Abstract
Background
Acute bacterial prostatitis is an uncommon male urinary tract infection that is the result of severe prostatic infection mainly by gram-negative bacteria. We conducted a retrospective study to report clinical outcomes of patients with acute bacterial prostatitis.
Materials and Methods
The clinical records of 49 patients diagnosed with acute bacterial prostatitis were reviewed retrospectively and patients' symptoms, investigations, and treatments were analyzed.
Results
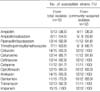
All patients presented with fever and voiding symptoms. Some patients (22.4%) had a history of prior manipulation of the lower urinary tract including transrectal prostate biopsy. Urine cultures were positive for 51% of the patients. The most common pathogen was Escherichia coli (60%), followed by Pseudomonas aeruginosa (20%) and Staphylococcus aureus (12%). The ciprofloxacin susceptibility against E. coli was 80%. All patients were treated with parenteral antibiotics in the hospital followed by oral antibiotics for average of three weeks. The major drugs used for empirical treatment were cephalosporins, aminoglycosides, and fluoroquinolones. Prostatic abscess was found in two (4.1%) patients and chronic pelvic pain syndrome developed in six (12.2%) patients during follow-up.
Figures and Tables
References
1. Wagenlehner FM, Naber KG. Therapy of prostatitis syndrome. Urologe A. 2001. 40:24–28.
2. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999. 282:236–237.

3. Schaeffer AJ, Datta NS, Fowler JE Jr, Krieger JN, Litwin MS, Nadler RB, Nickel JC, Pontari MA, Shoskes DA, Zeitlin SI, Hart C. Chronic Prostatitis Collaborative Research Network. Overview summary statement. Diagnosis and management of chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). Urology. 2002. 60:Suppl 6. 1–4.
4. Rubin RH, Shapiro ED, Andriole VT, Davis RJ, Stamm WE. Evaluation of new anti-infective drugs for the treatment of urinary tract infection. Infectious Diseases Society of America and the Food and Drug Administration. . Clin Infect Dis. 1992. 15:Suppl 1. S216–S227.
5. Neal DE Jr. Nicket JC, editor. Acute bacterial prostatitis. Textbook of prostatitis. 1999. 1st ed. Oxford: Isis Medical Media;115.
7. Etienne M, Chavanet P, Sibert L, Michel F, Levesque H, Lorcerie B, Doucet J, Pfitzenmeyer P, Caron F. Acute bacterial prostatitis: heterogeneity in diagnostic criteria and management. Retrospective multicentric analysis of 371 patients diagnosed with acute prostatitis. BMC Infect Dis. 2008. 8:12.

8. Lee SJ, Cho YH, Kim BW, Lee JG, Jung SI, Lee SD, Lee SE, Kim ME, Choi YD, Rim JS, Sim BS, Cho IR, Ryu SB, Kim CS, Kim WJ, Lee TY. A multicenter study of antimicrobial susceptibility of uropathogens causing acute uncomplicated cystitis in woman. Korean J Urol. 2003. 44:697–701.
9. Kim ME, Ha US, Cho YH. Prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in female outpatients in South Korea: a multicentre study in 2006. Int J Antimicrob Agents. 2008. 1:Suppl 1. s15–s18.

10. Kirby RS, Lowe D, Bultitude MI, Shuttleworth KE. Intra-prostatic urinary reflux: an aetiological factor in abacterial prostatitis. Br J Urol. 1982. 54:729–731.

11. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999. 20:250–278.
12. Naber KG, Bergman B, Bishop MC, Bjerklund-Johansen TE, Botto H, Lobel B, Jinenez Cruz F, Selvaggi FP. Urinary Tract Infection (UTI) Working Group of the Health Care Office (HCO) of the European Association of Urology (EAU). EAU guidelines for the management of urinary and male genital tract infections. Urinary Tract Infection (UTI) Working Group of the Health Care Office (HCO) of the European Association of Urology (EAU). Eur Urol. 2001. 40:576–588.

13. Yamamoto S, Shima H, Matsumoto T. Controversies in perioperative management and antimicrobial prophylaxis in urologic surgery. Int J Urol. 2008. 15:467–471.

14. Wagenlehner FM, Naber KG. Prostatitis: the role of antibiotic treatment. World J Urol. 2003. 21:105–108.

15. Ludwig M, Schroeder-Printzen I, Schiefer HG, Weidner W. Diagnosis and therapeutic management of 18 patients with prostatic abscess. Urology. 1999. 53:340–345.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download