This article has been corrected. See "Correspondence" in Volume 18 on page 290.
Abstract
Objectives
Healthcare institutions need timely patient information from various sources at the point-of-care. Evidence-based medicine (EBM) is a tool for proper and efficient incorporation of the results of research in decision-making. Characteristics of medical treatment processes and practical experience concerning the effect of EBM in the clinical process are surveyed.
Methods
A cross sectional survey conducted in Tehran hospitals in February-March 2012 among 51 clinical residents. The respondents were asked to apply EBM in clinical decision-making to answer questions about the effect of EBM in the clinical process. A valid and reliable questionnaire was used in this study.
Results
EBM provides a framework for problem solving and improvement of processes. Most residents (76%) agreed that EBM could improve clinical decision making. Eighty one percent of the respondents believed that EBM resulted in quick updating of knowledge. They believed that EBM was more useful for diagnosis than for treatment. There was a significant association between out-patients and in-patients in using electronic EBM resources.
Conclusions
Research findings were useful in clinical practice and decision making. The computerized guidelines are important tools for improving clinical process quality. When learning how to use IT, methods of search and evaluation of evidence for diagnosis, treatment and medical education are necessary. Purposeful use of IT in clinical processes reduces workload and improves decision-making.
In recent decades, information and communication technologies have changed the way of life in all aspects including health care. Scientific texts show that application of information technology for making the best decision in the medical arena is crucial [1,2]. Many data are produced in this field. However, there is a lack of programs, systems and formal structures to convert this data into meaningful health information. Hence, it could be said with certainty that health care organizations have strong data but weak knowledge [3].
Panzarasa et al. [4] showed that medical knowledge in current health care systems was not essentially used. In its report in November 1999, the Institute of Medicine announced that in the United States, nearly 98,000 mortalities occur each year due to medical errors, making them the third cause of mortality. Administrative measures, and even employees and executive tasks are part of these errors [5]. These cases represent inappropriate use, failure in delivering timely information to health care providers and lack of appropriate technology to support transfer, delivery, presentation and integration of information. It is also important to note that health care with the highest dynamic rate faces numerous challenges and needs maximum coordination.
During the past 20 years, process-oriented information systems
for integration and coordination of patients' treatment have always been discussed [6]. Information technology (IT) is used as a tool in managing health care information. In fact, IT is the automated process of places and points that documents, information and tasks move between parts and members of an organization on the basis of predefined rules and policies to meet organizational goals [7]. Significant improvements in the quality and safety of the health care domain have been achieved through health information technology (HIT) [8]. Many studies have identified the positive effects of HIT such as Electronic Health Records (EHR) in health care systems, particularly in the management of adverse drug reactions and patient-centered medical practice [1,9]. EHR with the support of structured data entry, electronic information exchange, participation in medical care and risk reduction measures for patients acts as a central database for data integration of different health systems [10]. In researches related to the role of IT, it has been determined that the major side effects of drugs are associated with inadequate communication and little information of the medical staff [11]. IT prepares health care practitioners with correct information and timely access and supports the processes of patient care [12]. However, despite these facts, there are significant gaps between the application of IT and its potential benefits [13]. What could be the reason for the limited use of IT in supporting information flow between processes in health care? To find a suitable response it is essential to understand complex characteristics of health care [14]. Therefore, evidence-based medicine (EBM) as an approach that applies IT is briefly discussed theoretically and practically in this research.
In this section, basic characteristics of medical treatment processes and their relationship with medical knowledge and patient data are considered. Also, the nature of medical treatment process and related parameters, as a basis for evaluating potential IT especially EBM, to improve the quality of treatment processes and medical decision-making has been studied.
Medical care organizations, due to increased staff workload in performing the duties, need to correct required resources to use advanced tools in order to convert data and information to high quality knowledge through automating the processes of treatment. A medical therapeutic process often comprises data collection (observation), diagnosis, and therapeutic plan [14]. It starts with the patient history, demographic data and proceeds with diagnostic procedures that are selected based on available information. The role of (electronic) medical records, as IT, is to assist healthcare personnel in making informed decisions. Consequently, the system should present relevant information at the time of data acquisition and at the time of order entry [15]. In any medical discipline, the diagnosis is made by taking some of the data and converting this data into information by a physician or other medical practitioners. Based on the diagnosis, appropriate treatment, which may take months or even years, is selected for most diseases like high blood pressure or cancer [16]. Each pass of this cycle aims at decreasing uncertainty about the patient's disease or the actual state of the disease process [15]. Thus, an important question that should be answered is how relevant data can be determined. The available information only comprises primary assumptions for decision-making. There are numerous medical software programs on the Internet installed on computers. Clinical reference applications that provide guidelines and information can be accessed via the Internet. Availability of clinical data at the point of care provides access to complete and accurate clinical information for the care provider. Dosage and computational formulas, which were previously available only through printed material but are now accessible through handheld computers, can help to reduce medical errors and update old data [17]. They may offer solutions to administrative and information management that are more realistic than those offered by desktop computers or traditional Electronic Medical Record (EMR). There are different tools for providing computer-based medical guidelines such as proformalisation, which is a process of capturing clinical expertise in a form that can be directly applied by one agent (such as a computer) on behalf of another (such as an expert clinician or an authoritative organization). CAPSULE is an example of proformalised expertise [18]. IT is a decision support system designed to advise on the prescription of medications for common conditions in general practice [19]. Asbru is another tool which places a particular emphasis on an expressive representation for time-oriented actions and world states [20]. Quaglini describes a methodology for representing clinical practice guidelines and facilitating their introduction into the medical routine [21].
This section consists of two parts; part one examines the problems of traditional ways and explains benefits of EBM as a new solution. The second part is practical work conducted in a university hospital.
There is no doubt that both physicians and patients benefit from strategies that improve diagnosis, clinical judgment, and decision making [22]. EBM is the conscientious, explicit, and judicious use of current best evidence in making clinical decisions about patient care [23]. EBM is being applied to decisions in a range of contexts beyond one-to-one patient care [24]. In the present era of technology, medical procedures and treatments are not acceptable only based on specialists' old information [25]. Hillman [26] stated that medical procedures essentially based on old data, uncontrolled studies, expert opinions and financial constraints may increase the possibility of inappropriate actions. Medical knowledge limited to medical reference books is rapidly changing [27]. On the other hand, there is a large gap between the information contained in published medical guidelines and the knowledge required to perform remedial action. An appropriate way to fill this gap is through the application of IT and focusing on medical informatics research. Physicians usually do not have enough time to do all the above-mentioned activities [26]. Covell et al. [19] showed that only 30% of the physicians' information needs were met during patient visit and that this percentage could usually be achieved through asking questions from colleagues. They also mentioned that lack of necessary knowledge and up-to-date recourses needed by professional, time shortage for the retrieval of information from texts, and old printed material were among the reasons why physicians were not willing to use traditional resources [19]. Sackett et al. [28] reported that 52% of the information searches to answer clinical questions resulted in effective management decisions, 25% led to new treatments or diagnoses and 23% led to correction of previous treatment programs. Crowley demonstrated [18] that 53% of clinical questions led to management decisions and 47% led to changes in medications, diagnostic tests and information modification given to patients [29]. Many efforts have been made to establish standards for modeling of diagnostic and therapeutic guidelines [30]. Medical guidelines with direct medical knowledge at the point of care with an evidence-based nature and access to updated information help to improve the quality of treatment and treatment outcomes, reduce unwanted errors and decrease economic costs [31]. Greenes and Lorenzi [32], Stead et al. [33], and Shiffman et al. [34], in separate researches, studied the effective ways of applying medical guidelines in clinical settings and stated that the guidelines provided features for timely and rapid access to information, through which physicians would be able to respond and make decisions quickly using appropriate and accurate information in real time [25]. Several official websites such as www.guideline.gov have been created in order to share medical knowledge among physicians. Many of these websites can create texts in HTML or text format and provide useful links [3]. The most important step in EBM is to collect the best available evidence (primary and secondary papers registered in databases) to answer a clinical question. It has been determined that practitioners who have established their actions based on scientific evidence could make better decisions, perform high quality of care, and reduce costs and hospital stays [35].
To sum up, EBM is a tool for proper and efficient incorporation of the results of research in decision-making. Accessing and retrieving valid and reliable evidence is possible through the knowledge of proper electronic databases and systematic and purposeful search strategies. Lack of knowledge about the best available evidence is one of the main causes of application of various and controversial medical treatments [22].
A cross sectional survey was conducted in February-March 2012 at Tehran University of Medical Sciences (TUMS) among clinical residents. A valid and reliable questionnaire was used in this research [22,36]. Residents were free to participate and an informed consent ensured the confidentiality of collected data. First, the ability of the participants to access, use, and interpret found evidence in the clinical process was examined. Then, the respondents were asked to apply EBM in clinical decision-making to answer questions about the effect of EBM in the clinical process. Convenience sampling method was used to select respondents in the study. The questionnaire comprised 3 sections and 12 statements. Three questions included demographics feature, 2 items covering attitudes and familiarity toward EBM, 5 items about the EBM effect on clinical decision making, and two open questions gave participants the opportunity to state their views of the major barriers and encouraging mechanisms All questionnaires were distributed personally by the authors in order to reduce non-response bias. Responses to closed questions were categorized on a 1-5 scale and options that were "rather negative" received negative ratings. Hence, all of the questions were evaluated based on a 1-4 Likert scale. Association between two categorical variables was tested using chi-square test. The statistic is performed utilizing a 2-tailed test and significance level of 0.05. Answers were reviewed and categorized with Microsoft Office Excel and the data collected were analyzed using statistical software SPSS ver. 11.0 (SPSS Inc., Chicago, IL, USA).
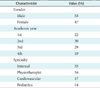
Demographics of for the respondents, their academic years and specialties are presented in Table 1. Internists were the group with the highest application of EBM process in the diagnostic plan.
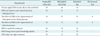
We assumed that the residents' knowledge of specific EBM processes in clinical decision-making was limited. Of the 51 questionnaires, nine with poor rating were excluded (14%). As shown in Table 2, out of 42 completed questionnaires with positive response, most (76%) agreed that EBM could improve clinical decision making from the standpoint of the accuracy of the treatment process implemented by residents. However, respondents had a negative opinion of the time of rendered services. Results showed that 34% of the respondents were of the opinion that practicing EBM improved clinical decision-making. They believed that EBM was more useful for diagnosis than for treatment. The results showed that there was a significant association in using electronic EBM resources between outpatients and in-patients (χ2 = 6, df = 2, p = 0.002).
Main comments in open questions showed that residents do not have the time to discuss the resource to patients and search databases or websites. Besides, encouragement mechanisms have not been adopted through health care administrators or hospitals policy makers. In addition, some respondents stated they would prefer to get answers during clinical practice through colleagues' consultation rather than EBM sites.
Health care, due to the utilization of research findings and new medical technologies, is one of the fastest changing areas in the world. Healthcare institutions need timely patient information from various sources at the point-of-care and they are often willing to buy a comprehensive, complete and fully functional system fulfilling all their needs from one vendor. Given the need to identify health care processes, it is necessary to separate therapeutic from organizational processes.
According to the results of this study, 81% of the respondents believed that EBM resulted in a quick knowledge update. EBM is the result of the integration of three basic components: The best and most recent evidence-based systematic research, expertise and clinical experience of the physician and the patient, and community values. EBM has been a large part of the modernization of today's healthcare, and many see that it will become widespread in the future as more emphasis is put on taking the time to find the right diagnosis and enacting quality care [37]. It also provides a common framework for problem solving and improving communication and understanding between people from different backgrounds, such as clinicians and patients [38].
Findings of the practical study indicated that the respondents were not sure if EBM could take into account patients' personal preferences and improve the accuracy of the clinical process, which is in agreement with the results of previous studies [39,40]. EBM was seen to be necessary and respondents stated that the research findings were useful in clinical practice and decision-making. Similar results have been reported by previous studies [39,41]. A study in Ardebil, Iran, showed that lack of familiarity with EBM and related websites and databases were the main reason why most physicians did not use EBM databases [42]. Although 38% of the respondents claimed that they applied EBM in clinical decision-making, its application was not completely according to the EBM process. Some of them only checked databases such as PubMed without any appraisal or comparison.
Therefore, learning how to use information technology, methods of search and evaluation of evidence for diagnosis, treatment and medical education is necessary. Implementing collected evidence improves confidence in management decisions, enables clinicians to upgrade their knowledge routinely and enables them to communicate better with patients about the rationale behind management decisions [21].
Physiotherapy residents showed a significant difference in daily application of EBM in decision-making. The reasons seem to be the following. First, these specialists have patients for whom several sessions are needed, so they can spend more time on collecting credible evidence without receiving any negative feedbacks from other patients or colleagues. Second, the type of the patients' diseases, in terms of acute or chronic, differs from others. Findings of chi square test also indicated that residents had enough time to review resources and databases for the diagnosis of in-patients. So EBM resources for inpatients are more used.
Some respondents believed that current clinical guidelines lacked sufficient support for EBM practice and therefore they did not apply it in clinical decision-making. EBM is conducted through guidelines, which include general description based on available evidence and expert experiences [43]. Evidence-based guidelines can be found in numerous sources, and the overall goal is to aggregate the best data and use the conclusions to help to come to a clinical decision. Most of the past attempts have focused on the use of computer guidelines to support clinical care and resource management based on the updated medical information. IT increases effectiveness and efficiency of guidelines in information retrieval [4,15]. Hence, computerization of medical guidelines in comparison with traditional methods can potentially improve physicians' decision-making [5]. Despite the current rapid information growth and limitations that medical staff have in retrieving information, computerized guidelines are important tools for improving the quality of treatment [44,45]. Purposeful use of IT in clinical processes reduces workload and improves decision-making.
Figures and Tables
Acknowledgments
The authors would like to thank the residents of the Tehran University of Medical Sciences (TUMS) for their help and commitment during the completion of this research.
References
1. Maheu MM, Whitten P, Allen A. E-Health, telehealth, and telemedicine: a guide to start-up and success. 2001. San Francisco: Jossey-Bass.
2. Sim I, Gorman P, Greenes RA, Haynes RB, Kaplan B, Lehmann H, et al. Clinical decision support systems for the practice of evidence-based medicine. J Am Med Inform Assoc. 2001. 8(6):527–534.

3. Smith RG, Farquhar A. The road ahead for knowledge management: an AI perspective. AI Mag. 2000. 21(4):17–40.
4. Panzarasa S, Madde S, Quaglini S, Pistarini C, Stefanelli M. Evidence-based careflow management systems: the case of post-stroke rehabilitation. J Biomed Inform. 2002. 35(2):123–139.

5. Rezaei hachesoo P, Habibi S, Fozonkhah S. Information technology, an effective tool in reducing and preventing medical errors: suggestions for improvement. Health Inf Manag. 2007. 4(1):90–97.
6. Vegoda P. Introducing the IHE (Integrating the Healthcare Enterprise) concept. J Healthc Inf Manag. 2002. 16(1):22–24.
7. Zargar M. Principle and concepts of information technology. 2001. Tehran: Behineh Publication.
8. Kwak YS. Electronic health record: definition, categories and standards. J Korean Soc Med Inform. 2005. 11(1):1–15.

9. Seo JW, Kim KH, Choi JW, Ha KS, Chin HJ, Kim JU, et al. Implementation of electronic medical records at Seoul National University Hospital. J Korean Soc Med Inform. 2006. 12(3):213–225.

10. Ahmadi M, Rezaeehachesoo P, Shahmoradi L. Electronic health record: standards and evaluation. 2009. Tehran: Jafari Publication.
11. Lester WT, Grant RW, Barnett GO, Chueh HC. Randomized controlled trial of an informatics-based intervention to increase statin prescription for secondary prevention of coronary disease. J Gen Intern Med. 2006. 21(1):22–29.

12. Brennan TA, Leape LL. Adverse events, negligence in hospitalized patients: results from the Harvard Medical Practice Study. Perspect Healthc Risk Manage. 1991. 11(2):2–8.

13. Institute of Medicine, Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. 2001. Washington: National Academy Press.
14. Van Bemmel JH, Musen MA, Helder JC. Handbook of medical informatics. 1997. Heidelberg: Springer-Verlag.
15. Lenz R, Reichert M. IT support for healthcare processes: premises, challenges, perspectives. Data Knowl Eng. 2007. 61(1):39–58.
16. Decruyenaere J, De Turck F, Vanhastel S, Vandermeulen F, Demeester P, de Moor G. On the design of a generic and scalable multilayer software architecture for data flow management in the intensive care unit. Methods Inf Med. 2003. 42(1):79–88.

17. Criswell DF, Parchman ML. Handheld computer use in U.S. family practice residency programs. J Am Med Inform Assoc. 2002. 9(1):80–86.

18. Fox J, Johns N, Rahmanzadeh A. Disseminating medical knowledge: the PROforma approach. Artif Intell Med. 1998. 14(1-2):157–181.

19. Covell DG, Uman GC, Manning PR. Information needs in office practice: are they being met? Ann Intern Med. 1985. 103(4):596–599.

20. Miksch S, Shahar Y, Johnson P. In : Motta E, Harmelen F, Pierret-Golbreich C, Filby I, Wijngaards N, editors. Asbru: a task-specific, intention-based, and time-oriented language for representing skeletal plans. Proceedings of the 7th Workshop on Knowledge Engineering: Methods and Language; 1997 Jan 22-24; Milton Keynes, UK.
21. Quaglini S, Dazzi L, Gatti L, Stefanelli M, Fassino C, Tondini C. Supporting tools for guideline development and dissemination. Artif Intell Med. 1998. 14(1-2):119–137.

22. Sadeghi M, Khanjani N, Motamedi F, Saber M, Rad GS. Familiarity of medical residents at Kerman Medical University with evidence based medicine databases. J Res Med Sci. 2011. 16(10):1372–1377.
23. Kim S, Choi J. Improving the performance of text categorization models used for the selection of high quality articles. Healthc Inform Res. 2012. 18(1):18–28.

24. Tilburt JC. Evidence-based medicine beyond the bedside: keeping an eye on context. J Eval Clin Pract. 2008. 14(5):721–725.

26. Hillman BJ. Noninterpretive skills for radiology residents: critical thinking: deciding whether to incorporate the recommendations of radiology publications and presentations into practice. AJR Am J Roentgenol. 2000. 174(4):943–946.
27. Hawkins RC. The evidence based medicine approach to diagnostic testing: practicalities and limitations. Clin Biochem Rev. 2005. 26(2):7–18.
28. Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996. 312(7023):71–72.

29. Sackett DL, Straus SE. Finding and applying evidence during clinical rounds: the "evidence cart". JAMA. 1998. 280(15):1336–1338.

30. Crowley SD, Owens TA, Schardt CM, Wardell SI, Peterson J, Garrison S, et al. A Web-based compendium of clinical questions and medical evidence to educate internal medicine residents. Acad Med. 2003. 78(3):270–274.

31. Ohno-Machado L, Gennari JH, Murphy SN, Jain NL, Tu SW, Oliver DE, et al. The guideline interchange format: a model for representing guidelines. J Am Med Inform Assoc. 1998. 5(4):357–372.

32. Greenes RA, Lorenzi NM. Audacious goals for health and biomedical informatics in the new millennium. J Am Med Inform Assoc. 1998. 5(5):395–400.

33. Stead WW, Miller RA, Musen MA, Hersh WR. Integration and beyond: linking information from disparate sources and into workflow. J Am Med Inform Assoc. 2000. 7(2):135–145.

34. Shiffman RN, Brandt CA, Liaw Y, Corb GJ. A design model for computer-based guideline implementation based on information management services. J Am Med Inform Assoc. 1999. 6(2):99–103.

35. Habai S, Rezaei P, Tabaghi R. Enhancing information literacy as a base of developing evidence-based nursing. Health Inf Manag. 2010. 7(3):371–378.
36. Oliveri RS, Gluud C, Wille-Jorgensen PA. Hospital doctors' self-rated skills in and use of evidence-based medicine: a questionnaire survey. J Eval Clin Pract. 2004. 10(2):219–226.

37. Kelly MP, Moore TA. The judgement process in evidence-based medicine and health technology assessment. Social Theory Health. 2012. 10(1):1–19.

38. Rosenberg W, Donald A. Evidence based medicine: an approach to clinical problem-solving. BMJ. 1995. 310(6987):1122–1126.

39. Jette DU, Bacon K, Batty C, Carlson M, Ferland A, Hemingway RD, et al. Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys Ther. 2003. 83(9):786–805.

40. Retsas A. Barriers to using research evidence in nursing practice. J Adv Nurs. 2000. 31(3):599–606.

41. Heiwe S, Kajermo KN, Tyni-Lenne R, Guidetti S, Samuelsson M, Andersson IL, et al. Evidence-based practice: attitudes, knowledge and behaviour among allied health care professionals. Int J Qual Health Care. 2011. 23(2):198–209.

42. Habibi SH, Farzi J, Lotfollahzade R. Information seeking behaviour in Ardebil general physicians and their approach towards electronic resources. J Ardebil Univ Med Sci. 2008. 8(2):136–141.
43. Park M. Development of evidence based nursing practice guideline document model for electronic distribution. J Korean Soc Med Inform. 2004. 10(2):147–159.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download