Introduction
Group A streptococcus (GAS), or
Streptococcus pyogenes, is a facultative, Gram-positive coccus which causes a wide range of diseases in humans, from mild to life-threatening ones, such as pharyngitis, scarlet fever, tonsillitis, cellulitis, impetigo, erysipelas, proctitis, vulvovaginitis, pneumonia, endocarditis, meningitis, sepsis, necrotizing fasciitis, and myonecrosis [
123456].
GAS is the most common cause of bacterial pharyngitis in children [
7]. Antibiotic resistance to this organism has been changing in recent years, mostly due to inappropriate usage of wide spectrum antibiotics [
8]. The frequency of resistance of this organism to antibiotics and the number of drugs to which they are resistant have been increasing worldwide [
9]. Currently, penicillin is the drug of choice for GAS pharyngitis treatment, and penicillin resistance to GAS has not been reported yet [
58]. However, the prevalence of resistance to other antibacterial agents such as macrolides has been increasing [
34710]. The antibiotic resistance rate to GAS is related to geographic and epidemiologic factors and the time of investigation.
Continuous local surveillance is recommended to observe changes in the antimicrobial susceptibility profile of GAS in order to guide physicians to choose appropriate antibiotics.
There are scanty data on epidemiology and antibiotic resistance of GAS in Iranian children. The current resistance pattern of GAS in Iran is unknown; therefore, this study was conducted to evaluate the antibiotic susceptibility of GAS to the antibiotics usually used in Iran for treatment of GAS pharyngitis in children.
Materials and Methods
1. Study population
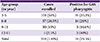
In this prospective study, children 3-15 years of age with acute tonsillopharyngitis who attended.
Mofid Children's Hospital emergency ward in Tehran, Iran were enrolled in a sequential manner from 2010-2013. The study was approved by the ethics review committee for clinical research, Pediatric Infectious Research Center (PIRC). Informed consent was received from children's guardians before enrollment.
Exclusion criteria were pharyngitis with at least one of the following signs and symptoms: conjunctivitis, coryza, prominent cough, vesicular or ulcerative stomatitis, and hoarseness or aphonia. Throat culture was carried out in 200 children.
2. Sample collection, transport, and culture
A throat sample was obtained with a Dacron swab from the patients by a physician and was transported to the Pediatric Infectious Research Center in the thioglycolate transport media within 2 hours. Each sample was cultured on trypticase soy blood agar with 5% sheep blood, incubated overnight at C under 5% CO2 effect, and tested for the pressure of GAS by the formation of distinct zones of beta hemolysis around colonies. The isolated strains were identified as GAS by colony morphology, gram staining, beta hemolysis on blood agar, sensitivity to bacitracin (inhibition screening test using 0.04-Ubacitracin disk), a positive pyrrolidonyl arylamidase (PYR) test result, and the presence of Lancefield A antigen determined by agglutination test.
3. Antibiotic susceptibility testing
Antimicrobial susceptibility was first identified by disk diffusion method on Muller-Hinton agar supplemented with 5% defibrinated sheep blood using the disk of commonly used antibiotics in Iran and in accordance with Clinical and Laboratory Standards Institute (CLSI 2012) guideline [
11].
The antibiotics used were erythromycin (15 µg), penicillin (1 µg), azithromycin (15 µg), clarithromycin (15 µg), ofloxacin (5 µg), clindamycin (2 µg), rifampin (5 µg), ceftriaxone, and cefixime.
Cefixime is one of the most commonly used antibiotics for upper respiratory tract infection treatment in Iran, but
in vitro susceptibility of Streptococcus pyogenes to this antibiotic is not included in the CSLI 2012 guideline; therefore, another reference for determining the rate of susceptibility was used [
1112].
Susceptibility of the GAS strains to the described antibiotics was also checked by the broth dilution method according to the CLSI, 2012 guideline recommendation. Briefly susceptibility testing was performed by broth microdilution procedure using dried plates reconstituted with Mueller-Hinton broth with 5% lysed horse blood. The inocula were 5 × 105 CFU/mL. The microdilution trays were incubated in ambient air at 35℃ for 24 hours. Minimum inhibitory concentration (MIC) was determined after 24 hours of incubation and was defined as the lowest concentration that yielded no visible growth. Streptococcus pneumoniae ATCC 49619 was included as a control strain.
4. Statistical analysis
Frequency of categorical variables including susceptible and resistant strains, age groups, and sign and symptoms were reported as numbers and percentages.
Discussion
Although there are several therapeutic options for GAS pharyngitis, the most acceptable recommendation is single dose intramuscular benzathine penicillin in Iran because penicillin is the drug of choice for the treatment of GAS pharyngitis, and no GAS resistance to this antibiotic has been reported yet throughout the world [
5]. In addition, the compliance of Iranian parents for ten days oral therapy is usually low.
On the other hand, there are some families that do not accept injection, or patients with immediate-type hypersensitivity to penicillin that compel pediatricians to use other therapeutic options such as macrolides, oral beta lactams, clindamycin, or oral cephalosporins [
513]. So it is very important for all the physicians to be aware of local antimicrobial susceptibility patterns to select appropriate alternative treatment options.
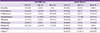
In our study, all the GAS strains were susceptible to penicillin, so this antibiotic remains the drug of choice for GAS pharyngitis.
Surprisingly, 8.4% of GAS strains were resistant to rifampin by broth dilution method, and 5% of the strains had intermediate sensitivity to this antibiotic. In other studies from Romania in 2011, the USA in 2003, and Greece in 2009, all of the GAS strains were susceptible to rifampin [
1415]. Epidemiologically, most of the provinces of Iran are endemic for tuber-culosis, so it seems that rifampin usage as one the main agents of tuberculosis treatment might be a cause of increasing resistance to rifampin, and this is an alarm for physicians in areas endemic for tuberculosis to be aware and use the anti-tuberculosis antibiotics cautiously. In addition, rifampin might be used in the treatment regimen of some infections caused by multi-resistant microorganisms, such as acinetobacter spp. and MRSA. The increasing rate of these multi drug-resistant microorganisms in recent years might be another cause of increasing consumption and resistance to rifampin.
Macrolides have been widely used for the treatment of GAS pharyngitis, and it seems that high resistance to the macrolides in recent years is related to this over usage.
In our study, 33.9%, 57.6%, and 33.9% of the GAS strains were resistant to erythromycin, azithromycin, and clarithromycin, respectively.
Other studies confirm the increasing rate of resistance to macrolides in most parts of the world [
416]. An increasing trend toward erythromycin resistance was reported from Taiwan, and then decreased once the use of this antibiotic was reduced [
17]. The resistance rate to erythromycin decreased from 53.1% in 1998 and 2000 to 14.6% in 2002 and 2004, and finally to 10.7% in 2006-2010 [
17].
Currently, treatment of GAS pharyngitis with macrolides is absolutely discouraged in Iran. The results of a surveillance study in Iran from 1995-1997 showed 0.2% resistance to erythromycin [
18]. After nearly 15 years, the resistance rate has reached 33.9% and 57.6% resistance to erythromycin and azithromycin, respectively. These findings might be the result of inappropriate use of these antibiotics in recent years in Iran.
Surprisingly the resistance to azithromycin was more than the two other macrolides. Azithromycin is one of the antibiotics in which general practitioners and pediatricians are very interested in Iran. Its low cost, availability and short course of therapy have made it a first choice for many related pediatric infections. Clarithromycin is more expensive and less popular for usage among general practitioners in Iran. Longer course of therapy (10 vs. 5 days) and more side effects have made Erythromycin loss its priority after introduction of the azithromycin. So it seems that the increased resistance of azithromycin in comparison of the two other macrolides is related to its more consumption in Iran.
In this study, 13.5% of strains were resistant to clindamycin, which is similar to the result of a study from Romania in 2011 in which 15% of the strains were resistant to clindamycin [
15]. This rate of resistance should warn physicians to use this antibiotic restrictedly and logically to prevent the rising resistance rate in the future. A study from Korea showed 32.5% resistance of GAS to clindamycin [
2]. Nevertheless there are some reports showing very low resistance to clindamycin from other countries [
1419]. This might be related to difference in the rate of resistance genotypes and phenotypes (e.g. cMLSB and iMLSB) or policies of antibiotic consumption among different parts of the world.
The resistance rate of our GAS strains to ofloxacin, the only fluoroquinolone that was evaluated in our study, was 32.5%. In general, older fluoroquinolones (e.g., ciprofloxacin) have limited activity against GAS pharyngitis and should not be used to treat GAS pharyngitis [
20]. Newer fluoroquinolones (e.g., levofloxacin and moxifloxacin) are active
in vitro against GAS, but they are expensive, have an unnecessarily broad spectrum of activity, and therefore not recommended for routine treatment of GAS pharyngitis [
20].
In 2003, a study from the USA showed 0.05% resistance of GAS to levofloxacin [
19]. On the other hand, a study from Belgium identified an increase in fluoroquinolones non-susceptibility from 4.3% (2008) to 10.9% (2009) to 21.6% in 2010 [
21].
Although fluoroquinolones are used restrictedly in the pediatric age group, it seems that inappropriate use of this category of antibiotics in domestic animals, veterinary medicine, industries, and also in adults has raised the GAS resistance to these agents in recent years in our region.
Although some studies from 2002 to 2012 with no GAS resistance to cefteriaxon exist, 11.8% of the GAS stains in the current study were resistant to this antibiotic, which might again be the result of its over-usage in our country [
14]. The relationship between antibiotic usage and resistance is strongly supported by data from this study. It seems that countries with the highest per capita antibiotic consumption have the highest resistance [
9].
The signs and symptoms of GAS pharyngitis overlap extensively with other infectious causes, particularly viral agents, making a diagnosis based solely on clinical findings difficult [
513].
Although there are several scoring systems to raise the probability of streptococcal pharyngitis in children, none of them could definitely differentiate streptococcal from non-streptococcal ones.
In this study, despite usage of the exclusion criteria, only one-third of the enrolled cases were culture positive. One of the most important reasons for this problem is the liberal use of antibiotics in Iran, which affects the rate of positive cultures. In addition, our study was based on culture result, and rapid antigen test or serologic study for detecting GAS infection was not performed; therefore, the GAS positive-culture negative cases could not be determined.
According to 2012 Infectious Diseases Society of America guideline for the diagnosis and management of group A streptococcal pharyngitis, diagnostic studies for GAS pharyngitis are not indicated for children <3 years. Therefore, we conducted our study for children 3-15 years old particularly because streptococcal pharyngitis is most prevalent in 5-15 years old cases [
20].
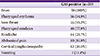
The most prevalent symptoms of streptococcal pharyngitis are the sudden onset of fever greater than 38℃ and sore throat [
513]. Cervical lymphadenopathy, pharyngeal and/or tonsillar inflammation, or exudates are common signs [
513]. Palatal petechiae and scarlatiniform rash are highly specific, but uncommon [
13]. Some nonspecific symptoms such as headache, vomiting, and abdominal pain may also be noted [
13]. In our study, the most prevalent symptoms and signs were fever, sore throat, and pharyngeal erythema and exudate, respectively. In our and most other studies, fever is the most constant symptom of streptococcal pharyngitis, so it seems that absence of fever could generally help to rule out GAS pharyngitis.
In conclusion, it seems that the high rate of GAS resistance to some antibiotics in this study should warn physicians to use the antibiotics restrictedly and logically to prevent the rising of resistance rates in the future. Continuous local surveillance is also necessary to achieve the best therapeutic option for GAS treatment.
Although the number of isolates in this study was not sufficient to make any epidemiological conclusions, the high resistance to some antibiotics could render these data useful for future decisions to develop a therapeutic streptococcal guideline in Iran.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download