Abstract
Dexmedetomidine is a selective α-2 adrenoceptor agonist with anxiolytic, sedative, and analgesic properties that prolongs analgesia and decreases opioid-related side effects when used in neuraxial and perineural areas as a local anesthetics adjuvant. The current study was designed to evaluate the effects of a single perineural administration of dexmedetomidine without local anesthetics on narcotic consumption and pain intensity in patients with femoral shaft fractures undergoing surgery. This prospective randomized single-blind clinical trial was conducted in patients undergoing femoral fracture shaft surgery. Based on block permuted randomization, the patients were randomly divided into intervention and control groups. The intervention group received 100µg dexmedetomidine, for a femoral nerve block without any local anesthetics. Total intraoperative opioid consumption, postoperative opioid consumption, visual analogue score (VAS) for pain, and hemodynamic parameters were recorded and compared. Finally the data from 60 patients with a mean age of 30.4±12.3 were analyzed (90% male). There were no significant differences between the baseline characteristics of the two groups (p>0.05). The mean total consumption of narcotics was reduced during induction and maintenance of anesthesia in the intervention group (p<0.05). The amount of postoperative narcotics required showed a significant difference in the intervention group compared with the control group (p<0.05). It is likely that perineural administration of dexmedetomidine significantly not only reduced intra and postoperative narcotic requirement but also decreased postoperative pain intensity in patients undergoing femoral shaft surgery. Femoral blockade by dexmedetomidine can provide excellent analgesia while minimizing the side-effects of opioids.
Femoral nerve blocks are commonly used as a simple and conventional peripheral anesthetic method to perform procedures such as knee arthroscopy, anterior cruciate ligament reconstruction and femoral shaft fractures.12 In order to decrease postoperative pain and opioid requirements, single-shot peripheral nerve blocks (PNB) are routinely performed as an alternative to general anesthesia that are also associated with shorter hospital stays.3 Minimizing analgesic-related side effects and maximizing pain relief are vital to patient recovery after surgery. To reach this goal, multimodal approaches using different classes of analgesics are currently recommended.4 Various adjunct drugs, such as ketamine, antiemetic, pure opioidantagonist, opioid agonist–antagonist, and non-steroidal anti-inflammatory drugs have been used in different circumstances.5 It is known that alpha-2 agonist agents have some peripheral analgesic effects, so they can be used as a sole anesthetic or an adjuvant in this regard.6 Dexmedetomidine is a selective α-2 adrenoceptor agonist with anxiolytic, sedative, and analgesic properties that prolongs analgesia when used in neuraxial and intravenous (IV) infusion.78 As an off-label medication, dexmedetomidine has been administered as an adjunct to general or regional anesthesia in and out of the operating room for both medical and surgical procedures.9 The current study was designed to evaluate the efficacy of single perineural administration of dexmedetomidine without local anesthetics, on pain intensity and opioid consumption in patients with femoral shaft fractures undergoing surgery.
This prospective single-blind study was performed from April 2011 to December 2013 in Imam Hossein Hospital, Tehran, Iran.
The studied population included 18-65 year-old patients, with American Society of Anesthesiologists (ASA) physical status I–II, undergoing elective femoral shaft fracture surgery. The exclusion criteria were known allergies to α2-adrenergic agonists or any of the drugs used during the procedure (atracurium, propofol, morphine, midazolam, dexmedetomidine, lidocaine and fentanyl); renal or hepatic failure; planned intraoperative use of regional analgesia; addicted patients; consumption of psychotropic medication or an opioid agonist or antagonist in the 24 hours before surgery; history of recent treatment with α2-adrenergic agonist or antagonist; patients weighing less than 40 kg or more than 100 kg; and surgery durations of more than 3 hours.
The patients were randomly divided into intervention and control groups, using block permuted randomization. the intervention group included those who received the femoral block and control group involved those who did not. On arrival at the operating room, all patients were undergoing routine monitoring including mean arterial blood pressure (BP), baseline measurements of heart rate heart rate (HR), peripheral oxygen saturation (Spo2), and bispectral (BIS) index. To create a desirable BIS index, patients received a standardized anesthetic regimen that included premedication of IV midazolam 0.03-0.05 mg/kg and fentanyl 2-4 µg/kg. An IV administration of propofol titrate 1-2 mg/kg was started until the target level of 60-80 on the BIS index was obtained. In the intervention group, the femoral nerve was identified at a depth of 5 cm using a linear ultrasound (US) probe (Esaote, 10-18 MHz, Florence, Italy) or 5- to 12-Hz ultrasound probe (Toshiba™, Tokyo, Japan). A 20-21 gauge, 70-100 mm-long Stimuplex needle (B-Braun™, Melsungen, Germany) was used to perform the block and was connected to a neurostimulator (Stimuplex™; B-Braun) at a 2-Hz frequency and 0.5-mA intensity. A motor response was acquired to confirm the neural target and an anesthetic solution containing 100 µg dexmedetomidine in 20 ml distilled water was injected surrounding the nerve.
After performing the femoral blockade, the IV infusion of propofol, 100-200 µg/kg/min, was continued till 40-60 on the BIS index was achieved and endotracheal intubation was facilitated with atracurium 0.5 mg/kg and lidocaine 1.5 mg/kg. It used a dual proportional-integral-derivative algorithm for the IV administration of propofol. The input variable is the BIS value, whereby the system titrates propofol infusion to maintain a BIS between 40 and 60. The BIS was checked every 5 minutes and 20% of anesthetic infusion was reduced when BIS<40, while it was increased by 20% when BIS>60. If any patient was involved with tachycardia or hypertension more than 20% of its baseline for hemodynamic control, fentanyl was administrated with 1 µg/kg and repeated on failure of response after 10 min. At the end of surgery propofol was stopped and all patients underwent IV infusion analgesia.
Opioid consumption was recorded every one hour. Narcotic consumption was recorded in the recovery room and 12 and 24 hours after surgery. Blood pressures were recorded before, and at 0, 5, 10, 15, 30 minutes, then at 1, 2 and 3 hours after the start of the propofol infusion. Patients were then given a patient-controlled analgesia (PCA) delivery system provided by a 100 mL solution in the PCA reservoir bag containing 10 mg of morphine sulfate, 2 ml/hours, in normal saline. Pain was recorded using a visual analogue scale (VAS) for pain ranging from 0 (no pain) to 10 (worst pain) at hours 6, 12 and 24 after surgery. When a VAS score exceeded 3, rescue therapy was administered by providing 5 mg of IV morphine sulphate, followed as necessary by 2.5 mg boluses at 5-minute intervals. Adverse events were defined as bradycardia (heart rate <50 beats per minute), hypotension (a 30% decrease in systolic blood pressure in relation to the baseline value), and nausea or vomiting.
Finally, total intraoperative opioid consumption, postoperative opioid consumption, VAS and blood pressures were recorded and compared. Each patient was asked to grade satisfaction (Likert scale 1 to 5, in which grade 1 were completely satisfy; grade 2: relatively satisfy; grade 3: a little satisfy; grade 4: partly unsatisfied; grade 5: completely unsatisfied) with pain relief at the end of the PCA use.
Data analyses were done using the SPSS-22 software package. All data was expressed as mean±standard deviation. After testing for normality of pairwise differences with Shapiro-Wilk normality test, the effect of dexmedetomidine on propofol and opioid consumption and hemodynamic values were compared between groups using independent t tests. Hemodynamic data, BP means, are presented in a descriptive manner. A value of p<0.05 was considered statistically significant. Intra-group hemodynamic parameters were analyzed by using repeated measure ANOVA.
All authors adhered to the Helsinki - Ethical Principles for Medical Research throughout the study. The Ethics Committee of the Faculty of Medical School, Shahid Beheshti University of Medical Sciences, Tehran, Iran approved the study protocol (Ethical approval number: IR.SBMU.MSP.REC.1395.22). All patients were included after signing the written informed consent from. The trial was submitted in Iranian Registry of Clinical Trial at www.irct.ir and was received (IRCT code: IRCT201608019593N4)
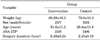
In total, 63 patients were considered eligible. One was excluded due to refusing to sign the consent form and the rest were randomly divided into two groups. The 62 patients were allocated into 2 intervention 2 groups including 30 and 32 patients. Furthermore, intervention was discontinued in 2 cases who had severe bradycardia after perineural injection of dexmedetomidine. Finally the data from 60 patients was analyzed. The CONSORT flowchart is presented in Fig. 1. Demographic data is summarized in Table 1. There were no significant differences between the two groups with respect to age, duration of surgery and weight (p>0.05).
Table 2 showed that intraoperative vital signs between two groups. There are some statistical differences in these regards.
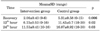
Table 3 includes recovery and postoperative VAS changes in studied patients. The mean VAS scores showed a significant difference immediately postoperatively and at the 6th, 12th, and 24th hours postoperatively in the intervention group in compare with the control group (p<0.05).
The assessment of narcotic consumption during induction and maintenance of anesthesia is shown in Table 4. The mean total consumption of narcotics was reduced during induction and maintenance of anesthesia in the intervention group: 216.6±11.3 µg versus 275±17.1 µg, in comparison with the control group, but the reduction was significant at the 3rd hour for intraoperative and total narcotic consumption (p<0.05).
Comparison of postoperative narcotic consumption in the studied patients is summarized in table 5. The amount of postoperative narcotics required showed a significant difference immediately postoperatively and at 12th and 24th hour postoperatively in the intervention group in comparison with the control group (p<0.05).
Regarding to the adverse effects, just one case showed severe bradycardia with a reduction of BIS after perineural injection of dexmedetomidine. In this case, perineural injection was performed after an accidental puncture of the femoral artery and sever bradycardia was treated with 1 mg of atropine.
In the current study, perineural administration of dexmedetomidine significantly not only reduced intra and postoperative narcotic requirements, but also decreased postoperative pain intensity in the patients undergoing femoral shaft surgery.
Perineural administration of anesthetic drugs is associated with limit considerable systematic absorption. Propofol is a suitable intravenous anesthetic agent for induction and maintenance of anesthesia during surgery that has some advantages including providing good control of anesthetic depth and rapid onset and recovery.10 Alfa-agonist drugs have been demonstrated as anesthetic adjuvant or sedative agents.11 Interest in dexmedetomidine as a potentially powerful adjunct to human anesthesia was generated by the report from Segal et al. (1988) that showed that dexmedetomidine produced more than a 90% reduction in halothane anesthetic requirements in rats through a postsynaptic alpha2-adrenergic receptor with little change in arterial blood gases and BP.12 It has been also reported that administration of dexmedetomidine significantly reduces the requirement for propofol.13 While, most of the previous studies have reported positive effects of dexmedetomidine as an adjuvant to the propofol requirement, the effects of the femoral blockade, by administering it alone, on the required amounts of propofol in maintaining the adequate depth of anesthesia was investigated in this study for the first time.13 The results from our study also showed that intraoperative and total narcotic requirements were lower in patients with the femoral blockade than in the group without the femoral blockade. Acute postoperative pain has various components such as inflammatory, nociceptive, and neuropathic issues because of direct nerve injury. These components are possible targets for postoperative analgesic strategies.14 The precise mechanism of action of perineural dexmedetomidine is not clear, but studies using other α2-adrenoceptor such as clonidine reported that α2-adrenoceptor-mediated vasoconstrictive effects may somehow explain the inflammatory responses, centrally mediated analgesia, and activities on the peripheral nerves. Also, it is well demonstrated that postoperative analgesia of clonidine or dexmedetomidine is based on activity-dependent inhibition of inwardly modifying potassium currents.1516 The analgesic effect of dexmedetomidine was not reversed by an alpha-adrenoceptor antagonist.17 In addition, dexmedetomidine induced perineural vasoconstriction with concomitant slower absorption of itself.14 Inhibiting potassium channel-mediated discharge of nociceptive C-fibres, attenuating the release of inflammatory mediators, and reducing ectopic neuronal discharge may justify how perineural dexmedetomidine alone can prolong the duration of analgesia. Prolonging the duration of postoperative analgesia by clonidine and dexmedetomidine, as a local anesthetic adjuvant, has been also demonstrated for brachial plexus blocks and infra-clavicular brachial plexus blocks, respectively.1618 Here we suggest that dexmedetomidine alone without any local anesthetics prolongs the duration of sensory blocks when administered perineurally to patients undergoing femoral anesthesia. It has generally been believed that the α2 agonists can reduce pain and opioid requirements after surgery, thus decreasing the incidence of opioid-related adverse effects.19 However, intravenous administration of dexmedetomidine exhibits synergy with regional that neuraxial analgesia effects of dexmedetomidine on narcotic consumption and controling pain in patients undergoing femoral surgery. We showed that perineural administration of dexmedetomidine significantly reduce intra and postoperative analgesic consumption. Furthermore, the lower mean VAS score in the intervention group indicated that perineural dexmedetomidine alone was associated with significantly lowering pain intensity postoperatively in comparison with control group. The recent systematic review and meta-analysis has indicated that dexmedetomidine as a neuraxial adjuvant was associated with a reduction in postoperative pain intensity within 24 hours.20 Brummett et al. conducted several animal studies to test the effects of additional dexmedetomidine to local anesthetics and showed that the duration of complete sensory and motor blockades were lengthened in the dexmedetomidine group.21 They also showed that perineural dexmedetomidine administration provided an increased duration of analgesia to a thermal stimulus when compared with a systemic control in a rat sciatic nerve block.17 Human studies have subsequently demonstrated that increased duration of a sensory blockade can be achieved by adding dexmedetomidine as an adjuvant to bupivacaine and levobupivacaine, in greater palatine and axillary brachial plexus nerve blocks, respectively.22 Unlike previous studies, we demonstrated that perineural dexmedetomidine alone resulted in patient's qualitatively ‘better’ analgesia or lower pain scores than without. In the present study, significantly higher patient satisfaction scores were reported by patients in the perineural dexmedetomidine group. There were not any undesired effects from perineural dexmedetomidine administration in the current study. However, one of our cases had severe bradycardia after perineural injection of dexmedetomidine, who underwent accidental puncture of femoral artery before perineural block. Abdel-Aleem et al. reported that intrathecal administration of dexmedetomidine with morphine significantly decreased postoperative nausea and vomiting and improved overall patient satisfaction after cesarean delivery.23 Well-designed multi-central research is still need to generalize the results of this study. Considering some other baseline characteristics such as history of drug abuse could also challenge the results.
It is likely that perineural administration of dexmedetomidine not only significantly reduced intra and postoperative narcotic requirement but also decreased postoperative pain intensity in the patients undergoing femoral shaft surgery. Femoral blockade by dexmedetomidine can provides excellent analgesia, minimizing the side-effects of opioids.
Figures and Tables
ACKNOWLEDGEMENTS
The authors would like to thank Miss Zahra Unesi and Miss Maedeh Sayad for their help.
References
1. Mulroy MF, Larkin KL, Batra MS, Hodgson PS, Owens BD. Femoral nerve block with 0.25% or 0.5% bupivacaine improves postoperative analgesia following outpatient arthroscopic anterior cruciate ligament repair. Reg Anesth Pain Med. 2001; 26:24–29.

2. Fletcher AK, Rigby AS, Heyes FL. Three-in-one femoral nerve block as analgesia for fractured neck of femur in the emergency department: a randomized, controlled trial. Ann Emerg Med. 2003; 41:227–233.

3. Williams BA, Kentor ML, Vogt MT, Williams JP, Chelly JE, Valalik S, et al. Femoral-sciatic nerve blocks for complex outpatient knee surgery are associated with less postoperative pain before same-day discharge: a review of 1,200 consecutive cases from the period 1996-1999. Anesthesiology. 2003; 98:1206–1213.

4. Joshi GP. Multimodal analgesia techniques and postoperative rehabilitation. Anesthesiol Clin North America. 2005; 23:185–202.

5. Lin TF, Yeh YC, Lin FS, Wang YP, Lin CJ, Sun WZ, et al. Effect of combining dexmedetomidine and morphine for intravenous patient-controlled analgesia. Br J Anaesth. 2009; 102:117–122.

6. Le Guen M, Liu N, Tounou F, Augé M, Tuil O, Chazot T, et al. Dexmedetomidine reduces propofol and remifentanil requirements during bispectral index-guided closed-loop anesthesia: a double-blind, placebo-controlled trial. Anesth Analg. 2014; 118:946–955.

7. Rancourt MP, Albert NT, Côté M, Létourneau DR, Bernard PM. Posterior tibial nerve sensory blockade duration prolonged by adding dexmedetomidine to ropivacaine. Anesth Analg. 2012; 115:958–962.

8. Gertler R, Brown HC, Mitchell DH, Silvius EN. Dexmedetomidine: a novel sedative-analgesic agent. Proc (Bayl Univ Med Cent). 2001; 14:13–21.

9. Mason KP, Lerman J. Review article: Dexmedetomidine in children: current knowledge and future applications. Anesth Analg. 2011; 113:1129–1142.
10. Burow BK, Johnson ME, Packer DL. Metabolic acidosis associated with propofol in the absence of other causative factors. Anesthesiology. 2004; 101:239–241.

11. Ohtani N, Kida K, Shoji K, Yasui Y, Masaki E. Recovery profiles from dexmedetomidine as a general anesthetic adjuvant in patients undergoing lower abdominal surgery. Anesth Analg. 2008; 107:1871–1874.

12. Segal IS, Vickery RG, Walton JK, Doze VA, Maze M. Dexmedetomidine diminishes halothane anesthetic requirements in rats through a postsynaptic alpha 2 adrenergic receptor. Anesthesiology. 1988; 69:818–823.

13. Sen S, Chakraborty J, Santra S, Mukherjee P, Das B. The effect of dexmedetomidine infusion on propofol requirement for maintenance of optimum depth of anaesthesia during elective spine surgery. Indian J Anaesth. 2013; 57:358–363.

14. Wang PH, Tsai CL, Lee JS, Wu KC, Cheng KI, Jou IM. Effects of topical corticosteroids on the sciatic nerve: an experimental study to adduce the safety in treating carpal tunnel syndrome. J Hand Surg Eur Vol. 2011; 36:236–243.

15. Ali Erdogan M, Polat A, Yucel A, Aydogan MS, Parlakpinar H, Tekin S, et al. Effects of perineural administration of dexmedetomidine in combination with levobupivacaine in a rat sciatic nerve block. Curr Ther Res Clin Exp. 2013; 74:74–78.

16. Pöpping DM, Elia N, Marret E, Wenk M, Tramèr MR. Clonidine as an adjuvant to local anesthetics for peripheral nerve and plexus blocks: a meta-analysis of randomized trials. Anesthesiology. 2009; 111:406–415.

17. Brummett CM, Hong EK, Janda AM, Amodeo FS, Lydic R. Perineural dexmedetomidine added to ropivacaine for sciatic nerve block in rats prolongs the duration of analgesia by blocking the hyperpolarization-activated cation current. Anesthesiology. 2011; 115:836–843.

18. Mirkheshti A, Saadatniaki A, Salimi A, Manafi Rasi A, Memary E, Yahyaei H. Effects of dexmedetomidine versus ketorolac as local anesthetic adjuvants on the onset and duration of infraclavicular brachial plexus block. Anesth Pain Med. 2014; 4:e17620.

19. Blaudszun G, Lysakowski C, Elia N, Tramèr MR. Effect of perioperative systemic α2 agonists on postoperative morphine consumption and pain intensity: systematic review and meta-analysis of randomized controlled trials. Anesthesiology. 2012; 116:1312–1322.

20. Wu HH, Wang HT, Jin JJ, Cui GB, Zhou KC, Chen Y, et al. Does dexmedetomidine as a neuraxial adjuvant facilitate better anesthesia and analgesia? A systematic review and meta-analysis. PLoS One. 2014; 9:e93114.

21. Brummett CM, Amodeo FS, Janda AM, Padda AK, Lydic R. Perineural dexmedetomidine provides an increased duration of analgesia to a thermal stimulus when compared with a systemic control in a rat sciatic nerve block. Reg Anesth Pain Med. 2010; 35:427–431.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download