Ginseng is a slow-growing, perennial plant with fleshy roots, belonging to the genus Panax of the family Araliaceae.1 Ginseng is one of the most widely prescribed and intensively studied herbal medicines. Several studies have indicated benefits of ginseng in the treatment of renal damage23 and hepatotoxicity.4 However, acute kidney injury as an adverse effect has not been reported.
A 43-year-old woman who had consumed 3 roots of ginseng with alcohol some days before, was transferred to our hospital because of general weakness, myalgia, and oligouria. She had been taking hypertension medication for 1 year, and had undergone surgery for early gastric cancer 3 years ago. She was in an oliguric state (150 mL/day) when she was admitted to the other hospital, and therefore, massive hydration (3 L/day) was administered. However, it did not increase her urine output, and she was referred to our hospital. A blood test showed elevation of aspartate aminotransferase (AST, 5,241 IU/L [normal range, 10–37]), alanine transaminase (ALT, 721 IU/L [normal range, 10–37]), and lactate dehydrogenase, 1,560 IU/L (normal range, 218–472) levels. Blood urea nitrogen (BUN) and creatinine (Cr) levels were 41.0 mg/dL (normal range, 8–23) and 4.3 mg/dL (normal range, 0.5–1.3), respectively. The fractional excretion of sodium into urine (FENa) was 6.6%. IgE levels increased to 921 IU/mL (normal range, 0–100). Complete blood count, white blood cell count was 5,500/mm3 (Neutrophil 4570/mm3, Lymphocyte 600/mm3, monocyte 280/mm3, basophil 10/mm3, and Eosinophil 90/mm3), hemoglobin was 11.3g/dL and platelet was 101,000/mm3. There was no eosinophilia when she stayed in hospital. On urinalysis, the color of urine was dark yellow. The pH was 8.5, protein 3+ (300 mg/dL), Red blood cell was 2+ (80/uL), white blood cell 3+ (500/uL). We diagnosed acute kidney injury and toxic hepatitis due to ginseng ingestion. She was administered hepatotonics and physiologic saline 80 mL/h. Her liver function improved, but oliguria, general oedema, and renal function (BUN 34.4 mg/dL, Cr 7.7 mg/dL) worsened the next day. We decided to perform haemodialysis and conducted a renal biopsy.
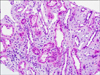
In the biopsy, we found interstitial mononuclear cell infiltration and oedema, which were compatible with acute interstitial nephritis (Fig. 1). After 5 rounds of haemodialysis, oliguria and oedema also improved. She was discharged from the hospital when she showed normal AST and ALT levels (16 IU/L and 26 IU/L, respectively), improved renal function (BUN: 48.3 mg/dL, Cr: 3.4 mg/dL), and increased urine output (2,930 mL/day). She visited the outpatient clinic after a week. Her renal function test showed completely normal results (BUN: 17.5 mg/dL, Cr: 1.0 mg/dL). Although the pathogenesis of Panax ginseng-induced toxic hepatitis and acute kidney injury remained unknown, several factors might be involved. The patient ingested ginseng with alcohol and she was dehydrated. It could be hypothesized that dehydration and alcohol consumption resulted in higher susceptibility to kidney and liver damage.
This is the first reported case of acute kidney injury associated with ingestion of ginseng. We emphasize that despite the known benefits of ginseng, it is necessary to ingest it in sufficiently hydrated condition, without concurrent consumption of harmful agents.
Figures and Tables
References
1. Pace R, Martinelli EM, Sardone N, DE Combarieu E. Metabolomic evaluation of ginsenosides distribution in Panax genus (Panax ginseng and Panax quinquefolius) using multivariate statistical analysis. Fitoterapia. 2015; 101:80–91.

2. Han MS, Han IH, Lee D, An JM, Kim SN, Shin MS, et al. Beneficial effects of fermented black ginseng and its ginsenoside 20(S)-Rg3 against cisplatin-induced nephrotoxicity in LLC-PK1 cells. J Ginseng Res. 2016; 40:135–140.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download