Abstract
Objectives
The objective of this research is to introduce the unique approach of the Catholic Medical Center (CMC) integrate network hospitals with organizational and technical methodologies adopted for seamless implementation.
Methods
The Catholic Medical Center has developed a new hospital information system to connect network hospitals and adopted new information technology architecture which uses single source for multiple distributed hospital systems.
Results
The hospital information system of the CMC was developed to integrate network hospitals adopting new system development principles; one source, one route and one management. This information architecture has reduced the cost for system development and operation, and has enhanced the efficiency of the management process.
Conclusions
Integrating network hospital through information system was not simple; it was much more complicated than single organization implementation. We are still looking for more efficient communication channel and decision making process, and also believe that our new system architecture will be able to improve CMC health care system and provide much better quality of health care service to patients and customers.
Go to : 
Information system is rising as an important tool for improving quality of health care services with unique features for shaping organizational culture, automating processes, and creating close relationship. When the new information technology (IT) architecture is created and implemented throughout the organization, health care organizations can improve stability [1-4]. Yonsei University Health Care System has once implemented u-Severance information system focusing on electronic hospital records and enhance the efficiency in management and customer satisfaction [5]. The Catholic Medical Center has also developed and adopted a new IT architecture in order to address major ineffective elements for its intrinsic benefits.
The CMC was originally established in 1932 to train gifted doctors, research and develop medicines, and provide humanitarian medical services. The CMC began healthcare service with only 15 health care professionals and 24 beds. As Seoul St. Mary's hospital opened with cutting-edge facilities including 22 floors, 6 basements, 1,200 patient beds and around 3,200 healthcare service professionals in 2009, this center became the largest medical network hospital in Korea comprising of 8 hospitals and about 5,000 beds. [6].
Since 2005, the CMC decided that information technology can be the important tool to gain its competitiveness in rapidly changing healthcare market as well as economic and social business environment. The basic philosophy of this new system is based on the Catholic spirit in healing sick people with great compassion in the name of Jesus. From this perspective, the nU (neuro-Ubiquitous) system, CMC's new hospital information system, was developed. The development of the nU system connecting eight hospitals is perceived as an important infrastructure to develop health care network, improve inter-relationship between subsidiary hospitals and transform information flow into the mutual rapport based on the Catholic spirit. It is a unique approach in healthcare organization and is the first example implementing single information technology architecture in Korea.
Currently, nU system architecture has been deployed throughout five network hospitals, Uijeongbu St. Mary hospital, Bucheon St. Mary's hospital, Yeouido St. Mary's hospital, and St. Paul's hospital starting from Seoul St. Mary hospital in 2009. In implementing in other network hospitals, we found out that much more strategic, organizational as well as technical factors should be carefully considered than implementing in a single organization.
The objective of this research is to introduce our single source based information systems integrating CMC network hospitals. In addition, our unique approach for organizational and technical alignments adopted to mitigate risks will be discussed. Our experiences will be helpful for integrating network hospitals to implement HIS in the forthcoming future. In the next section, we examine how the information system strategy connecting network hospitals has been developed and discuss some of the key distinctions of the nU system. The article concludes by presenting implications and drawbacks in integrating network hospitals.
Go to : 
As The Hospital Environment Is Getting More Competitive, A Strategic Decision Is Necessary To Move Forward To The Leading Position For Providing Better Health Care Service. In 2005, To Address The Changing Environment, The Cmc Announced The New Vision As "the Life Admiring And Global Leading Hightech Healthcare Service". To Implement Its New Vision, The Management Focused On Integrating Each Individual Capability, Which Is Spread Out Among The Cmc Network Hospitals. Information Systems Have Played Major Role To Integrate Hospital [7]. Information Systems Are Identified As The Best Tool To Accomplish Its New Vision And Inter-connect Network Hospitals. As A Starting Point For The Strategic Information System Architecture, The Isp Project Has Been Conducted. Isp Is The Methodology For Developing Strategic It Plan With The Analysis Of The Internal And External Business Environment [8]. The Followings Are Major Problems Founded From The Isp Projects.
ISP project team analyzed the current business processes at the same department level of eight network hospitals and found out several ineffective factors to be revised.
First, the same statistical and administrative data were separately generated and managed redundantly at different departments even within one hospital as well as among different hospitals. Secondly, review and decision-making between central medical center and subsidiary hospitals were carried out redundantly. Third, information could not be shared among relevant departments and/or provided on time to authorized staff members in an appropriate and usable form. These results showed that IT architecture should be redesigned so that important information could be correctly collected, stored, processed, and systematically documented to ensure that correct, pertinent, and up-to-date patient information to be supplied to the physicians or nurses within one hospital as well as among different hospitals within the center.
It was the "Information Support" team at the CMC as well as each hospital which was responsible for the centralized management of information system. The team worked for integrating information management process of eight hospitals. They held regular meeting semi-weekly to discuss emergent issues and operating status of the HIS. However, strategic directions on the information system could not be provided on time for the timely decision due to the lack of dedicated IT professions. Redesigning of IT organization was necessary at the central level and at the department level to gain the centralized competency and effective management.
Information requirements were collected and managed separately at each hospital, and also the system development requirements were separately fulfilled in each hospital level. Redundant requirements for the information system development finally increased overall development backlog and users complaints because information requirement could not be met on time.
Access to the health record database must be limited to authorized individuals, and the appropriate security measures were needed to ensure data integrity. However, each hospital had its own system access procedure and practices which caused the uncontrollable system access into the database. Therefore, centralized procedures and controls should be put in place to prevent the altering, browsing, querying, or reporting of secured data.
Based on the analysis of the current business and IT environment from the ISP project, the current information architecture was found to provide poor effectiveness and extensibility. Thus, a new IT architecture should be proposed to address the aforementioned issues.
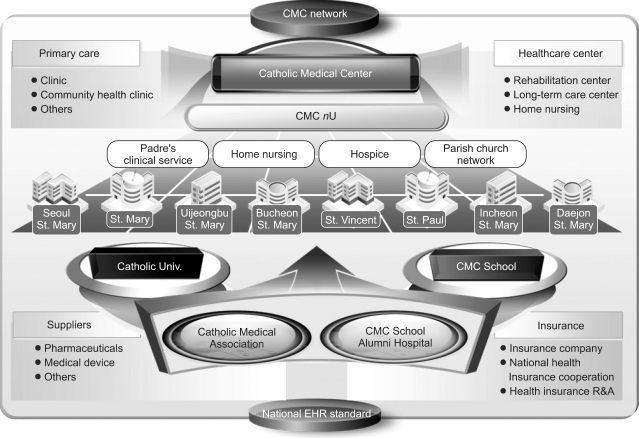
The new CMC hospital information system called as "nU" system, aimed to facilitate patient information management and holistic medical treatment through effective data sharing among hospitals ("nU" is the abbreviation for "neuro-Ubiquitous"). It is a ubiquitous system based on a network like the nervous system. There are three main objectives of nU System (Figure 1).
First, new system should solidify a collaborative network of hospitals through the unified process of CMC-affiliated hospitals. Data and process integration can help hospitals to build a collaborative relationship; it should include not only standardized source code and data but also health care process.
Second, patients can be able to connect with hospital professionals at the remote, priests serving for the sick and the poor within the hospital, and home nursing care service providers for better health care service based on catholic philosophy. The new system allows them to access the system for the better care service.
Third, the overall costs for developing and operating the information system should be reduced. Integrating dispersed IT resources in all over the hospitals can help reducing IT-related costs.
Go to : 
The integrated system can lead to cost reduction and health care quality improvement. To actually achieve positive effects, however, it is of paramount importance to evaluate current health care service, redesign existing process, and establish new organization from the patient's perspective. CMC prepared a list of prerequisites for developing and managing integrated systems of 8 hospitals.
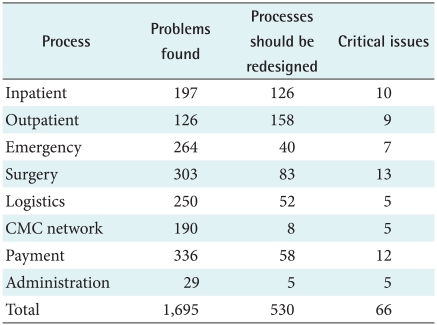
The Mega Business Process Reengineering (M-BPR) project was conducted to make better standardized process for eight areas; inpatient, outpatient, emergency, surgery, logistics, CMC network, payment, and administration. A total of 1921 people were involved in BPR team, with 121 meetings and workshops. All 1,695 problems were found and 530 creative processes were suggested for redesigning (Table 1).
After Mega BPR, working level professionals in each organization were involved in functional BPR for 39 particular processes. A total of 297 meetings were held by 3,048 people in 36 teams within the f-BPR. Finally, 175 tasks were executed and 240 issues were resolved.
Health information systems transitionally tends to be fragmented, incomplete and isolated. To communicate and exchange data accurately among each hospital, CMC standardized the forms, codes and clinical terminologies including priests' terminologies.
CMC began to standardize terminologies, forms, addresses, names of operations and diagnosis in 2006. The primary step was to investigate the medical charts from 8 hospitals, collect 220,492 terms of diagnosis, 64,556 terms of surgery and 39,859 terms of chief complaints, and then remove duplicated words and acronyms. As a result, 73,356 terms of diagnosis, 29,896 terms of surgery and 20,000 terms of chief complaints were selected. Selected terminologies were mapped with SNOMED-CT (Systematized Nomenclature of Medicine-Clinical Terms), the global medical standard terminology-then was mapped with ICD-9-CM (International Classification of Diseases-9-Clinical Modification extensions) and KCD-4 (Korean Standard Classification of Diseases-4). Standardization enables CMC hospitals to share and interchange patients' records, for becoming the basis of the data utilization to improve the treatment quality.
CMC established the centralized organization for data integration and system management. The CMC nU Integrated Information Committee was the highest decision making organization to decide priorities of issues collected from 8 hospitals for CMC nU, and establish the direction for development and maintenance of EMR system.
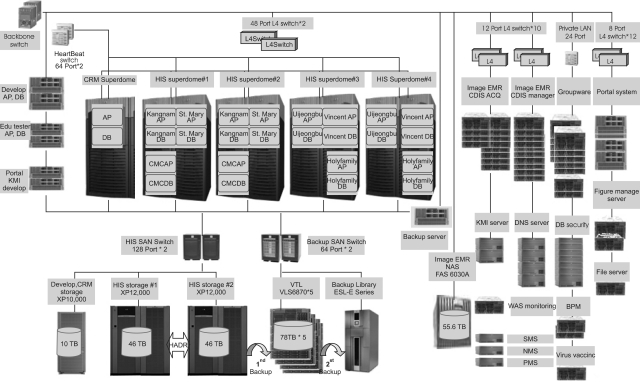
CMC nU system is physically separated. However, it is logically integrated by the central center. "3 ones principle" is considered a fundamental principle for realizing the system and consists of "One-source", "One-route", and "One-management". "One-source" means managing 8 hospitals with a unified source. "One-route" means establishing a consistent strategy of hospital information system by unifying communication path. And "One-management" aims to enhance operational efficiency by centralizing the management of hospital information system. This architecture will support the stability, efficiency and economic feasibility (Figure 2).
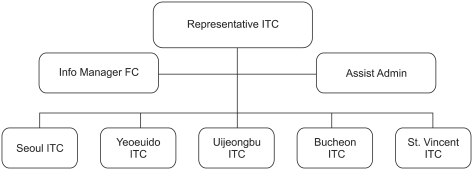
Information technology coordinators (ITC) consisting of 97 on hand workforces from 47 departments were organized. The roles for ITC are drawing agreement on issues and changes about nU programs from each hospital's department, maintaining standardization and managing nU program centrally. ITC arbitrates practical tasks, processes, IT environment and visions of each department to apply these aspects on to divisional nU system. ITC conducts training for users and deals with departmental issues (Figure 3).
Internet Data Center (IDC) was established to manage information resources at the central level. Information resources from 5 hospitals were integrated in IDC with a plan to be extended to other hospitals as well. The roles of IDC are to manage those aspects related with information resources such as network, integrated security, and resources management.
Since our nU systems use the common business process for all different hospitals, the same department of network hospitals should adopt the agreed business process as well. If a hospital wants to change specific business process, all other hospitals should come to an agreement about the change. During this process, participants try to learn and adopt the best practice from other hospitals. Groupware and messenger programs have played a major role in obtaining agreement easily through discussion.
Centralized data center can reduce the cost of information system development and operation. While implementing HIS in five hospitals, labor cost was reduced to around 8.2%. As more hospitals start using the system, cost reduction rate is expected to increase.
Generally, it takes almost two years for a hospital to stabilize its operation through typical HIS development. Our approach took only five to seven months to implement into one hospital. The speed of implementation will accelerate as the system expands into other hospitals.
System bugs and errors, which were not easily detected before, are recognized and resolved with less effort and applied to other hospitals without additional request. Our approach allowed for easy detection and efficient resolution of the system errors.
Medical faculty and trainee of the CMC are rotating among eight network hospitals. When the information system of each hospital was different, it took a considerable amount of time for staffs to be accustomed to local information and process. Once the system is integrated, the confusion derived from job rotation will be decreased and faster adoption will occur.
Previously, when government insurance policy was changed, each hospital had to independently modify their system according to the regulation change. The new nU system enables hospitals to obtain overall reflection of policy change for the system thus resulting in reduction of labor efforts.
Go to : 
IT had played a reactive role in responding to the current healthcare services. HIS is the socio-technical subsystem of a hospital, which comprises all information processing as well as the associated human or technical factors in their respective information processing [5]. During the implementation period for expanding into other hospitals, there found some problems as follows.
First, since the decision was made based on agreement, it usually took longer than a single hospital's decision making process. Second, usually inter-departmental communication within one hospital had not been conducted smoothly. Communication between same departments among eight hospitals created even more issues and difficulties to come to conclusion. Misunderstanding and misinterpretation created during the discussion of the same issue interfered with the system development. What is worse is the conflict with top managements. Sometimes top managements put pressure on the development team even with unaccepted requirements.
However, as time passed by, the conflict has been resolved and more reasonable decision was being made. People come to learn how to communicate with others within hospital and among other hospitals. Furthermore, people learn mutual respect and look at the hospital process from the broader perspective. In addition, top managements come to understand the process more and suggest better resolution.
The CMC tried to develop HIS comprising IT architecture, organizational structure and business process to develop health network throughout the same network medical center. Integrating network hospital through information systems was not simple; it was much more complicated than single organization implementation. We are still looking for an efficient communication channel and decision making process. Even though the integration process has been very tough, we believe that our new IT architecture would be able to provide more enhanced health care service for patients and customers without geographical boundaries and seamless linkages connecting CMC network hospitals.
Go to : 
References
1. Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. 2001. Washington: National Academy Press.
2. Balas EA, Austin SM, Mitchell JA, Ewigman BG, Bopp KD, Brown GD. The clinical value of computerized information services. A review of 98 randomized clinical trials. Arch Fam Med. 1996; 5:271–278. PMID: 8620266.

3. Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009; 360:1628–1638. PMID: 19321858.

4. DesRoches CM, Campbell EG, Rao SR, Donelan K, Ferris TG, Jha A, Kaushal R, Levy DE, Rosenbaum S, Shields AE, Blumenthal D. Electronic health records in ambulatory care: a national survey of physicians. N Engl J Med. 2008; 359:50–60. PMID: 18565855.
5. Chang BC, Kim NH, Kim YA, Kim JH, Jung HK, Kang EH, Kang HS, Lee HL, Kim YO, Yoo SK, Sunwoo I, An SY, Jeong HJ. Ubiquitous-Severance hospital project: implementation and results. Healthc Inform Res. 2010; 16:60–64.

6. Catholic Medical Center [Internet]. cited 2010 Jun 20. Seoul: The Catholic University of Korea, Catholic Medical Center;Available from:
http://www.cmc.or.kr/global/eng/front.
7. Haux R, Winter A, Ammenwerth E, Brigl B. Strategic information management in hospitals: an introduction to hospital information systems. 2003. NY: Springer;p. 177–220.
8. Martin J. Information engineering. Book I: Introduction. 1989. Englewood Cliffs (NJ): Prentice-Hall, Inc..
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download