Abstract
Objectives
We were to analyze the effect of managing metabolic syndrome using a u-health service in a health center.
Methods
We collected biometric data from 316 subjects living in a county (gun) in South Korea before and after the introduction of uhealth services in 2010. Analysis was done by contingency table using SPSS and latent growth model using AMOS.
Results
We found that regional u-health services affected instance of metabolic syndrome. Further, biometrics and health behavior improved. After six months of u-health services, the number of subjects with three or more factors for metabolic syndrome decreased by 62.5%; 63.3% of regular drinkers stopped drinking; 83.3% of subjects who rarely exercised began to exercise twice a week or more; and 60.9% of smokers stopped smoking.
With the improvement of standards of living in many countries worldwide, the demand for improved social welfare provisions, low birth rates, and aging societies, health services are changing their structure [1]. Traditional supplier-focused services and post-treatment services are transforming into pre-treatment and user-oriented services, which consider wellness and preventative healthcare more actively than in the past. In South Korea, as low fertility rates (total fertility rate is 1.23 in 2010) and the aging society (people aged 65 and over is 11.3% of its total population in 2008) [2] become increasingly problematic, two health-related problems are emerging: increasing demand for chronic-disease related healthcare services, and the rising cost burden on the government for increased health services. U-health, called telehealth or e-health in other countries, is considered a useful method to manage health-related problems, although evidence of the effectiveness of it is incomplete [3]. In Korea, u-health is defined as "healthcare services delivered through ubiquitous technology such as radio frequency identification (RFID), biometric devices, and ubiquitous sensor networks. In particular, u-health is testing intended to monitor and manage people's health incomes, including those of people with chronic diseases. In this situation, many countries can adopt u-health as a good countermeasure with two positive effects. First, it will ease the burden of healthcare services, which has a ripple effect throughout the healthcare industry. Second, it has policy effects on public healthcare and disease prevention.
Worldwide, the u-health market is expected to increase 15% or more annually by 2013, from US$ 1.057 trillion in 2007 to $ 2.537 trillion in 2013 [4]. It is anticipated that u-health services for elderly people, especially services for remote monitoring, will earn US$ 1.2 billion of net income annually. This market will grow from US$ 1.4 billion in 2010 to US$ 2.6 billion in 2014; this means a 12.5% increase every year [5]. In addition, it is expected that new job opportunities will exist for 39,000 people by 2014. Until now, u-health has been used for telemedicine and as an instrument in home healthcare for patients who have chronic diseases, by means of biosensor devices. Patients monitoring their conditions through u-health services measured their own biometric data, including temperature, blood pressure, pulse, weight, blood sugar, body fat, electrocardiograms, and clinical tests using blood and urine.
It has been proven that telemedicine or telecare services are effective for diabetes [1,6-9], hypertension [10,11], tuberculosis [12], asthma [13], metabolic syndrome [14,15], and quitting smoking [16]. U-health methods to manage or monitor chronic disease are regarded as useful to improve health status and lower medical expenditures [17,18]. However, confirmation of whether u-health services based on ubiquitous technology would also be effective to manage chronic disease in rural Korea is to be determined.
The purpose of this study is to analyze the effectiveness of u-health services for managing people with metabolic syndrome in a health center in Korean county (gun).
The South Korean Ministry of Health and Welfare (MOHW) have been experimenting with the management of metabolic syndrome in a trial project using u-health devices and systems at the community level. The service was targeted at people aged over 20 with risk factors for metabolic syndrome in households with less than the average monthly income.
The trial project ran for six months in an urban-rural complex in Korea. It included periodical health assessment, consultation about healthy lifestyles, nutrition programs, and exercise, all using the u-health device. The main point of u-health is to provide customized healthcare services for individuals, consulting services for patients, programs for self-health management with a 24-hour monitoring target and feedback to patients on health examination results.
Subjects' bio-signals were measured daily through u-health devices such as 3D passometers, body-composition analyzers, and sphygmomanometers. The measured data were transmitted to a u-health database. A clinical-decision support system (CDSS) analyzed the data in real time and sent the information to the individual concerned directly by phone call or web service. Phone calls were made by u-health consultants: two exercise therapists and two dietitians (Figure 1).
We applied the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) standards [19], which are used to decide whether an individual has metabolic syndrome: body fat (waist greater than 90 cm in a man and greater than 85 cm in a woman), high neutral fat (greater than 150 mg/dL), low high-density lipoprotein cholesterol (less than 40 mg/dL), blood pressure (above 130 mmHg of systolic blood pressure; above 85 mmHg of diastolic blood pressure), and fasting blood sugar (greater than 100 mg/dL). Anyone who meets more than one of these conditions is considered to have metabolic syndrome.
We implemented the project using a one-group posttest-only design [20].
The subjects were 316 residents in county A who had been medically diagnosed with metabolic syndrome and earned less than the average national monthly income. We collected biometric data on subjects twice using u-health devices: before and six months after the implementation of u-health services. We surveyed the data about their health on the same schedule.
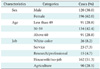
The sample comprised of 38.0% male, 42.4% people in their fifties, and 51.3% housewives and people without regular paid work (Table 1).
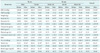
Basic biometrics for the subjects, who used u-health services to track the state of their metabolic syndrome for six months, improved significantly in that time: blood pressure, weight, abdominal visceral fat, physical age, the extent of walking, waist size and blood sugar (p < 0.01); body fat and BMI (p < 0.05); and body fat (triacylglycerol; p < 0.1) (Table 2).
We analyzed BMI change over time using a latent growth model. The most useful model for tracing BMI by time was a second-year model. Its mean for the first year was 26.00, and variance was 16.19%. Mean BMI change rate was -0.48, and variance was 2.56. Model fit was appropriately high: NFI (0.982), TLI (0.975), CFI (0.987), and RMSEA (0.085). Covariance between initial BMI value and rate of change was -3.48 (Figure 2).
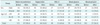
The number of people with biometric data indicating a likelihood of metabolic syndrome decreased after using the u-health service. After six months of u-health, subjects that showed one or more biometric indicator for metabolic syndrome decreased by 24.5% (from 204 to 154 people). The number of people with two or more biometric indicators of metabolic syndrome decreased by 45.7% (from 151 to 82 people). The number of people with three or more biometric indicators decreased by 62.5% (from 88 to 33 people), and the number with four or more indicators decreased by 81.8% (from 33 to six people). The number of people who showed five biometric indicators of metabolic syndrome decreased by 100% (from five to zero). Biometric data overall decreased more than 16%: high blood pressure decreased 73.5%, body fat 49.4%, HDL-C 35.4%, blood sugar 20.5%, and neutral fat 16.0% (Table 3).
Drinking behavior improved owing to u-health services. The number of people who used to drink alcohol once or twice a week drank 49% and 63.3% less alcohol after three and six months respectively. People who used to drink three to five times a week also drank 22.2% less alcohol three months later and 37.0% less alcohol six months later. The number of people who used to drink six or seven times in a week also drank 10.0% and 40.0% less alcohol three and six months later, respectively (Table 4).
Although frequency of exercise showed less change than the drinking behavior, it also improved after u-health. Three months after beginning u-health, 50.0% of people who did not exercise before the service had started to exercise more than twice a week. Six months later, that figure was 83.3% (Table 5).
With regard to smoking behavior, 79.3% of smokers had quit after three months and 39.1% after six months (Table 6).
This research has intended to reveal whether u-health services could be useful for improving and changing the health status and behavior of people who are living in South Korean urban-rural complexes and diagnosed with metabolic syndrome. It was proven that u-health services are effective for managing the health status of people with metabolic syndrome, although there was not strong evidence for this in the previous research. Some previous research on diabetes showed a blood sugar decrease from 9.7% to 13.2% [1,7], but other research [16] showed no difference in it. In the context of hypertension, the u-health service was effective in promoting adherence to its plan [11]. It was proven that u-health was effective in ameliorating metabolic syndrome by decreasing HbA1C (Glycated hemoglobin), TC, TG, and HDL-C [14,15]. It has also been shown that u-health decreases NRT adherence rate [16], HbA1C, TC, TG, HDL-C, waist size, weight, and BMI [11]. Therefore, we suggest that some u-health service models can effectively align with the offline healthcare programs or services in rural areas, including consulting or education services for patients who have chronic diseases, nonsmoking promotion services, personalized and visiting health-management services, preventive services for chronic diseases, emergency healthcare service for the aged living alone and for people with senile dementia, and care services for children who are obese.
There are differences in the settings between our u-health services and those in the previous research that did not show beneficial effects. We believe that u-health services with appropriate devices and systems can be useful and effective to manage the health of people with metabolic syndrome.
Some limitations of this study should be acknowledged. The first limitation involves the fact that this study used a one-group posttest-only design, that is, we could not be sure of the pure effect of u-health services, because the influence of exogenous variables such as self-care, medical treatment, and other voluntary activities was not controlled for [20]. The second limitation is that we did not compare the results of the present study with those that can be gleaned by other methods.
The present study provides a case of effective management of metabolic syndrome using the u-health method. The findings indicate that real-time information and consultation about health status and behavior can be useful in managing metabolic syndrome. In particular, u-health systems played an important role in measuring bio-information using a u-health device, analyzing the information, and communicating the results and implications to subjects. However, it is important for future research to compare this line of study to other candidate methods. Furthermore, research should also control for exogenous factors, as discussed above.
Figures and Tables
References
1. Ahring KK, Ahring JP, Joyce C, Farid NR. Telephone modem access improves diabetes control in those with insulin-requiring diabetes. Diabetes Care. 1992. 15:971–975.

2. Statistics Korea. Complete enumeration results of the 2010 population and housing census. 2011. Daejon, KR: Statistics Korea.
3. Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010. 79:736–771.

4. BBC Research. Healthcare information system. 2006. Denver, CO: BBC Research.
5. Lee YT, Kim MS, Kim SH, Kim SY. A study of business strategy on U-health industry. 2010. Cheongwon, KR: Korea Health Industry Development Institute.
6. Benhamou PY, Melki V, Boizel R, Perreal F, Quesada JL, Bessieres-Lacombe S, Bosson JL, Halimi S, Hanaire H. One-year efficacy and safety of Web-based follow-up using cellular phone in type 1 diabetic patients under insulin pump therapy: the PumpNet study. Diabetes Metab. 2007. 33:220–226.

7. Cho JH, Kwon HS, Yoon KH. Perspectives of "ubiquitous health care system" for diabetes management. J Korean Diabetes Assoc. 2006. 30:87–95.

8. Sacco WP, Morrison AD, Malone JI. A brief, regular, proactive telephone "coaching" intervention for diabetes: rationale, description, and preliminary results. J Diabetes Complications. 2004. 18:113–118.
9. Vahatalo MA, Virtamo HE, Viikari JS, Ronnemaa T. Cellular phone transferred self blood glucose monitoring: prerequisites for positive outcome. Pract Diabetes Int. 2004. 21:192–194.

10. Marquez Contreras E, de la Figuera von Wichmann M, Gil Guillen V, Ylla-Catala A, Figueras M, Balana M, Naval J. Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phone (HTA-Alert). Aten Primaria. 2004. 34:399–405.
11. Park MJ, Kim HS, Kim KS. Cellular phone and internet-based individual intervention on blood pressure and obesity in obese patients with hypertension. Int J Med Inform. 2009. 78:704–710.

12. DeMaio J, Schwartz L, Cooley P, Tice A. The application of telemedicine technology to a directly observed therapy program for tuberculosis: a pilot project. Clin Infect Dis. 2001. 33:2082–2084.

13. Ostojic V, Cvoriscec B, Ostojic SB, Reznikoff D, Stipic-Markovic A, Tudjman Z. Improving asthma control through telemedicine: a study of short-message service. Telemed J E Health. 2005. 11:28–35.

14. Kim HS, Song MS. Technological intervention for obese patients with type 2 diabetes. Appl Nurs Res. 2008. 21:84–89.

15. Kim SI, Kim HS. Effectiveness of mobile and internet intervention in patients with obese type 2 diabetes. Int J Med Inform. 2008. 77:399–404.

16. Brendryen H, Kraft P. Happy ending: a randomized controlled trial of a digital multi-media smoking cessation intervention. Addiction. 2008. 103:478–484.

17. Kim KH, Lee MO, Lee JG, Ryu S. Compliance of hypertensive patients registered in primary health care posts implementing the Gangwon telemedicine service system. J Korean Soc Health Inf Health Stat. 2008. 33:59–76.
18. Bergmo TS. Can economic evaluation in telemedicine be trusted? A systematic review of the literature. Cost Eff Resour Alloc. 2009. 7:18.

19. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001. 285:2486–2497.
20. Chae SI. Survey methodology in social science. 2005. 3rd ed. Seoul, KR: B&M Books.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download