Abstract
The aerozolization is one of possible Brucella transmission mechanisms, particularly in air-borne exposed laboratory workers. In this study, seven laboratory workers were potentially exposed to B. abortus via aerosols. Two laboratory workers who sniffed an agar plate several times were considered to be at high risk for acquiring the disease, 5 workers who did not work directly with the strain were be considered at low risk of infection. Prophylactic antibiotics of doxycycline 200 mg/day and rifampin 600 mg/day were offered for 6 weeks in high risk workers and 3 weeks for low risk workers, respectively. Enrolled workers were advised to check for serological testing of Brucella species every 3 weeks during a total period of 12 weeks. Compliance with taking medicine was 57.1% (4/7) and compliance for completing the serological tests was 85.7% (6/7). None of the laboratory workers developed clinical disease or tested positive serologically during 3 months of serological testing and 1 year of clinical follow-up.
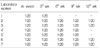
Figures and Tables
References
2. Pappas G, Papadimitriou P, Akritidis N, Christou L, Tsianos EV. The new global map of human brucellosis. Lancet Infect Dis. 2006. 6:91–99.

3. Staszkiewicz J, Lewis CM, Colville J, Zervos M, Band J. Outbreak of Brucella melitensis among microbiology laboratory workers in a community hospital. J Clin Microbiol. 1991. 29:287–290.

4. Robichaud S, Libman M, Behr M, Rubin E. Prevention of laboratory-acquired brucellosis. Clin Infect Dis. 2004. 38:e119–e122.
5. Fiori PL, Mastrandrea S, Rappelli P, Cappuccinelli P. Brucella abortus infection acquired in microbiology laboratories. J Clin Microbiol. 2000. 38:2005–2006.

6. Park MY, Lee CS, Choi YS, Park SJ, Lee JS, Lee HB. A sporadic outbreak of human brucellosis in Korea. J Korean Med Sci. 2005. 20:941–946.

7. Lim HS. Diagnosis of human brucellosis. Korean J Med. 2006. 71:1–3.
8. Park MS, Woo YS, Lee MJ, Shim SK, Lee HK, Choi YS, Lee WH, Kim KH, Park MY. The First Case of Human Brucellosis in Korea. Infect Chemother. 2003. 35:461–466.
9. Corbel Michael J., Beeching Nicholas J.. Kasper DL, Braunwal E, Fauci AS, Hauser SL, Longo DL, Jameson JL, editors. Brucellosis. Harrison's principle of internal medicine. 2005. 16th ed. New York: McGraw-Hill Korea, Inc.;914–917.
10. Memish ZA, Mah MW. Brucellosis in laboratory workers at a Saudi Arabian hospital. Am J Infect Control. 2001. 29:48–52.

11. Martin-Mazuelos E, Nogales MC, Florez C, Gomez-Mateos JM, Lozano F, Sanchez A. Outbreak of Brucella melitensis among microbiology laboratory workers. J Clin Microbiol. 1994. 32:2035–2036.

13. Grammont-Cupillard M, Berthet-Badetti L, Dellamonica P. Brucellosis from sniffing bacteriological cultures. Lancet. 1996. 348:1733–1734.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download