of the outpatient care floors showed that there were also 11 clerks fully dedicated to the management of the paper-charts, and they were laid off after the EMR adoption. It was very difficult to calculate the number of clerks on the outpatient care floors because the management of paper-charts on the floor was usually shared by all of the clerks. The registered nurses expressed that there were about 20 separate outpatient care areas, but only 11 clerks were moved to another department or did not have their contracts renewed. It is also conservative in that it did not consider the expansion of a building with about 10 outpatient care floors. The PV from the decreased clerk FTEs was US$990 thousand.
In 2009, the number of medical devices interfaced with the EMR system through the MDIS was 352. The MDIS has saved supplies for medical devices such as A4-size paper, photographic paper, and roll-paper. The reduced cost for only 126 devices in 2006 was US$7 thousand. The yearly cost reductions were proportional to the number of interfaced devices. The PV of the savings was US$944 thousand.
Among the benefits, additional revenues have been recognized from the paper-chart storage areas. The indoor storage was remodeled into clinic rooms for outpatient examinations. The revenue from this clinic was US$17 thousand in 2009, considering the contribution (4.15%) of the remodeled space to the revenue. The PV of the generated revenue was US$125 thousand.
After adoption of the EMR system, 5 paper-chart temporary storage rooms on the outpatient care floors were also converted to clinic rooms. In this case, the contribution of the remodeled space to revenue was 4.02%. The PV from the clinic rooms was US$1,646 thousand.
This study also found that the MT assistance also contributed to the growth of the number of outpatients per examination session. The contribution degree is counted as 25% of the growth; about 1.2 outpatients per the session they attended. The PV of additional revenue from the MT contribution was US$9,956 thousand. The total PV of all accrued benefits was US$19,672 thousand.
During the analysis period, the cumulative NPV and the BCR were US$3,617 thousand and 1.23, respectively. The DPP was about 6.18 years (
Table 3).
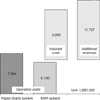
Total personnel costs for MT support were US$8,612 thousandwhich was 53.6% of total accrued costs (US$16,054 thousand). The direct costs for the EMR applications and the system infrastructure were 21.9% and 10.0%, respectively. These 3 items covered 85.5% of the total costs.
Among benefits, additional revenue from MT support was also the largest at 50.6% of the total accrued benefits (US$19,672 thousand). The reduction of chart management FTEs contributed 21.5% to the benefits. The additional revenues incurred from remodeling of paper-chart storage areas accounted for 9.0% of the benefits. These 3 items also covered 80.5% of the total benefits.
Both the costs and the benefits are largely influenced by the MT support, which was introduced to smooth EMR adoption. Scaning the existing paper-charts and storing them in the EMR system allowed the remodeling of the storage rooms into outpatient examination rooms. The benefits from this remodeling were also a large proportion of the total benefits. Looking at these results, the combination of the MT support and scanning the existing paper-charts could lead to different results. Therefore, this study attempted a case analysis with these 2 items.
3. Case Analysis
The SMC invested in both scanning the existing paper-charts and MT support with the EMR adoption. In other cases, one of these might be excluded or both might be excluded. Thus, 3 additional cases were used for the economic evaluation (
Table 4).
If a 5-year analysis period would have been applied, the cumulative NPV would have been under 0. However, the cumulative NPV based on an 8-year analysis is greater than 0. Thus, the EMR system can be financially cost-effective, but only if it is used for at least 4 or 5 years after full implementation.
The most cost-effective choice would have been investing in a simple transition from the paper-charts to the EMR system. Without scanning the existing paper-charts and the MT assistance, the cost would have been much lower. The DPP in this simple transition would have been 5.45 years which is a little shorter than in other scenarios. Even though it would be the best choice among other scenarios, it still does not meet the SMC's expected ROI period.






 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download