Abstract
We report on a 45-year-old man with a confirmed diagnosis of acute myopericarditis associated with Mycoplasma pneumoniae. He visited our emergency department due to high fever (39℃) via a primary clinic. We made a diagnosis of myopericarditis based on symptoms, cardiac enzymes, electrocardiography, and transthoracic echocardiography. Serology (particle agglutination) testing for M. pneumoniae IgG antibody was also performed. The IgG antibody titer was 1:80 on the second day of admission, and increased to 1:2,560 by the 12th day of admission. Therefore, we confirmed the diagnosis of acute myopericarditis associated with M. pneumoniae and subsequently treated him with azithromycin. The symptoms and laboratory findings improved, and he recovered uneventfully.
Mycoplasma pneumoniae is a common pathogen in upper and lower respiratory tract infections. M. pneumoniae infection manifests as pharyngitis, bronchitis and atypical pneumonia in children and adolescents (1). M. pneumoniae infection can also present with extrapulmonary manifestations such as skin lesions, gastrointestinal or neurologic symptoms, as well as cardiac involvement (2). Cardiac involvement, such as acute myocarditis, pericarditis or myopericarditis, is an infrequent manifestation of M. pneumoniae (2-5). In 1979, a review reported by Ponka found that only 58 cases of carditis associated with M. pneumoniae infection had been reported in medical literature (4). In 2002, Paz et al. (5) reported on an additional 21 cases of carditis, and a few cases have been reported since then (6, 7). There have been only a few reports in Korea of M. pneumoniae-associated carditis in pediatric patients (8-10). However, to our knowledge, there has been no report of an adult case. Here, we report a serologically confirmed case of acute myopericarditis associated with M. pneumoniae in a Korean adult.
A 45-year-old previously healthy man was admitted to a primary clinic due to high fever (39℃). He also had a cough and whitish sputum. There was no chest pain or dyspnea reported. The initial complete blood count revealed a white cell count of 16.8×103/mm3, a hemoglobin of 13.1 g/dL, and a platelet count of 240×103/mm3. The C-reactive protein (CRP) level was elevated to 22.8 mg/dL, and the EKG showed a normal sinus rhythm. On the third day of admission, he complained of acute severe chest pain in the retrosternal area radiating to the left shoulder for two hours. During this time, the EKG showed abnormal T-wave inversions in the III and aVF leads, and a slight ST elevation in the I and aVL leads. Therefore, he was referred to the emergency department of our hospital for further evaluation.
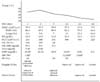
Upon presentation at our hospital, there was no chest pain and the EKG revealed an upward concave T-wave elevation below 1 mm in the I, aVL and V6 leads and an elevation of the cardiac enzymes. He was admitted to the intensive care unit of our hospital with the suspicion of acute myopericarditis. The initial subjective symptoms were cough, whitish sputum, sore throat, and dyspnea on exertion. The dyspnea was aggravated in the supine position and relieved upon bending forward. Physical examination revealed a temperature of 39℃, a pulse rate of 110 beats/min, a blood pressure of 120/70 mmHg, and no murmur. The initial laboratory tests showed a white cell count of 19.4×103/mm3, a hemoglobin of 14.6 g/dL, and a platelet count of 233×103/mm3. The CRP concentration was elevated to 22.9 mg/dL. The CK/CK-MB/Tn-I was elevated on the first day of admission and normalized by the third day of admission (Fig. 1). There was an upward concave ST elevation below 1 mm in the I, aVL, and V6 leads in the initial EKG. Initial chest x-ray showed mild cardiomegaly with slight pulmonary vascular congestion. However, there was no definite active parenchymal lung lesions noted. The initial echocardiogram revealed minimal pericardial effusion, multiple focal regional wall motion abnormalities and mild left ventricular dysfunction (ejection fraction, 48%). The coronary angiography results were normal. Pericardiocentesis was not possible due to the small amount of pericardial effusion. The blood, urine and throat cultures were all negative. On the fifth day of admission, the chest x-ray showed a newly developed left side pleural effusion. We suspected the diagnosis of an acute myopericarditis combined with pharyngitis or pneumonia due to an atypical pathogen, ceftriaxone and azithromycin were started. After a few days, the laboratory findings slightly improved but the symptoms including a sore throat, chest pain and mild fever persisted. Therefore, the antibiotic regimen was changed to meropenem and azithromycin. Serology tests for serum toxoplasma Ig M, EBV-VCA Ig M, EBV-EA IgM, HBs Ag, anti-HCV antibody, throat influenza virus Ag, throat parainfluenza virus Ag, and throat adenovirus Ag were all negative. The enterovirus RT-PCR from the stool specimen was also negative.
Serology for Mycoplasma IgG antibody was also performed using the particle agglutination (PA) method. The initial (second day of admission) IgG titer was 1:80 and this increased to 1:160 on the fifth day of admission) and to 1:2,560 on the 12th day of admission (Fig. 1). Based on clinical manifestations, cardiac enzymes data, EKG, echocardiographic findings, and increasing Mycoplasma IgG antibody titer, the patient was diagnosed with acute myopericarditis associated with M. pneumoniae on the 12th day of admission. The patient was then treated with a single antibiotic regimen using azithromycin 500 mg IV q 24 hour for 7 days, and then changed to oral azithromycin. The Mycoplasma IgG antibody titer decreased to 1:640 by the 24th day of admission. Follow-up echocardiography revealed a normal left ventricular ejection fraction and a decrease in the pericardial effusion compared to the initial study. The clinical symptoms (i.e., fever, sore throat and chest discomfort) and laboratory findings (CRP and white blood cell count) also improved. The patient was discharged with oral azithromycin on the 28th day of admission and followed 10 days later at the outpatient clinic. At follow-up, the sore throat symptoms had resolved, the CRP level and leukocyte counts, and the EKG and chest x-ray all returned to normal The patient is currently doing well without complications.
The known common causes of myopericarditis are viruses such as enterovirus, Epstein-Barr virus, Cytomegalovirus, Human Herpes virus-6, adenovirues, influenza A and B, parvovirus B19, Hepatitis B and C, Human Immunodeficiency virus, and varicella (11). Finkelstein and Klainer (12) first described M. pneumoniae pericarditis in three cases of pericarditis in 1944. Since then, while additional M. pneumonia-associated myocarditis or pericarditis cases have been reported in the medical literature (2, 4, 5), only a few cases have been reported in pediatric patients in Korea (8-10). However, to our knowledge, there has been no known report of adult cases in Korea.
The best method for identifying pathogenic agents associated with pericarditis, myocarditis or myopericarditis is to take tissue directly from the involved area or a pericardial effusion and use it in microbiologic cultures (11). However, there are significant risks associated with obtaining a sample of tissue from the pericardium. In addition, culturing M. pneumoniae is difficult, and it takes several weeks to confirm the culture results. Therefore, additional methods for diagnosing M. pneumoniae infection have been developed, including serological methods such as the compliment fixation test (CFT), the cold agglutination test, the particle agglutination (PA) test, immunofluorescence antibodies, EIA and ELISA, and polymerase chain reaction (PCR)-based methods (13, 14).
Although PCR has recently been used for early and rapid detection of M. pneumoniae infection, there are issues in clinical practice regarding false positives for the carrier state (15). Currently CFT is used widely worldwide; its sensitivity and specificity is 90% and 94%, respectively (16). Although the specificity of the PA test is inferior to that of the CFT, the sensitivity of it is similar to that of the CFT or ELISA (13, 14, 17). Therefore, PA test can be useful for the diagnosis of M. pneumoniae infection. Several countries such as Korea, Japan, and South-East Asian countries use the PA test as a serological diagnostic method for the diagnosis of M. pneumoniae infection (18). According to Kim et al. (19), a 4-fold or more increase in the antibody titer, or a single titer ≥1:640 confirms the diagnosis of a M. pneumoniae infection. At our hospital, the PA test is performed when M. pneumoniae infection is suspected. In the present case, the result of this test showed a 4-fold increase in the IgG antibody titer and a single titer ≥1:640 (1:2,560), therefore confirming the diagnosis of M. pneumoniae infection.
Although there have been no report in a Korean adult, there is a possibility of publication bias. Possible explanations for this publication bias are as follows. Clinicians might not perform serologic test to confirm M. pneumoniae infection because M. pneumoniae infection in adult is less common than that in children although there were clinical manifestations suggesting that infection. And, because M. pneumoniae infection is not rare disease, clinicians might think that there had been many cases and might not publish the M. pneumoniae infection associated with acute myopericarditis. Also, besides serologic test, there need to perform invasive tests such as pericardiocentesis, or myocardial biopsy to confirm M. pneumoniae infection and culturing M. pneumoniae is difficult in routine laboratory.
In conclusion, we report the first confirmed case of acute myopericarditis associated with M. pneumoniae in a Korean adult. M. pneumoniae should be considered in differential diagnosis for pathogens in acute myopericarditis patients in Korea.
Figures and Tables
References
1. Waites KB. New concepts of Mycoplasma pneumoniae infections in children. Pediatr Pulmonol. 2003. 36:267–278.
2. Sands MJ Jr, Satz JE, Turner WE Jr, Soloff LA. Pericarditis and perimyocarditis associated with active Mycoplasma pneumoniae infection. Ann Intern Med. 1977. 86:544–548.

3. Farraj RS, McCully RB, Oh JK, Smith TF. Mycoplasma-associated pericarditis. Mayo Clin Proc. 1997. 72:33–36.

4. Pönkä A. Carditis associated with Mycoplasma pneumoniae infection. Acta Med Scand. 1979. 206:77–86.
5. Paz A, Potasman I. Mycoplasma-associated carditis. Case reports and review. Cardiology. 2002. 97:83–88.
6. Duthoit G, Ou P, Sidi D, Bonnet D. Mycoplasma pneumoniae myopericarditis in children. Arch Mal Coeur Vaiss. 2006. 99:511–513.
7. Esposito S, Colombo C, Ravaglia R, Faelli N, Tagliabue C, Corti F, Costantini D, Principi N. Mycoplasma pneumoniae pericarditis and cardiac tamponade in a 7-year-old girl with cystic fibrosis. Infection. 2006. 34:355–356.

8. Jeon CH, Hong SY, Song MS, Kim CH, Hwang YH, Cho KH. Pericardial Effusion: Report of Three Unusual Cases. J Korean Pediatr Cardiol Soc. 2002. 6:97–103.
9. Koo GD, Ahn SH, Kim HS, Cho BS, Cha SH. A Case of Pericarditis Associated with Mycoplasma and Salmonella co-Infection. Korean J Pediatr Infect Dis. 1997. 4:155–159.

10. Lee JM, Lee SJ, Kim WD, Cho SM, Lee DS, Kim DK, Choi SM. A case of pericarditis with pericardiac effusion caused by Mycoplasma pneumonia. Dongguk J Med. 2003. 10:473–479.
11. Imazio M, Trinchero R. Myopericarditis: Etiology, management, and prognosis. Int J Cardiol. 2008. 127:17–26.

12. Finkelstein D, Klainer MJ. Pericarditis associated with primary atypical pneumonia. Am Heart J. 1944. 28:385–394.

13. Echevarría JM, León P, Balfagón P, López JA, Fernández MV. Diagnosis of Mycoplasma pneumoniae infection by microparticle agglutination and antibody-capture enzyme-immunoassay. Eur J Clin Microbiol Infect Dis. 1990. 9:217–220.

14. Yoo SJ, Oh HJ, Shin BM. Evaluation of Four Commercial IgG- and IgM-specific Enzyme Immunoassays for Detecting Mycoplasma pneumoniae Antibody: Comparison with Particle Agglutination Assay? J Korea Med Sci. 2007. 22:795–801.

15. Liu FC, Chen PY, Huang F, Tsai CR, Lee CY, Wang LC. Rapid diagnosis of Mycoplasma pneumoniae infection in children by polymerase chain reaction. J Microbiol Immunol Infect. 2007. 40:507–512.
16. Jacobs E. Serological diagnosis of Mycoplasma pneumoniae infections: a critical review of current procedures. Clin Infect Dis. 1993. 17:Suppl 1. 79–82.
17. Barker CE, Sillis M, Wreghitt TG. Evaluation of Serodia Myco II particle agglutination test for detecting Mycoplasma pneumoniae antibody: comparison with µ-capture ELISA and indirect immunofluorescence. J Clin Pathol. 1990. 43:163–165.

18. Chan PW, Lum LC, Ngeow YF, Yasim MY. Mycoplasma pneumoniae infection in Malaysian children admitted with community acquired pneumonia. Southeast Asain J Trop Med Public Health. 2001. 32:397–401.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download