An inflammatory pseudotumor of the lung can manifest as lung nodules or masses, which can mimic the presentation of malignant tumors. As it is not clear whether the lesions are the result of an inflammatory process or a malignancy combined with an inflammatory response, surgical resection is the recommended treatment.1 However, some patients are not amenable to surgical treatment because of medical conditions, including reduced pulmonary function or multiple lesions. I describe a case of an inflammatory pseudotumor of the lung that showed complete regression following medical treatment.
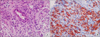
A 61-year-old male presented with a 9.3 cm×7.3 cm cavitary lung mass in the right lower hemithorax involving the right middle and lower lobes (Fig. 1A). The patient was transferred to our hospital because of a persistent fever, despite treatment with antibiotics at a previous hospital. A percutaneous needle biopsy of the cavitary lung mass was performed. The biopsy revealed an inflammatory pseudotumor of the lung, consisting of a foamy histiocytic infiltrate, with a collagenous background (Fig. 2A). Immunohistochemical staining for CD68 was positive (Fig. 2B). Due to the patient's poor pulmonary function, with forced vital capacity (FVC) of 1.34 L (35% predicted) and forced expiratory volume in 1 second (FEV1) of 1.15L (40% predicted), we adopted a conservative approach to the lung lesion rather than a complete surgical resection. Thus, the patient was treated with imipenem intravenously for 3 weeks, followed by clindamycin orally for 3 months on an outpatient basis after defervescence. All microbiological tests, including bacterial and mycobacterial cultures from sputum, blood, and pleural fluid, were negative. Glucocorticoids were not considered a treatment option due to the patient's positive response to the antibiotics. A chest computed tomography (CT) scan, performed 4 months after the medical treatment targeting the abscess-forming pathogens, showed complete regression of the lung mass (Fig. 1B). In addition, C-reactive protein had decreased significantly from 18.01 mg/dL to 0.67 mg/dL.
Surgical resection is the treatment of choice for inflammatory pseudotumors of the lung, which are also known as inflammatory myofibroblastic tumors, plasma cell granulomas, and fibrous histiocytomas. For patients who are not good candidates for surgery, nonsurgical methods can be utilized. These include glucocorticoids, radiotherapy, and chemotherapy.123 Crizotinib is an option in patients with anaplastic lymphoma kinase (ALK)-rearranged inflammatory pseudotumors.4 A previous report described a case of an inflammatory pseudotumor that responded to antibiotics.5 However, in the reported case, an uncommon microorganism affected the lungs and multiple organs.5 In the current case, the patient required a prolonged course of antibiotics, which is common in cases where a patient has a protracted infection. The negative microbiological results in the present case may have been due to antibiotic treatment administered to the patient at the previous hospital. The present case can aid the decision making of clinicians treating an inflammatory pseudotumor with an infectious cause, especially in patients with poor pulmonary function.
Figures and Tables
References
1. Urschel JD, Horan TA, Unruh HW. Plasma cell granuloma of the lung. J Thorac Cardiovasc Surg. 1992; 104:870–875.

2. Kovach SJ, Fischer AC, Katzman PJ, Salloum RM, Ettinghausen SE, Madeb R, et al. Inflammatory myofibroblastic tumors. J Surg Oncol. 2006; 94:385–391.

3. Bando T, Fujimura M, Noda Y, Hirose J, Ohta G, Matsuda T. Pulmonary plasma cell granuloma improves with corticosteroid therapy. Chest. 1994; 105:1574–1575.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download