Abstract
Objectives
To examine the current status of hospital information systems (HIS), analyze the effects of Electronic Medical Records (EMR) and Clinical Decision Support Systems (CDSS) have upon hospital performance, and examine how management issues change over time according to various growth stages.
Methods
Data taken from the 2010 survey on the HIS status and management issues for 44 tertiary hospitals and 2009 survey on hospital performance appraisal were used. A chi-square test was used to analyze the association between the EMR and CDSS characteristics. A t-test was used to analyze the effects of EMR and CDSS on hospital performance.
Results
Hospital size and top management support were significantly associated with the adoption of EMR. Unlike the EMR results, however, only the standardization characteristic was significantly associated with CDSS adoption. Both EMR and CDSS were associated with the improvement of hospital performance. The EMR adoption rates and outsourcing consistently increased as the growth stage increased. The CDSS, Knowledge Management System, standardization, and user training adoption rates for Stage 3 hospitals were higher than those found for Stage 2 hospitals.
Hospital information systems (HIS) are being increasingly adopted by hospitals with the evolution of information technology (IT). The effective use of HIS reduces costs and improves patient care in the healthcare industry. According to a nationwide survey on HIS development in 2005 [1], almost all Korean tertiary hospitals were equipped with Computerized Provider Order Entry (CPOE) System, Picture Archiving and Communication System, insurance claims by Electronic Data Interchange, and admission/discharge/transfer. However, only 9 hospitals (21.43%) had adopted Electronic Medical Record. These systems fall into the category of transaction processing systems (TPS), which are focused on reducing the waiting time for outpatients and length of hospital stay, and increasing hospital revenues [2].
Unlike TPS, decision support systems (DSSs) are focused on improving the quality of decisions made by doctors and managers. Examples of DSSs are Clinical DSS (CDSS) for diagnosing diseases or prescribing medicine and Knowledge Management Systems (KMS) for financial management and marketing analysis. CDSS is defined as: 'providing clinicians or patients with computer-generated clinical knowledge and patient-related information, intelligently filtered or presented at appropriate times, to enhance patient care [3]. DSSs are generally integrated with a data warehouse, which is a comprehensive data repository of decision-oriented information. According to the 2005 survey, only a few hospitals had adopted DSSs and data warehouse, perhaps due to the following underlying barriers. Unlike TPS, DSSs are not easily adopted by hospitals due to difficulties in justifying their outcome and economic return. Moreover, their use is not compulsory. That is, doctors do not rely on CDSS to diagnose or prescribe medicine and planning staffs are not required to use KMS to analyze the hospital market or customer behavior. Since DSSs can be more easily developed if there is sound IT infrastructure such as data warehouse or EMR, the increasing adoption of such infrastructure by hospitals necessitates an examination of KMS adoption.
The Ministry of Health and Social Welfare has launched a hospital performance evaluation project since 2004 in an effort to improve the quality of hospital services and patient management. All hospitals have to be evaluated every three years in the areas such as clinical care, quality of care, clinical information, emergency care, lab, and drug information [4]. While several studies have analyzed the effects of HIS on patient waiting time, length of stay, and medication errors, no study has been conducted to examine the effects of HIS on hospital performance in Korea.
IT has also created various management issues for hospitals. EMR has changed workflow processes, resulting in the reduction of jobs and changes in the roles of key players such as physicians, nurses, and administrative staffs. Problems have arisen due to the lack of system knowledge and increased workloads for physicians and nurses as they have to manually enter all of their orders into the system. In the study on the barriers and solutions for use of EMR, Miller and Sim [5] found that underlying barriers for EMR were: difficulties with technology, complementary changes, and physicians' attitudes. Kim et al. [6] and Kwak et al.[7] conducted surveys on key management issues for Korean HIS in 1999 and 2006 by targeting hospital IT managers using three-round Delphi surveys. Key management issues identified by two surveys were: top management, standardization, regulations on EMR, user training, outsourcing, security policy, and information strategy planning.
IS are greatly affected by the rapid development of IT. Gibson and Nolan [8] categorized the stages in the growth of IS into four stages from initiation to maturity as IT changes. They also recommended how each stage can be applied, as well as management issues that can emerge in each developmental stage. Nolan [9] introduced a six-stage model theory, which later expanded further into nine stages. Since Nolan's stages of growth were introduced three decades ago, several revisions have been made to the model. Earl [10] applied the stages of growth model for e-business. Earl proposed the six-stage model for e-business that corporations are likely to experience. Gottschalk [11] has linked the information technology support for knowledge management in law firms to four stages of growth. This study analyzed the temporal changes in HIS development activities and management issues from the very beginning of the HIS implementation in order to examine whether Nolan's stage theory holds for a hospital setting.
The study purposes were to examine the current status of HIS, analyze the effects of EMR and CDSS on hospital performance, and examine how management issues change according to the growth stages.
HIS adoption status and management issues were obtained from a survey conducted for all 44 tertiary hospitals in Korea from October 1 to 30, 2010. Hospital performance scores were obtained from the hospital performance appraisal survey conducted by the Korea Health Industry Development Institute in 2009 [4].
The association between the adoption of EMR/CDSS and hospital characteristics were analyzed by chi-square test. The effect of EMR/CDSS on hospital performance was analyzed by t-test. The hospital performance score was obtained by adding performance scores from six areas related to EMR/CDSS [4]: clinical care, quality of care, clinical information, emergency care, lab, and drug information. Statistical analysis was performed by the Statistical Analysis System (SAS ver. 9.2, SAS Institue, Cary, NC, USA).
In order to examine the temporal changes in HIS development activities and management issues, hospitals were grouped into one of three growth stages based on the year of HIS initiation: 1996-2010 (stage 1), 1986-1995 (stage 2), and before 1986 (stage 3). Specifically, this study surveyed the hospitals in each stage to determine exactly which had more advanced HIS applications (e.g., EMR, CDSS, and KMS) and more mature management policies (e.g., top management support, standardization, user training, and out-sourcing). According to the Nolan's stage theory, the hospitals in stage 3 are assumed to have more advanced HIS applications and more mature management policies that the hospitals in stages 1 and 2.
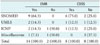
As seen in Table 1, every hospital had adopted CPOE. The adoption rate of EMR had greatly increased from 21.4% in 2005 to 77.3% in 2010. Compared to adoptions in 2005, adoption of DSSs had also greatly increased in 2010. The adoption rate for CDSS was 27.3%. Adoption rates for DSS for management, KMS was 29.4%. None of these DSSs had been implemented in 2005. 21.9% of the hospitals had also adopted the data warehouse.
As seen in Table 2, hospital size and top management support were significantly associated with EMR adoption. The percentage of EMR adoption increased with increasing hospital size. With strengthening top management support, the percentage of EMR adoption also increased since EMR adoption requires large capital investment. While the other characteristics (ownership, location, and standardization) were not significantly associated with the EMR adoption, foundation-owned hospitals located in Seoul and other metropolitan areas, and hospitals that had adopted standardization had higher EMR adoption rates.
As seen in Table 3, only standardization was significantly associated with CDSS adoption. Standardization refers to the hospitals that had adopted standard terminology to develop EMR or CDSS. Eight hospitals (66.7%) developed CDSS by using standard terminologies. Adoption of CDSS were higher for hospitals with over 800 beds, foundation-owned hospitals, public hospitals, and hospitals located in Seoul than the hospitals that did not adopt CDSS.
As seen in Table 4, three types of standard clinical terminology were used by 14 (29.5%) hospitals. Systematized Nomenclature of Medicine-Clinical Terms (SNOMED-CT) was utilized by the majority of hospitals. Nine hospitals (64.3%) used it to develop EMR and eight hospitals (75%) used it to develop CDSS. Two hospitals used Unified Medical Language System (UMLS) and thee hospitals used International Classification of Nursing Practice (ICNP).
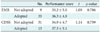
The EMR-adopted hospitals had higher performance scores than those hospitals that had not adopted EMR although difference was not statistically significant (Table 5). Similarly, those hospitals that had adopted CDSS had higher performance scores than those that had not adopted CDSS. These findings suggest that both EMR and CDSS influenced the improvement of hospital performances.
Adoption rates of EMR and outsourcing consistently increased as growth stage increases although the association between the two factors was not statistically significant; hospitals are likely to adopt EMR and outsource as they have more experience of implementing information systems (Table 6). Hospitals in stage 3 also had the highest adoption rates of KMS and user training. On the other hand, hospitals ins 1 had the highest adoption rates of CDSS and standardization.
In this study, the status of HIS, effects of EMR/CDSS on hospital performance, and changes in management issues over time were examined. Adoption rate of EMR has greatly increased from 21.4% in 2005 to 77.3% in 2010. Compared to rate in 2005, adoption of clinical and managerial DSSs has also greatly increased in 2010. Data warehouse was also adopted by similar number hospitals (21.9%). Increase in adoption of DSSs may be explained by the adoption of EMR and data warehouse which provide key information to them. Use of an EMR is the first step toward CDSS.
Factors associated with the adoption of EMR were investigated. Hospital size was the only significant factor associated with the adoption of EMR. As hospital sizes got bigger, the adoption rate of EMR increased to increase efficiency of hospital operation and patient management. Robles [12] reported that EMR improves efficiency of work performance, communication among health professionals, thus reducing duplicate entries, and speeding-up flow of information. Characteristics, such as ownership, location, top management support, and standardization, were not significantly associated with the EMR adoption. Hospitals owned by private foundation, hospitals located in metropolitan, including Seoul, hospitals that have strong top management support, and adopted standard terminology showed to have higher EMR adoption rates. Strong top management support was associated with EMR as hospitals face enormous financial challenges in adopting EMR. Poon et al. [13] reported that only large institutions could afford to implement EMR because of the large upfront investments necessary to deploy EMR. Adler-Milstein et al. [14] also reported that large investment was the biggest obstacle in the adoption process of EMR.
Unlike EMR, standardization was the only significant factor associated with the CDSS adoption. This may be explained by the fact that CDSS can be more effectively developed and used by clinicians if it is developed based on the standard clinical terminologies. Top management support was not strongly associated with the adoption of CDSS as it does not require large initial investment as EMR.
Both EMR and CDSS influenced the improvement of hospital performances. The results are consistent with previous studies in EMR and CDSS. EMR improves patient safety and quality of clinical services [15]. Florez-Arango et al. [16] reported of an increased adherence to guidelines by healthcare workers using CDSS's on mobile devices in a controlled experimental setting. CDSS also reduced serious medication error rates by 55% in one study [17].
This study also analyzed the temporal changes in HIS development activities and management issues from the very beginning of the HIS implementation in order to examine whether Nolan's stage theory holds for a hospital setting. Adoption rates of EMR and the percentage of outsourcing consistently increased as the growth stage increases although the association between the two factors was not statistically significant. Hospitals in stage 3 also had the highest adoption rates of KMS and user training. Ryu and Kim [18] stated that user training is critical to increase computer self-efficacy and to maximize the use of information systems. On the other hand, hospitals in stage 1 had the highest adoption rates of CDSS and standardization. As aforementioned, standardization provides a key infrastructure for CDSS. This finding suggests that hospitals are likely to adopt information systems to increase efficiency in hospital management and that they increasingly emphasize importance of HIS management as they have more experience of implementing HIS.
There were several limitations to this study. There were some missing values in user training and outsourcing variables. Future research should increase the number of respondents by including face-to-face interviews in addition to the mail-out surveys. In addition, more in depth study should be conducted to accurately segment hospitals into growth stages as some initial conditions adapted from Nolan's study do not perfectly suit with the conditions of Korean hospitals.
Figures and Tables
References
1. Chae YM, Kang SW, Wang KH. Status of computerization at health institutes in Korea. 2005. Seoul: Korea Health Insurance Review Agency.
2. Park WS, Kim JS, Chae YM, Yu SH, Kim CY, Kim SA, Jung SH. Does the physician order-entry system increase the revenue of a general hospital? Int J Med Inform. 2003. 71:25–32.

3. Osheroff JA, Pifer EA, Teich JM, Sittig F, Jenders RA. Improving outcomes with clinical decision support: an implementer's guide. 2005. Chicago: Healthcare Information and Management Systems Society.
4. Ministry of Health and Welfare. Hospital performance appraisal survey. 2009. Seoul: Ministry of Health and Welfare.
5. Miller RH, Sim I. Physicians' use of electronic medical records: barriers and solutions. Health Aff (Millwood). 2004. 23:116–126.

6. Kim JE, Chae YM, Kim NH. Study of management issues in hospital information systems using Delphi method. Paper presented at: 15th Spring Conference of the Korean Society of Medical Informatics. 2002 Jun 14; Seoul, Korea.
7. Kwak EA, Chae YM, Ho SH, Kim KK. Key issues of hospital information systems management. J Korean Soc Med Inform. 2007. 13:9–17.

8. Gibson CF, Nolan RL. Managing the four stages of EDP growth. Harv Bus Rev. 1974. 52:76–88.
9. Nolan RL. Managing the crises in data processing. Harv Bus Rev. 1979. 57:115–126.
11. Gottschalk P. Toward a model of growth stages for knowledge management technology in law firms. Informing Sci. 2002. 5:79–93.

12. Robles J. The effect of the electronic medical record on nurses' work. Creat Nurs. 2009. 15:31–35.

13. Poon EG, Jha AK, Christino M, Honour MM, Fernandopulle R, Middleton B, Newhouse J, Leape L, Bates DW, Blumenthal D, Kaushal R. Assessing the level of healthcare information technology adoption in the United States: a snapshot. BMC Med Inform Decis Mak. 2006. 6:1.

14. Adler-Milstein J, McAfee AP, Bates DW, Jha AK. The state of regional health information organizations: current activities and financing. Health Aff (Millwood). 2008. 27:w60–w69.

15. Zlabek JA, Wickus JW, Mathiason MA. Early cost and safety benefits of an inpatient electronic health record. J Am Med Inform Assoc. 2011. 18:169–172.

16. Florez-Arango JF, Iyengar MS, Dunn K, Zhang J. Performance factors of mobile rich media job aids for community health workers. J Am Med Inform Assoc. 2011. 18:131–137.

17. Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, Burdick E, Hickey M, Kleefield S, Shea B, Vander Vliet M, Seger DL. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998. 280:1311–1316.

18. Ryu I, Kim M. An empirical study on the success factors and performance model of hospital information systems. Asia Pac J Inform Syst. 2002. 12:45–65.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download