This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
To explore classification rules based on data mining methodologies which are to be used in defining strata in stratified sampling of healthcare providers with improved sampling efficiency.
Methods
We performed k-means clustering to group providers with similar characteristics, then, constructed decision trees on cluster labels to generate stratification rules. We assessed the variance explained by the stratification proposed in this study and by conventional stratification to evaluate the performance of the sampling design. We constructed a study database from health insurance claims data and providers' profile data made available to this study by the Health Insurance Review and Assessment Service of South Korea, and population data from Statistics Korea. From our database, we used the data for single specialty clinics or hospitals in two specialties, general surgery and ophthalmology, for the year 2011 in this study.
Results
Data mining resulted in five strata in general surgery with two stratification variables, the number of inpatients per specialist and population density of provider location, and five strata in ophthalmology with two stratification variables, the number of inpatients per specialist and number of beds. The percentages of variance in annual changes in the productivity of specialists explained by the stratification in general surgery and ophthalmology were 22% and 8%, respectively, whereas conventional stratification by the type of provider location and number of beds explained 2% and 0.2% of variance, respectively.
Conclusions
This study demonstrated that data mining methods can be used in designing efficient stratified sampling with variables readily available to the insurer and government; it offers an alternative to the existing stratification method that is widely used in healthcare provider surveys in South Korea.
Keywords: Sampling Studies, Decision Trees, Data Mining
I. Introduction
Stratified random sampling or stratified sampling, as opposed to simple random sampling, is often used in the field of healthcare management and policy [
1]. A stratified sample is defined as one resulting from classification of population into mutually exclusive groups, called strata, and choosing a simple random sample from each stratum. The main reason for using stratified sampling instead of simple random sampling is improved efficiency of sampling [
2,
3]. Sampling efficiency is the amount of information obtained for a given sampling cost, and the efficiency of stratified sampling is usually better than the efficiency of simple random sampling because the classification of population into strata can reduce variability of measurements within a stratum and result in smaller bounds on estimation errors [
2,
3]. Therefore, stratification should reduce variability within strata and increase variability between strata to achieve the intended improvement of sampling efficiency. Well-designed stratified sampling should be able to define strata where measurements within strata are homogeneous.
Stratified sampling is widely used in studies regarding healthcare policy formulation to sample healthcare providers in South Korea. The variables often used to define strata in these studies include the type of medical facilities defined by the medical law-tertiary hospitals, general hospitals, hospitals, and clinics, the type of location defined by the local autonomy law-district of special and metropolitan city, county of special and metropolitan city, city of province, and county of province, the size of providers defined by the number of beds a provider operates, and the type of ownership. However, the appropriateness of the variables in defining strata within which measurements should be homogeneous has been rarely studied, although managerial and clinical characteristics of providers vary widely within categories of the variables used to define strata. Conflicting interests of stakeholders are common in healthcare policy scenes, and the appropriateness and generalizability of samples has been a source of controversy as to the validity of study findings. Scheaffer et al. [
3] suggested 3 criteria to be considered in deciding the design of stratified sampling: 1) measurements within strata should be homogeneous, 2) the survey cost should be reduced by stratification, and 3) estimates of population parameters for each stratum should be useful.
The objective of this study was to demonstrate how data mining methodologies can be used to design stratification rules that improve sampling efficiency compared to designs that are generally used in policy studies in South Korea. We introduce the method by presenting the study that we conducted as a part of a project supported by a grant from the Health Insurance Review and Assessment Service (HIRA) of South Korea; in the study, a framework was developed for updating payment rates in the Diagnosis Related Groups (DRGs) based prospective payment system as well as work processes, including sampling healthcare providers and collecting data needed to analyze updates from the sample [
4]. The project concerned factors that affect changes in the cost of treating patients that should be factored into payment updates. Examples of those factors are changes in prices of input resources, such as labor and materials, and changes in productivity.
In this study, we explored variables and classification rules based on data mining methodologies for defining strata in surveys of healthcare providers. We performed cluster analysis to segment medical facilities with similar characteristics. Then, decision trees were created to generate rules to clearly identify and analyze each cluster, which is used to define sampling strata. We compared the efficiency of the proposed sampling design with that of a conventional design of stratified sampling to assess the effectiveness of this approach.
In data mining or the process of Knowledge Discovery in Databases, interesting patterns and knowledge are discovered from large amounts of data. A pattern is interesting if it is valid on test data with some degree of certainty, novel, useful, and easy to understand [
5]. Data mining involves a number of common classes of tasks. One of them is cluster analysis, or simply clustering. It is the process of partitioning a set of data observations into subsets. Each subset is a cluster, such that observations in a cluster are similar to one another, yet dissimilar to observations in other clusters. Another task is classification. Classification is a form of data analysis that extracts models or rules describing important data classes or labels. Such models, called classifiers, predict categorical class labels, which are discrete and unordered.
One natural application of cluster analysis is consumer segmentation in consumer relationship management (CRM). For example, Hung et al. [
6] used k-means clustering methods to segment the customers in the Taiwanese telecommunication market into five clusters of roughly equal size according to their billing amounts, tenure months, and payment behaviors. Then, they created a decision tree model in each cluster to see if the churn behaviors, or attrition rates, differed for various segments. There was also a study that applied k-means clustering and decision tree algorithms to detect healthcare providers with abusive billing patterns in South Korea [
7]. Ngai et al. [
8], in their review article, showed that decision tree and k-means clustering were highly popular data mining tools in CRM research.
II. Methods
1. Analysis
This research selected k-means clustering and decision tree induction as data mining techniques to segment and classify healthcare providers. The k-means algorithm is a method of cluster analysis which aims to partition n observations into a predetermined number of k clusters in which each observation belongs to the cluster with the nearest mean. The algorithm proceeds as follows. First, it randomly selects k of the observations in the data set, each of which initially represents a cluster mean or center. For each of the remaining observations, an observation is assigned to the cluster to which it is the most similar, based on the Euclidean distance between the observation and the cluster mean. The k-means algorithm then iteratively improves the within-cluster variation, and the iterations continue until the assignment becomes stable. On the other hand, the construction of decision tree classifiers does not require any domain knowledge or parameter setting. Decision trees can easily be converted to classification rules that are intuitive and generally easy to understand. Decision tree induction algorithms have been used for classification in many application areas, such as medicine, manufacturing and production, financial analysis, astronomy, and molecular biology [
5].
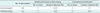
We studied a sampling design for single specialty clinics or hospitals in the two specialties, general surgery and ophthalmology. We chose the nine most relevant and representative variables to be used in clustering among 94 highly correlated variables we had in the study database of healthcare providers. They included type of provider location (REG), population density of the region (POPD), number of specialists the provider had (MD_SPEC), number of beds (FAC_SICK), number of inpatients per specialist (NPAT_SPEC), lengthiness index (LI), costliness index (CI), case-mix index (CMI), and rate of annual change in number of inpatients per specialist (CHG_NPAT_SPEC). Details of variable definition are given in
Table 1. The number of clusters for each specialty of clinics and hospitals was decided based on discussions with experts in the project team and Silhouette coefficients, which measure cohesion and separation of clusters. Clustering was performed using clustering functions in the Matlab ver. 7.11 program (MathWorks Inc., Natic, MA, USA). Then, Spotfire ver. 4.5 (TIBCO Spotfire, Somerville, MA, USA) was used to visualize the clustering results. We used SAS E-miner ver. 4.3 (SAS Institute Inc., Cary, NC, USA) to create decision trees.
We evaluated the performance of the proposed sampling design by assessing the degree of variance reduced or explained by the classification of clinics and hospitals with a single specialty into strata as a measure of sampling efficiency following the suggestion by Scheaffer et al. [
3]. We compared the efficiency of the stratification proposed in this study with the efficiency of conventional stratification based on the type of administrative region of provider location and the size of inpatient bed. The type of administrative region had four categories, namely, district of special and metropolitan city, county of special and metropolitan city, city of province, and county of province; size had two categories, that is, with 30 or more beds and with fewer than 30 beds. We conducted an analysis of variance (ANOVA) to compute the degree of variance reduction achieved by stratifications. The dependent variable used in the analysis was the annual rate of change in the number of inpatients per specialist which is a measure of changes in productivity, and the categorical independent variables were strata. SAS ver. 9.3 (SAS Institute Inc.) was used for statistical computations and tests.
2. Data
We constructed a study database of providers with data from the HIRA and Statistics Korea (KOSTAT). The major sources of data from the HIRA were inpatient insurance claims data and provider profile data. The inpatient insurance claims data comprised claims submitted to the HIRA by providers for insurance payments from January 2006 to December 2011, and there was a total of 50,769,933 records. Each record included claims information as to a hospitalization for inpatient care, and the information items in each record were patient ID, provider ID, type of provider, Korean DRG code, gender, age, length of stay, and charges. Provider profile data comprised provider information as of the end of each calendar year from 2006 to 2011, and there was a total of 174,081 records. Each record included provider ID, type of medical facilities, type of ownership, establishment date, numbers of general doctors, specialists in each of 26 specialties, nurses, and inpatient beds. We attached the population density statistics obtained from KOSTAT to the profile data by the provider location and year [
9]. We computed yearly statistics using claims data for each provider, such as total numbers of inpatients and inpatients in the four specialties of-general surgery, obstetrics and gynecology, ophthalmology, and otolaryngology-who were paid by the DRG-based prospective payment system, LI, CI, and CMI, and merged them with provider profile data by provider ID and year. We further computed measures of physician productivity in the four specialties in terms of the number of inpatients per specialist with merged data. We used the two-year moving average to compute annual change in physician productivity which was used as the dependent variable in the ANOVA.
Table 1 shows the detailed definition of study variables and data sources.
We excluded providers which were established in the year 2009 or after for the completeness of data and excluded those with an absolute change rate value greater than 0.5 as outliers from the study. Finally, we used data for the year 2011 in this study, and 442 clinics and hospitals with the specialty of general surgery and 715 clinics and hospitals with the specialty of ophthalmology were included in the analyses.
III. Results
1. Clustering
We identified three clusters of general surgery clinics and hospitals, and their general characteristics are presented in
Table 2. Providers in cluster 1 were mostly private clinics in rural areas with a low number of inpatients per specialist and a decreasing number of inpatients in the DRGs paid by the DRG-based prospective payment system. Those in cluster 2 were relatively large private clinics and hospitals with a decreasing number of inpatients, and those in cluster 3 were mostly urban clinics with a large number of inpatients.
We identified four clusters of ophthalmology clinics and hospitals, and their general characteristics are presented in
Table 2. Providers in the cluster 1 were relatively small private clinics located in metropolitan areas with a low number of inpatients in the DRGs paid by the DRG-based prospective payment system. Those in cluster 2 were large clinics with multiple specialists and beds for inpatient care, and those in cluster 3 were private clinics in rural areas with a decreasing number of inpatients in the DRGs paid by the DRG-based prospective payment system. Providers in cluster 4 were large private clinics with an increasing number of inpatients.
2. Decision Tree and Rules to be Used in Stratification
The decision tree we constructed to identify three clusters of general surgery clinics and hospitals is shown in
Figure 1. Three variables were used to classify clinics and hospitals into homogeneous groups or strata, namely, the number of inpatients per specialist who were in the DRGs paid by the DRG-based prospective payment system (NPAT_SPEC_GS), population density (POPD), and lengthiness index (LI_DRG). The suggested classification rule would result in five strata:
Stratum 1: clinics and hospitals with fewer than 57 inpatients per specialist and located in a city/county/district with a population density lower than 83,
Stratum 2: clinics and hospitals with fewer than 57 inpatients per specialist and located in a city/county/district with a population density higher than 82,
Stratum 3: clinics and hospitals with 57 to 123 inpatients per specialist whose lengthiness index was less than 0.95,
Stratum 4: clinics and hospitals with 57 to 123 inpatients per specialist whose lengthiness index was larger than 0.94,
Stratum 5: clinics and hospitals with more than 123 inpatients per specialist.
The general characteristics of clinics and hospitals in each stratum are presented in
Table 3. The results show that clinics and hospitals in strata 2 and 3 had significantly different inpatient volumes in the DRGs paid by the DRG-based prospective payment system in general surgery even though the characteristics of the type of location and the number of beds were not very different, which means they may have been classified into a stratum in a conventional stratified sampling that uses the type of location and the number of beds as stratification variables. Also, clinics in strata 4 and 5 appear to be similar in terms of the type of location and the number of specialists even though the productivities of specialist measured by the number of inpatients per specialist are not.
The decision tree we constructed to identify four clusters of ophthalmology clinics and hospitals is shown in
Figure 2. Two variables were used to classify clinics and hospitals into homogeneous groups or strata, namely, the number of patients per specialist who were in the DRGs paid by the DRG-based prospective payment system (NPAT_SPEC_EYE) and the number of beds (FAC_SICK). The suggested classification rule would result in five strata:
Stratum 1: clinics and hospitals with fewer than 60 inpatients per specialist,
Stratum 2: clinics and hospitals with fewer than 4 beds and with 60 to 421 inpatients per specialist,
Stratum 3: clinics and hospitals with fewer than 4 beds and with more than 421 inpatients per specialist,
Stratum 4: clinics and hospitals with more than 3 beds and with 60 to 196 inpatients per specialist,
Stratum 5: clinics and hospitals with more than 3 beds and with more than 196 inpatients per specialist.
The general characteristics of clinics and hospitals in each stratum are presented in
Table 3. The patient volumes of clinics in strata 1 and 2 were different, although they were mostly located in urban areas with a single specialist in ophthalmology, which implies that clinics in stratum 1 may focus in ophthalmology care not covered by the national health insurance. Stratum 3 includes clinics with a single specialist and a single bed in all types of location whose patient volume in the DRGs paid by the DRG-based prospective payment system is heavy; therefore, the physician productivity in ophthalmology care in those DRGs is high.
3. Evaluation
The performance of the stratification using the variables and rules found through data mining methods were far better than the performance of conventional stratification based on the type of location and bed size in both specialties (
Table 4). The percentages of variance explained by the stratification based on data mining methods for general surgery and ophthalmology clinics and hospitals were 22% and 8%, respectively, whereas the percentages explained by conventional stratification were 2% and 0.2%; although fewer strata were created by data mining methods than by conventional stratification. These findings imply that the homogeneity of measurements, changes in physician productivity in this evaluation, within strata is better with stratification by data mining methods than that of conventional stratification; thus, sampling efficiency is improved.
IV. Discussion
This study attempted to find a stratified sampling design based on data mining methods that achieves improved sampling efficiency over designs conventionally used in studies of healthcare providers for management and policy decisions in South Korea. Utilizing widely used data mining methods, we wanted to provide an explanatory study that would offer an efficient alternative that can be easily adopted by health care professionals. Specifically, cluster analysis groups a data set according to perceived intrinsic characteristics or similarity and is known to find structure in data which, in turn, can be identified as stratification rules by the application of decision tree induction on the cluster labels [
5,
10]. The stratification rules found in this study defined strata with far better homogeneity within strata in measurements with several classification variables and fewer strata than conventional stratified sampling did. In our evaluation study of clinics and hospitals in the specialties of general surgery and ophthalmology, the performance of stratification by the type of provider location and bed size which is widely used in policy studies in South Korea was so inadequate that the stratification did not add any value in sampling efficiency over simple random sampling. Clinics and hospitals with single specialty were quite heterogeneous within categories of the type of provider location and bed size, the variables routinely used to classify providers to homogenous groups, and they were not good predictors at all.
Fueled by conflicting interests of stakeholders, inappropriate sampling and generalizability of samples have been major sources of controversy over findings of policy studies, particularly studies concerning payment rates which are affected by providers' managerial, financial, and environmental characteristics. This study demonstrated that data mining methods can be applied to find an intelligent sampling design with data that are routinely collected and readily available to the insurer, the government, and researchers. Stratification rules may need to be updated in three to five years as the economic, social, and policy environment changes. The sensitivity of sampling results and performance to changes in classification thresholds should be further investigated to achieve robust sampling designs.
This study is not free from limitations, and further studies are needed. First, we did not examine the applicability of the sampling designs found in this study in a variety of study settings. Although we can assume that the classification rules could hold in studies concerning providers' managerial and financial performance, we did not explicitly look into the applicability of study findings in this regard. Second, the study findings suggest different classification variables and rules for providers in different specialties and this may be obvious to achieve maximum efficiency. However, we did not explore whether it would be optimal to have different rules for different groups of providers in terms of sampling efficiency, overall costs, and the simplicity of sampling schemes. Third, we did not perform out-of-sample analysis in building our decision trees. However, overfitting would not be a major problem in this study due to pruning procedures we performed. In a future study, we may want to perform out-of-sample analysis and compare the predictability of our model with other popular data mining methods, such as support vector machines. Lastly, during the variable selection process in the clustering analysis, due to time constraints, we automatically excluded variables with 80% or more missing values from the analyses. However, in a future study, we may want use an appropriate algorithm to impute missing values for some key variables and test if the use of these variables would result in better clustering.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download