Abstract
The aim of this study was to evaluate the usefulness and accuracy of supraclavicular lymph node excision biopsy in the diagnosis of suspected supraclavicular lymph node metastasis of lung cancer. A retrospective review was performed to evaluate patients with suspected supraclavicular lymph node metastasis of lung cancer who underwent supraclavicular lymph node excision biopsy from January 2011 to July 2014. Forty-six patients with suspected supraclavicular lymph node metastasis of lung cancer underwent supraclavicular lymph node excision biopsy, which diagnosed benign diseases in 6 patients and malignant diseases in 40 patients. Supraclavicular lymph node excision biopsy was usually performed on patients during their first clinical visit under local anesthesia. For diagnosing suspected lung cancer, supraclavicular lymph node excision biopsy had a diagnostic sensitivity of 100%, specificity of 97.6%, positive-predictive value of 83.3%, negative-predictive value of 100%, and accuracy of 97.8%. No major complication resulted from surgical intervention. Supraclavicular lymph node excision biopsy is a useful and accurate adjunct for the evaluation of suspected supraclavicular lymph node metastasis of lung cancer in a tertiary hospital.
Lung cancer is the most common cause of cancer-related death in both men and women worldwide.1 The need for diagnosis and staging of cancer in patients with suspected lung cancer is a frequent occurrence in medical practice.2 Accurate assessment of clinical stage and cell typing at diagnosis is essential for the selection of appropriate curative and palliative therapy.34 A variety of noninvasive and invasive non-radiologic and radiologic procedures can be used for the diagnosis of lung cancer and its metastasis.2 However, in patients with lung cancer, metastases are usually located in lymph nodes within the mediastinum that are difficult to reach with minimally invasive techniques.5
In patients with lung cancer, palpable supraclavicular lymph nodes are usually involved in metastatic disease.6 In addition, non-palpable supraclavicular lymph nodes with malignancy were reported in 41% to 51% of patients with lung cancer.2 Therefore, surgical biopsy for supraclavicular lymph nodes may be a valuable tool to determine the treatment plan and cell typing.
We hypothesized that supraclavicular lymph node excision biopsy may be a useful and accurate adjunct for the evaluation of patients with suspected supraclavicular lymph node metastasis of lung cancer before determining a treatment plan. Herein, we review our experience with supraclavicular lymph node excision biopsy in patients with suspected supraclavicular lymph node metastasis of lung cancer. The aim of this study was to evaluate the usefulness and accuracy of supraclavicular lymph node excision biopsy in the diagnosis of suspected supraclavicular lymph node metastasis of lung cancer in comparison to histopathological findings.
After obtaining approval from the Institutional Review Board of Chonnam National University Hwasun Hospital, a retrospective review was performed to evaluate patients with suspected supraclavicular lymph node metastasis of lung cancer who underwent supraclavicular lymph node excision biopsy at the hospital's Department of Otolaryngology-Head and Neck Surgery from January 2011 to July 2014. All patients were suspected of having lung cancer with supraclavicular lymph node metastasis based on clinical and/or radiologic finding by pulmonologists, and referred to our department for supraclavicular lymph node excision biopsy. The criteria for significant enlarged lymph nodes in the study was a short axis diameter of more than 1 cm.3
Forty-six patients with suspected supraclavicular lymph node metastasis of lung cancer who underwent supraclavicular lymph node excision biopsy were enrolled in this study. A detailed history was obtained and thorough general physical examination and systemic examination were carried out in all cases. Charts were reviewed to obtain information about preoperative diagnostic workups and pathologic diagnoses.
All patients underwent supraclavicular lymph node excision biopsy with local anesthesia. The procedure typically was completed within 60 minutes. All cases of supraclavicular lymph nodes were confirmed histopathologically. Bronchoscopy and fine needle aspiration cytology (FNAC) were performed in 17 and 10 cases of 46 patients, respectively. FNAC was always initially performed in the largest supraclavicular lymph node. However, FNAC was not performed in patients whose supraclavicular lymph nodes were barely detected by palpation. Fisher's exact test was used in the statistical analysis using SPSS version 14.0. Statistical significance was defined as a p-value<0.05.
Forty-six patients with suspected supraclavicular lymph node metastasis of lung cancer underwent supraclavicular lymph node excision biopsy, including 30 (65.2%) men and 16 (34.8%) women. Clinical findings in these patients are summarized in Table 1. The age of the patients ranged from 40 to 86 years, with a mean of 63.3±11.9 years. Preoperative evaluations included clinical history, physical examination, and radiologic procedures. Supraclavicular, significantly enlarged lymph nodes were observed in all patients by radiologic examination. Of the 46 patients, 41 were palpable, the remaining five were non-palpable, however the metastasis was suspected in the computed tomography (CT). Of the 46 patients, 26 (56.5%) had enlarged lymph nodes located in the right neck, fifteen (32.6%) in the left neck, and five (10.9%) in the bilateral neck.
Supraclavicular lymph node excision biopsy was usually performed on patients during their first clinical visit with local anesthesia. The duration between first clinical visit and excision biopsy ranged between 0 and 17 days with a mean of 0.9±2.9 days. Except three patients who were delayed due to personal conditions or further evaluation of other diseases, all patients underwent supraclavicular lymph node excision biopsy within 3 days. None of the patients developed complications of the supraclavicular lymph node excision biopsy, such as hematoma, chyle leakage, wound infection, or nerve injury.
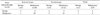
Forty of the 46 patients were diagnosed with lung cancer by supraclavicular lymph node excision biopsy. Thirty patients had adenocarcinoma. Seven had small cell carcinoma. Three had squamous cell carcinoma. Four were diagnosed with sarcoidosis. One was diagnosed with tuberculosis. One was negative for malignancy. When diagnosing suspected lung cancer, supraclavicular lymph node excision biopsy had a diagnostic sensitivity of 100%, a diagnostic specificity of 97.6%, a positive-predictive value of 83.3%, a negative-predictive value of 100%, and an accuracy of 97.8% (Table 2).
Seventeen of the 46 patients underwent bronchoscopic examination. The duration between first clinical visit and bronchoscopy ranged between 0 and 14 days with a mean of 6±0.58 days. Twelve patients were diagnosed with lung cancer, two with sarcoidosis, and one with tuberculosis. Two patients were diagnosed as negative for malignancy by the bronchoscopic examination, which eventually proved to be an adenocarcinoma and small cell carcinoma by the supraclavicular lymph node excision biopsy, respectively. When diagnosing suspected lung cancer, bronchoscopy had a diagnostic sensitivity of 100%, a diagnostic specificity of 85.7%, a positive-predictive value of 60%, a negative- predictive value of 100%, and an accuracy of 88.2% (Table 2).
Ten of the 46 patients underwent FNAC. Nine patients were diagnosed with lung cancer, however, the cell typings were not identified. One patient was diagnosed with reactive lymphadenitis, which turned out to be adenocarcinoma. When diagnosing suspected lung cancer, FNAC had a diagnostic sensitivity of 0%, a diagnostic specificity of 90%, a positive-predictive value of 0%, a negative-predictive value of 100%, and an accuracy of 90% (Table 2).
The ideal staging investigation should be inexpensive and easy to administer, highly sensitive and highly specific. In addition, it should provide accurate results that reflect the patient's true clinical state. Furthermore, it should only cause minimal patient discomfort and morbidity.78 The latest imaging techniques, such as positron emission tomography (PET), can provide infallible staging. However, cytological or histological confirmation of suspected metastasis is frequently required.89 The assessment of supraclavicular lymph nodes can be valuable in establishing both a diagnosis and a critical stage threshold for defining therapeutic options.2 Most palpable supraclavicular lymph nodes in patients with lung cancer yield a diagnosis of malignancy.6 Supraclavicular lymph node metastasis from lung cancer was reported in up to 75% of patients at the time of presentation.10 Therefore, we hypothesized that supraclavicular lymph node excision biopsy may be a useful and accurate adjunct for the evaluation of patients with suspected supraclavicular lymph node metastasis of lung cancer.
In this study, the sensitivity, specificity, positive-predictive value, negative-predictive value, and accuracy of supraclavicular lymph node excision biopsy for diagnosing suspected supraclavicular lymph node metastasis of lung cancer was 100%, 97.6%, 83.3%, 100%, and 97.8%, respectively. Supraclavicular lymph node excision biopsy had a higher specificity, positive-predictive value, and accuracy than bronchoscopy and FNAC. These values suggest that supraclavicular lymph node excision biopsy is an accurate method for assessing patients with suspected supraclavicular lymph node metastasis of lung cancer. The low positive-predictive value might be due to the somewhat small sample size. In our study, one false negative result occurred in the diagnosis of lung cancer. In the false negative case, the patient was diagnosed as negative for malignancy, which eventually proved to be a Sarcomatoid carcinoma. This result may be due to sampling errors or the lack of adequate material. However, the pulmonologist performed bronchoscopic biopsy, because the patient had symptoms, physical examination results, and radiologic results consistent with lung cancer. Therefore, joint decision-making between surgeons and pulmonologist is crucial.
Supraclavicular lymph node excision biopsy provides clear and reliable diagnosis as well as staging and cell typing as to which further investigations, such as molecular targeted therapy, should be planned. In addition, supraclavicular lymph node excision biopsy may help avoid unnecessary surgery or more invasive procedures or potential complications.8 However, it is important to recognize that the final histopathologic results may differ from the results of supraclavicular lymph node excision biopsy in rare cases, such as the one encountered in this study. If there is any suspicion of lung cancer, a further evaluation should be performed.
The suggestion for non-palpable supraclavicular lymph node surgical biopsy in patients with lung cancer varied.2611 In five patients who had non-palpable supraclavicular lymph node, we performed surgical biopsies and successfully made a diagnosis. Notably, one patient received a diagnosis as adenocarcinoma by supraclavicular lymph node excision biopsy, while the patient had been previously diagnosed as negative for malignancy by bronchoscopy. Therefore, if supraclavicular lymph nodes are detected on radiologic examinations, we suggest that supraclavicular lymph node excision biopsy should be performed, even if nonpalpable.
In summary, we suggest that supraclavicular lymph node excision biopsy has the potential to save time and cost by reducing the time from referral to diagnosis and reducing the need for invasive mediastinal staging and bronchoscopy.3 However, supraclavicular lymph node excision biopsy is not 100% accurate. Therefore, supraclavicular lymph node excision biopsy should be used in combination with clinical examination and radiologic examination. Joint decision-making between surgeons and pulmonologists is needed for accurate diagnosis. The limiting factors of this study include the fact that we were at a tertiary care center. In addition, all patients in this study were referred by pulmonologists. Therefore, there could have been an unintentional selection biases toward patients with advanced disease or an unusual case mix. In addition, this study was performed with a small sample size and retrospective review. In the future, prospective studies or multicenter studies are needed.
In patients with suspected lung cancer, a careful diagnostic approach must be used to prove the presence of a cancer, to determine the cell type, and to establish the stage while minimizing costs, discomfort, and risk to the patient.5 Based on those requirements, supraclavicular lymph node excision biopsy is a useful and accurate adjunct for the evaluation of suspected supraclavicular lymph node metastasis of lung cancer in a tertiary hospital.
Figures and Tables
References
1. Greenlee RT, Murray T, Bolden S, Wingo PA. Cancer statistics, 2000. CA Cancer J Clin. 2000; 50:7–33.

2. Fultz PJ, Feins RH, Strang JG, Wandtke JC, Johnstone DW, Watson TJ, et al. Detection and diagnosis of nonpalpable supraclavicular lymph nodes in lung cancer at CT and US. Radiology. 2002; 222:245–251.

3. Kumaran M, Benamore RE, Vaidhyanath R, Muller S, Richards CJ, Peake MD, et al. Ultrasound guided cytological aspiration of supraclavicular lymph nodes in patients with suspected lung cancer. Thorax. 2005; 60:229–233.

4. Sung YM, Lee KS, Kim BT, Kim S, Kwon OJ, Choi JY, et al. Nonpalpable supraclavicular lymph nodes in lung cancer patients: preoperative characterization with 18F-FDG PET/CT. AJR Am J Roentgenol. 2008; 190:246–252.

5. van Overhagen H, Brakel K, Heijenbrok MW, van Kasteren JH, van de Moosdijk CN, Roldaan AC, et al. Metastases in supraclavicular lymph nodes in lung cancer: assessment with palpation, US, and CT. Radiology. 2004; 232:75–80.

6. Brantigan JW, Brantigan CO, Brantigan OC. Biopsy of nonpalpable scalene lymph nodes in carcinoma of the lung. Am Rev Respir Dis. 1973; 107:962–974.
7. Grondin SC, Liptay MJ. Current concepts in the staging of non-small cell lung cancer. Surg Oncol. 2002; 11:181–190.

9. LeBlanc JK, Espada R, Ergun G. Non-small cell lung cancer staging techniques and endoscopic ultrasound: tissue is still the issue. Chest. 2003; 123:1718–1725.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download