Abstract
Azithromycin shows a comparable therapeutic efficacy to doxycycline against mild to moderate scrub typhus. It is safe enough to use in pregnant women or children less than 8 years of age, but may be associated with fatal cardiac dysrhythmia. Herein we report a case of scrub typhus in which torsades de pointes developed during treatment with intravenous azithromycin. A 63-year-old man with a history of hypertension and prolonged QT interval was admitted because of fever with duration of 13 days, rash, an eschar, and delirium. An initial electrocardiography showed atrial fibrillation with rapid ventricular response. Scrub typhus complicated by meningoencephalitis, pneumonitis, and possible myocarditis was diagnosed. Two 500 mg doses of azithromycin were infused over 30 minutes, 12 hours apart. The patient developed a cardiac arrest due to torsades de pointes 30 minutes after the second dose of azithromycin. After the patient was resuscitated successfully and the antibiotic was change to doxycycline. The patient eventually improved and was discharged without any sequelae.
Scrub typhus is endemic in Southeast Asia, including Korea. Doxycycline has been the drug of choice for the treatment of scrub typhus, however its becoming less effective due to the emergence of strains, resistant to doxycycline. Treatment of scrub typhus in children and pregnant women is a situation in which doxycycline is contraindicated. Azithromycin may be an ideal antibiotic for the treatment of scrub typhus because it is safe even in pregnant women and has good activities against doxycycline-resistant Orientia tsutsugamushi. In clinical studies, the efficacies of azithromycin for the treatment of scrub typhus of mild to moderate severity are comparable to those of doxycycline(1-3). These studies reaffirm that azithromycin is not associated with serious adverse effects. Reports of scrub typhus occurring during pregnancy also show the efficacy and safety of azithromycin. Further studies on the efficacy of azithromycin in treating severe scrub typhus are anticipated. Meanwhile while we want to mention a serious adverse effect that may be associated with the treatment of scrub typhus with azithromycin.
A 63-year-old man was admitted to our hospital because he had a fever lasting 13 days, myalgia, rash, and delirium. The patient had a history of uncontrolled hypertension, obesity, and fatty liver. The electrocardiography checked four years ago showed the left ventricular hypertrophy, T-wave abnormalities suggesting lateral ischemia, and prolongation of the corrected QT (QTc) interval (453 ms).
On admission, the body temperature was 37.5° and blood pressure was 185/89 mmHg. An eschar at the left inguinal area and regional lymphadenopathies were noted. Chest PA showed pulmonary congestion or interstitial pneumonitis. An initial ECG showed atrial fibrillation with rapid ventricular response and QTc interval of 442 ms. Serum potassium and ionized calcium levels were 4.8 mmol/L and 1.11 mmol/L, respectively. Arterial blood gas analysis revealed that the pH was 7.40; PCO2, 3.9 kPa; PO2, 7 kPa; and HCO3, 18 mmol/L. The cerebrospinal fluid showed a white blood cell count of 0.064 × 109/L with 44% lymphocytes, and protein and glucose levels of 1.83 g/L and 2.6 mmol/L, respectively. Brain CT revealed senile changes.
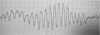
Scrub typhus complicated by encephalitis, pneumonitis and possible myocarditis was suspected, and two 500 mg doses of azithromycin were infused over 30 minutes, 12 hours apart over a period of 30 min. The patient developed a cardiac arrest 30 minute after the second infusion of azithromycin, and torsades de pointes was recorded in the electrocardiography (Fig. 1). The patient was successfully resuscitated with cardioversion. Because azithromycin was suspected of causing torsades de pointes, the antibiotic was changed to oral doxycycline. Other medications that were administered concomitantly were midazolam, furosemide, cimetidine, dopamine, and methylprednisolone. The subsequent clinical course was uneventful, and scrub typhus was confirmed by the fourfold increase in the antibody titers of O. tsutsugamushi. ECG findings at discharge were the same to those checked 4 years ago -QTc of 452 ms, left ventricular hypertrophy, and abnormal T waves.
Torsades de points (TdP) is a polymorphic ventricular tachycardia that is related with the prolongation of the corrected QT interval. It is rare, but fatal if it is not promptly identified and managed. Congenital long QT syndromes and class IA & III antiarrhythmic drugs are well-known causes of TdP. Recently, TdP by non-cardiovascular drugs, including antihistamines, cisapride, and antibiotics (the macrolides/ketolides, certain fluoroquinolones and antimalarials, pentamidine, and the azole antifungals) are increasingly recognized; although these drugs usually cause clinically unnoticeable delays of mild degree in ventricular repolarization, they may amplify the risk for torsades de pointes (TdP) when prescribed in the presence of other risk factors. Among antibiotics, macrolides have greatest potential to induce QT prolongation. The exact incidence of TdP associated with the use of macrolides is not known, but a postmarketing analysis estimated the adjusted report-utilization ratio of TdP in erythromycin is 0.07, clarithromycin 0.18, and azithromycin 0.06 reports per 1 million recommendations. The rate of TdP in cefuroxime, as a control, is 0.02 (4). Risk factors for the development of TdP by macrolides include increasing age, female sex, and structural heart diseases/co-administered drugs known to prolong the QT interval(4). Though the risk of the development of TdP by azithromycin seems to be 3 times higher than that of cefuroxime, the incidence of TdP is too low to estimate the actual risk of TdP by azithromycin, and this data are unable to establish causation of the administration of macrolides and the development of TdP. Actually reviewing the published reports, azithromycin has questionable or at least minimal risk of proarrhythmic potential, and does not alter the metabolism of other proarrhythmic drugs: in an experimental study, azithromycin prolongs QT interval, but shows no proarrhythmic effects(5); evaluation of the repolarization and proarrhythmia effects of azithromycin using the TdP-susceptible animal model does not reveal prolongation of QT interval(6); in a human volunteer study, azithromycin does not prolong QT interval(7); and there are only three case reports of TdP(8-10) and one case of QT prolongation(11), after use of azithromycin, exclusively in patients with underlying cardiac diseases.
Thus, azithromycin per se has a questionable association with TdP, but there is a possibility that it contributes the development of TdP by other proarrhythmic drugs or underlying cardiac diseases(12, 13). In our patient, other known proarrhythmic drugs are not administered, so underlying QT prolongation is the major cause of the TdP. However, development of TdP in patients with underlying QT prolongation after receiving azithromycin has been reported in only three cases, so its occurrence is a very rare event. Thus, we guess scrub typhus is an additional contributing factor for development of TdP in our patient.
Scrub typhus is a relatively benign disease in the antibiotic era. However, if the appropriate treatment is delayed or missed, the mortality rates reach up to 30% (14). Severe scrub typhus is characterized by involvement of multiple organs, including liver, lung, brain, kidney, and heart. The frequencies of involvement of these organs vary according to the duration of scrub typhus; generally the longer the duration of the illness, higher the frequent the incidence of complications. In studies performed in Korean, pneumonic involvement occurs in 34-69%, hepatic involvement in 90%, and azotemia in 15%. Pneumonitis can cause hypoxia that alters serum electrolytes level, especially potassium, and consequently contributes to the development of cardiac dysrhythmia. Hepatic dysfunction and azotemia can be associated with the development of cardiac dysrhythmia by altering the metabolism of proarrhythmic drugs. Furthermore, other risk factors, such as electrolytes imbalance, that can prolong the QT interval are frequently observed in scrub typhus. In addition, in Korea, scrub typhus occurs more frequently in elderly women, which is a risk factor for development of TdP during use of macrolides. Elderly people have many underlying illnesses and take several types of medications, such as anti-hypertensive medications and diuretics, which can contribute to the development of TdP. In addition, chronic B viral hepatitis or alcoholism is prevalent in the elderly in Korea, and may result results in altered drug metabolism. Alcoholism is common in men residing in urban areas, which is associated alcoholic liver diseases and alcoholic cardiomyopathy.
About the heart involvement in scrub typhus, pathologic examination of the heart performed in era before the introduction of tetracycline or chloramphenicol reveals the following abnormalities(15): perivascular and intramyocardial infiltration of leukocytes in about 50% of the autopsied patients; mild inflammatory reactions in the Purkinje tissue of the papillary muscles in certain portion of the patients; and subepicardial petechial hemorrhages in about half of the patients. Myocardial involvement by scrub typhus is usually not evident clinically, but in certain patients death may occur due to congestive heart failure or serious dysrhythmia; congestive heart failure occurs only in severe cases and begins in second or third week(16). Clinical features of myocardial involvement are cardiac enlargement, persistent gallop rhythm, apical systolic murmur; heart failure and resultant pulmonary edema at the terminal phase; and serious dysrhythmia usually occurred concomitantly with myocardial failure. The ECG findings representing myocardial injury are low voltage, slurring and notching of QRS complexes, and atrial fibrillation(17). Sharp T wave inversion or notching in lead CR-3 may also be another finding suggesting myocardial involvement(16). Thus, atrial fibrillation in our patient is certainly thought to be an evidence of myocardial involvement of scrub typhus. In post-antibiotic era, with the decrease of the number of patients with severe scrub typhus, are rare. However there have been reports of; myocarditis(17), pericarditis or pericardial effusion(18), and acute myocardial infarction (19). One study shows 3% of incidence of myocarditis (20). Various electrocardiographic abnormalities are reported, but, they are usually not specific to scrub typhus (21, 22). In a Korean study, the incidences of QT prolongation and the first degree AV block in scrub typhus are 5.1% and 5.1% each. A study from China showed ECG abnormalities of benign significance; one case showed QTc interval prolongation only during acute phase(21). A study from Thailand reports nonspecific electrocardiographic abnormalities that are those expected in other febrile illnesses(22); but the duration of the illness of the enrolled patients are 4 days (mean), which means that they include the early phase of scrub typhus and may not be adequate for studying cardiac complications of scrub typhus.
Thus, because the risk of fatal cardiac dysrhythmia may be substantial in severe scrub typhus, the use of azithromycin for the treatment of scrub typhus is better to be reserved to cases in which the disease severity is mild to moderate until further studies confirm the safety of azithromycin in severe scrub typhus. If its use is inevitable, electrocardiography, serum level of electrolytes, and liver and renal function tests should be checked before the administration of intravenous azithromycin. Administration via oral route might be preferred. In addition, concomitant administration of medications that potentially prolong QT intervals should be avoided.
References
1. Chung MH, Han SW, Choi MG, Chang WH, Pai HJ, Shin HS, Jung HJ, Kang MH, Jung JY. Comparison of a 3-day Course of Azithromycin with Doxycycline for the Treatment of Scrub Typhus. Korean J Infect Dis. 2000. 32:433–438.
2. Kim YS, Yun HJ, Shim SK, Koo SH, Kim SY, Kim S. A comparative trial of a single dose of azithromycin versus doxycycline for the treatment of mild scrub typhus. Clin Infect Dis. 2004. 39:1329–1335.

3. Phimda K, Hoontrakul S, Suttinont C, Chareonwat S, Losuwanaluk K, Chueasuwanchai S, Chierakul W, Suwancharoen D, Silpasakorn S, Saisongkorh W, Peacock SJ, Day NP, Suputtamongkol Y. Doxycycline versus azithromycin for treatment of leptospirosis and scrub typhus. Antimicrob Agents Chemother. 2007. 51:3259–3263.

4. Shaffer D, Singer S, Korvick J, Honig P. Concomitant risk factors in reports of torsades de pointes associated with macrolide use: review of the United States Food and Drug Administration Adverse Event Reporting System. Clin Infect Dis. 2002. 35:197–200.

5. Milberg P, Eckardt L, Bruns HJ, Biertz J, Ramtin S, Reinsch N, Fleischer D, Kirchhof P, Fabritz L, Breithardt G, Haverkamp W. Divergent proarrhythmic potential of macrolide antibiotics despite similar QT prolongation: fast phase 3 repolarization prevents early afterdepolarizations and torsade de pointes. J Pharmacol Exp Ther. 2002. 303:218–225.

6. Thomsen MB, Beekman JD, Attevelt NJ, Takahara A, Sugiyama A, Chiba K, Vos MA. No proarrhythmic properties of the antibiotics Moxifloxacin or Azithromycin in anaesthetized dogs with chronic-AV block. Br J Pharmacol.
. 2006. 149:1039–1048.

7. Strle F, Maraspin V. Is azithromycin treatment associated with prolongation of the Q-Tc interval. Wien Klin Wochenschr. 2002. 114:396–399.
8. Russo V, Puzio G, Siniscalchi N. Azithromycin- induced QT prolongation in elderly patient. Acta Biomed. 2006. 77:30–32.
9. Arellano-Rodrigo E, Garcia A, Mont L, Roque M. Torsade de pointes and cardiorespiratory arrest induced by azithromycin in a patient with congenital long QT syndrome. Med Clin (Barc). 2001. 117:118–119.

10. Kim MH, Berkowitz C, Trohman RG. Polymorphic ventricular tachycardia with a normal QT interval following azithromycin. Pacing Clin Electrophysiol. 2005. 28:1221–1222.

11. Matsunaga N, Oki Y, Prigollini A. A case of QT-interval prolongation precipitated by azithromycin. N Z Med J. 2003. 116:U666.
12. Granowitz EV, Tabor KJ, Kirchhoffer JB. Potentially fatal interaction between azithromycin and disopyramide. Pacing Clin Electrophysiol. 2000. 23:1433–1435.

13. Samarendra P, Kumari S, Evans SJ, Sacchi TJ, Navarro V. QT prolongation associated with azithromycin/amiodarone combination. Pacing Clin Electrophysiol. 2001. 24:1572–1574.

14. Levine HD. Pathologic study of thirty-one cases of scrub typhus fever with especial reference to thercadiovascular system. Am Heart J. 1946. 31:314–328.

15. Sayen JJ, Pond HS, Forrester JS, Wood FC. Scrub typhus in Assam and Burma. Medicine. 1946. 25:155–214.

16. Woodward TE, McCrumb FR, Carey TN, Togo Y. Viral and rickettsial causes of cardiac disease, including the Coxsachie virus etiology of pericarditis and myocarditis. Ann Intern Med. 1960. 53:1130–1150.

17. Yotsukura M, Aoki N, Fukuzumi N, Ishikawa K. Review of a case of tsutsugamushi disease showing myocarditis and confirmation of Rickettsia by endomyocardial biopsy. Jpn Circ J. 1991. 55:149–153.

18. Chang JH, Ju MS, Chang JE, Park YS, Han WS, Kim IS, Chang WH. Pericarditis due to Tsutsugamushi disease. Scand J Infect Dis. 2000. 32:101–102.

19. Kim DG, Kim JW, Choi YS, Kim SH, Kim SM, Park CG, Seo HS, Oh DJ. Acute myocardial infarction following scrub typhus infection. Int J Cardiol. 2007. 114:e18–e20.

20. Tsay RW, Chang FY. Serious complications in scrub typhus. J Microbiol Immunol Infect. 1998. 31:240–244.
21. Fang CY, Dennis DT, Lee JB. Electrocardiographic changes in scrub typhus patients. Southeast Asian J Trop Med Public Health. 1977. 8:503–509.
22. Watt G, Kantipong P, Jirajarus K. Acute scrub typhus in Northern Thailand: EKG changes. Southeast Asian J Trop Med Public Health. 2002. 33:312–313.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download