Abstract
The emergence of drug-resistant tuberculosis (TB) is a growing problem worldwide. The lack of safe and effective drugs, together with the frequent development of adverse drug reactions can result in worse outcomes. Therefore, new TB drugs able to bolster the current TB treatment regimen are urgently required. Novel drugs that are effective and safe against Mycobacterium tuberculosis are required to reduce the number of drugs and the duration of treatment in both drug-susceptible TB and multi-drug-resistant (MDR)-TB. This review covers promising novel TB drugs and regimens that are currently under development. Bedaquiline and delamanid are the most promising novel drugs for the treatment of MDR-TB, each having a high efficacy and tolerability. However, the best regimen for achieving better outcomes and reducing adverse drug reactions remains yet to be determined, with safety concerns regarding cardiac events due to QT prolongation still to be addressed. Pretomanid is a novel drug that potentially shortens the duration of treatment in both drug-susceptible and drug-resistant TB. Many regimens consisting of injection free drugs with shorter treatment duration compared to the conventional treatment are now undergoing clinical trials. Therefore a simple and short treatment with higher efficacy, and lesser adverse drug reactions and drug-drug interaction is expected for patients with MDR-TB.
Tuberculosis (TB) is a chronic infectious disease that has been in existence for several millennia. However, it is still a major health concern in worldwide, with an estimated 10.4 million new cases and 1.4 million deaths in 2015.1 In 2015, there were an estimated 480,000 new cases of multi-drug-resistant (MDR)-TB presenting with resistance to both rifampin and isoniazid and an estimated 100,000 incident cases of rifampin-resistant TB (RR-TB).1 These new candidates for MDR-TB treatment could threaten TB control efforts due to increasing resistance to effective TB drugs.1 Moreover, the proportion of patients with extensively drug-resistant TB (XDR-TB), which is defined as MDR-TB with an additional resistance to any fluoroquinolone and at least one second-line injectable drug (kanamycin, amikacin, or capreomycin) was estimated at 9.5% of all cases of MDR-TB in 2015.1 Although the emergence of drug-resistant TB could threaten global health, there had been little progress in developing new TB drugs until recently.
Current TB drugs have been in use for more than 40 years.23 Although they show high efficacy and safety, long periods of treatment and many drugs in combination are needed to cure TB. It is more difficult to treat MDR-TB and XDR-TB due to the lack of effective drugs and adverse drug reactions caused by multi-drug therapies and long duration treatments.4567891011121314 Moreover, unsatisfactory treatment success rates were reported as 52% in MDR/RR-TB and 28% in XDR-TB in 2013.1 Therefore, there is a pressing need to develop new TB drugs and regimens for these patients.
In the past decade, many novel agents and regimens have been investigated in the treatment of TB with the aim to increase treatment success rates, whiles decreasing treatment duration, the number of drugs needed in combination, adverse drug reactions, and drug-drug interactions (Fig. 1).315161718 This article presents an update on new TB drugs and regimens for the treatment of drug-resistant TB.
Bedaquiline, a novel diarylquinoline compound that targets the proton pump of adenosine triphosphate (ATP) synthase in Mycobacterium tuberculosis (Mtb).1718 It has a potent anti-mycobacterial activity with a very low minimal inhibitory concentration (MIC) value of 0.003 mg/L against Mtb in vitro, although the MIC value (0.003-0.12 mg/L) varies according to the different bacterial subpopulations within drug susceptible and drug-resistant strains.19 The anti-mycobacterial activity is synergic in combination with primary TB drugs including isoniazid, rifampin, ethambutol, and pyrazinamide. It could also be synergic with new anti-TB drugs including SQ109,20 oxazolidinones (such as linezolid, sutezolid, AZD5847, and tedizolid) in combination with pretomanid which could improve the effectiveness of the regimen consisting of bedaquiline, pretomanid, and linezolid for XDR-TB (Nix-TB trial, ClinicalTrial.gov registration no. NCT02333799).21
In a phase IIa study of early bactericidal activity (EBA) for seven days in treatment-naïve sputum smear-positive pulmonary TB patients, the bactericidal activity was significant at a daily dose of 400 mg with a delayed onset of activity from day 4 to day 7 which were similar in magnitude of that of isoniazid and rifampin, but without the serious drug-related adverse reactions.22
In a phase IIb study for the efficacy and safety of bedaquiline in combination with a WHO-recommended background regimen for 8 weeks (C208 stage 1) and for 24 weeks (C208 stage 2), the bedaquiline group showed a significantly higher culture conversion rate compared to those in placebo group. The cure rate, defined by both WHO study protocols at 120 weeks, was also significantly higher in the bedaquiline group compared to those in placebo group (Table 1). Although drug-induced adverse reactions were no different in the two groups in both studies, more deaths were noticed in the bedaquiline group compared to the placebo group in the C208 stage 2 study (2 [2%] vs. 10 [13%], p=0.02). However, another study (C209) which enrolled patients with MDR-TB, including patients previously on second-line treatment and those with XDR-TB, in contrast to the preceding studies in which these patients were excluded, showed that the mortality rate in patients on treatment with bedaquiline was not higher (6.9%) than seen in previous study and the cure rate was sill comparable to previous study (72.2 % by study protocol definition and 61.0% by WHO definition). The study was limited in being a single arm and open-label one (Table 1).25 However, there still remain concerns about safety including a long half-life, hepatotoxicity, drug-induced QT prolongation, drug interactions with cytochrome P450 enzyme CYP3A4 inducers and about efficacies in patients with pre-XDR (MDR-TB with resistance against fluoroquinolone or second-line injectable drugs), XDR, HIV infected patients, patients younger than 18, and extrapulmonary TB.
In recent cohort studies, some of these safety and efficacy issues have been dealt with. Regarding efficacy, the culture conversion rate of the bedaquiline containing regimen was still high in patients with pre-XDR, XDR-TB and also HIV infected patients receiving antiretroviral therapy (ART).2627 Regarding safety, patients on bedaquiline in combination with various drugs including levofloxacin, clofazimine, and linezolid had no cardiac arrhythmia although there were corrected QT prolongations in the bedaquiline group. Regarding drug interactions in patients on ART, no serious adverse drug reactions including hepato- and renal-toxicity and cardiac arrhythmia were reported. These studies were limited because a small number of patients were used, with a short follow-up period. Therefore additional studies about these issues are still needed.
Resistance to this drug and cross resistance to clofazimine is another concern. Bedaquiline resistance is caused by mutations in atpE encoding a part of the F0 subunit of ATP synthase which is the target of the drug and rv0678.1928 Mutation in rv0678 causes transcriptional upregulation of mmpS5 and mmpL5 resulting in cross-resistance to clofazimine through the activation of MmpL proteins which are multisubstrate efflux pumps for which bedaquiline and clofazimine function as possible substrates.28 However, the clinical impact on drug resistance caused by this mutation and on the use of efflux pump inhibitors such as verapamil and protonophores, which may restore drug susceptibility, are yet to be determined.1829
Based on previous studies, bedaquiline is recommended for adult patients with pulmonary MDR-TB if the patients cannot have an effective regimen because of intolerance, resistance, or an unavailability of other TB drugs.303132 Routine use of this drug for patients with MDR-TB is not recommended. Although there is no best regimen for this drug, it should be added to the WHO-recommended regimen. A close monitoring for adverse drug reactions of this drug and unexpected interactions with other drugs is also recommended.
Delamanid is a novel nitroimidazole compound which overcomes the mutagenicity of the drug and targets the mycobacterial cell wall by interrupting the synthesis of methoxy-mycolic and keto-mycolic acids.1633 It shows potent anti-mycobacterial activity with very low MICs ranging from 0.006 to 0.024 µg/mL in vitro to both drug-susceptible and drug-resistant Mtb strains which were 4-256 times lower than those of rifampin, isoniazid, ethambutol, streptomycin, CGI-17341, and pretomanid.33
In a phase IIa trial, a 14-day EBA study for evaluation of the anti-TB activity, pharmacokinetics, and toxicity of the drug with a dose of 100, 200, 300, or 400 mg delamanid taken once daily in patients with treatment-naïve smear-positive pulmonary TB showed a significant and continuous bactericidal activity.34 However, there was no dose-dependent bactericidal activity in this study: there was increasing bactericidal activity up to 300 mg daily, but it attenuated at 400 mg daily.34 The fall of the colony forming unit (CFU) of Mtb which is a method for measuring anti-TB activity in the EBA study reached significant levels on day 3 and then continued at a magnitude similar to the standard four drug regimen.34
In phase IIb, a randomized, placebo-controlled, multinational study in patients with pulmonary MDR-TB showed higher culture conversion rates on both Mycobacteria Growth Indicator Tube (MGIT) and solid medium in patients who received delamanid for 8 weeks in combination with WHO recommended optimized background regimen (OBR) than in patients on placebo in combination with OBR.35 A significant rapid culture conversion was also shown in both the MGIT system and solid medium in this study (Table 2).3536
A subsequent open-label extension trial showed that outcomes in patients with more than 6 months (6-8 months) of delamanid treatment were significantly higher than in patients with less than 2 months of delamanid or placebo.36 The mortality rate in patients with longer use of delamanid was significantly lower than in patients with shorter use of delamanid. However, in a subgroup analysis for patients with XDR-TB, there was no difference in favorable outcomes between the two groups (Table 2).36
Although two previous studies showed the efficacy of delamanid treatment in combination with OBR for 6 months, there remains safety concerns including QT prolongation especially in patients with hypoalbuminemia (<2.8 mg/dL) and efficacy concerns in the elderly, children, adolescents under 18 years, pregnant women, breast-feeding women, and patients with extrapulmonary TB.16
The recommended use of delamanid for treating TB is similar with that of bedaquiline.3237 Delamanid can strengthen the WHO-recommended MDR-TB regimen in patients who cannot have an effective regimen due to resistance, intolerance, and lack of availability of TB drugs. Although there is no data comparing the clinical efficacy and safety of delamanid and bedaquiline, delamanid might be more favorable in combination with CYP3A4 inducers because there is less interaction with this liver enzyme compared to bedaquiline.16 However, in patients with hypoalbuminemia, bedaquiline is favorable because delamanid causes QT prolongation in these patients.16
Current guidelines have not recommended combining bedaquiline and delamanid because there is no evidence regarding efficacy or safety risks including QT prolongation. However, this combination could be needed when an effective treatment regimen cannot be used due to drug resistance and intolerance to second-line TB drugs. Recently, two cases were reported which were both XDR-TB and extremely complicated.38394041 Both cases showed favorable clinical, microbiological, and radiological response after six months of treatment. Regarding safety, one patient experienced a transient QT prolongation which resulted in a temporary discontinuation of bedaquiline, but the drug was restarted in addition to verapamil without a recurrence of QT prolongation.41 Although these two patients are not enough to make conclusions about combination of these two drugs, better data can be expected in clinical trials about this issue (ClinicalTrials.gov identifier NCT02583048 and NCT02754765).
Pretomanid is a novel bicyclic nitroimidazole which has potent anti-mycobacterial activity against both drug-susceptible and -resistant Mtb with a low MIC ranging from 0.015 to 0.25 mg/mL, comparable to that of isoniazid.42 The mechanism of action of this drug is the disruption of the formation of mycolic acid, and bactericidal activity of this drug was shown in both replicating and hypoxic-static Mtb. In hypoxic conditions, the mechanism of anti-mycobacterial activity has been shown to be intracellular nitric oxide release.43 Based on the bactericidal and sterilizing activities of this drug in combination with moxifloxacin and pyrazinamide in a murine model, the efficacy of this regimen in patients with pulmonary TB was shown in a phase IIa 14-day EBA study and phase IIb multicenter, partly randomized clinical trial for 8 weeks of treatment.4445 In a phase IIa 14-day EBA study, this regimen showed comparable bactericidal activity compared to that of standard regimen and superior to those of other regimens including bedaquiline, bedaquiline-pyrazinamide, and bedaquiline-pretomanid.44 In a phase IIb study for 8 weeks of treatment, the bactericidal activity of this regimen measured by decreasing sputum colony counts during treatment period in patients with drug susceptible pulmonary TB were significantly higher than with a standard regimen.45 Moreover, in this trial, the bactericidal activity in patients with MDR-TB being treated with this regimen was comparable to that in patients with drug susceptible TB being treated with the standard regimen. Regarding safety, adverse drug reactions were not different among treatment groups with no events of QT prolongation of more than 500 ms. Although this regimen showed good efficacy and safety in previous studies, a phase III, open-label, partially randomized trial done by the TB alliance, a nonprofit product development partnership with a large portfolio of new TB drugs, for this regimen has been suspended at enrollment of participants (ClinicalTrials.gov identifier NCT02342886).
Sutezolid (PNU-100480) is a novel oxazolidinone analogue. Linezolid is the first agent in this class with great efficacy against MDR-TB, although it has been used off-label, and serious adverse drug reactions including peripheral neuropathy, optic neuropathy, and myelosuppression limit the long term use of this drug. Sutezolid showed more potent anti-mycobacterial activity than linezolid against both drug-susceptible and drug-resistant strains of Mtb. In the murine TB model, this drug alone or in combination with first-line TB drugs and moxifloxacin showed better initial bactericidal activity and sterilizing activity than linezolid.4647 In phase I trials, this drug was safe and well tolerated at up to 1,500 mg in a single dose and up to 1,200 mg in combination for 14 or 28 days. In these trials, bactericidal activity measured by ex vivo whole-blood culture was maximized at the 600 mg, twice daily dose and augmented by pyrazinamide.4849 In phase IIa trials in patients with smear positive pulmonary TB, the dosages, the 600 mg, twice daily and 1,200 mg daily doses, were safe, well tolerated, and readily showed significant bactericidal activity in sputum and blood.50 Further studies for efficacy and safety about this drug and its combinations with other drugs are needed.
Shortening the duration of MDR-TB treatment can enhance adherence to treatment, decrease side effects, and reduce costs that could be a big advancement in TB control. Finally it could result in lower default rates and increase treatment success rates. An observational study in applying shorter treatment regimens known as the “Bangladesh regimen,” consisting of 4 months of the intensive phase (kanamycin, prothionamide, isoniazid, gatifloxacin, ethambutol, pyrazinamide, and clofazimine) and 5 months of the maintenance phase (gatifloxacin, ethambutol, pyrazinamide, and clofazimine) achieved a high cure rate (88%), and the effect was mostly maintained for up to 2 years after treatment completion.5152 A similar regimen with a duration of 12 months also reported a high cure rate (89%) in Cameroon and Niger.5354 Although these studies had limitations as no control group which consists of comparable patients on the longer WHO-recommended conventional treatment, success rates were much higher compared to previous studies about treatment outcomes of MDR-TB used with a WHO recommended longer treatment, and it offers encouraging resluts about reducing the duration of treatment for MDR-TB.55 After a reanalysis of all the data from previous studies, the WHO recommends a shorter MDR-TB regimen in patients with MDR-TB except those with confirmed resistance, suspected ineffectiveness, intolerance, or previous exposure for more than 1 months to drugs in the shorter regimen, pregnancy, extrapulmonary TB, or a lack of availability of drugs for the shorter regimen.55 However, the shorter regimen for MDR-TB should be cautiously applied considering the drug resistance patterns on an individual basis.56 In a recent study of drug resistance patterns among MDR-TB patients in Busan, Ulsan, and Gyeongsangnam-do in Korea, only 50 % of patients were suitable candidates for the shorter MDR-TB treatment regimen.57 For making further decisions about the shorter MDR-TB treatment, the STREAM trial is now in progress for a comparison of the efficacy and safety of the conventional WHO recommended individualized MDR-TB regimen with the shorter MDR-TB regimens consisting of 4KCMEHZP/5MEZC (moxifloxacin instead of gatifloxacin) and the bedaquiline-containing regimens.58
Several trials for shortening the treatment of MDR-TB using new TB drugs is ongoing. Regarding the combination of bedaquiline and pretomanid, a phase IIa trial, 14-day EBA study of bedaquiline-pretomanid-pyrazinamide in patients with treatment-naïve smear-positive pulmonary TB, showed superior anti-mycobacterial activity compared to bedaquiline-pretomanid-pyrazinamide-clofazimine and bedaquiline-pyrazinamide-clofazimine and comparable anti-mycobacterial activity to the standard regimen.59 Currently, a phase IIb trial for evaluation of the efficacy, safety, and tolerability of the regimen consisting of bedaquiline-pretomanid-moxifloxacin-pyrazinamide in patients with drug-sensitive TB and MDR-TB is ongoing by the TB alliance (ClinicalTrials.gov identifier NCT02193776). The Nix-TB trial for using these two new TB drug combinations is ongoing by the TB alliance. This trial is a phase III open-label trial with a single arm for evaluation of the efficacy and safety of bedaquiline-pretomanid-linezolid regimen in patients with XDR-TB and non-responsive MDR-TB for 6 months with an option of 9 months (ClinicalTrials.gov identifier NCT02333799). The NEXT trial is a phase III open-label randomized control trial in South Africa for evaluating the efficacy and safety of the regimen consisting of 6-9 months of linezolid, bedaquiline, levofloxacin, pyrazinamide, and ethionamide/high dose isoniazid in patients with MDR-TB (ClinicalTrials.gov identifier NCT02454205). The MDR-END trial is a phase II open-label randomized control trial in South Korea for evaluating the efficacy and safety of the regimen consisting of delamanid, linezolid, levofloxacin, and pyrazinamide for 9-12 months in patients with quinolone-sensitive MDR-TB. Regimens in these studies are short and simple using only oral drugs. Therefore these regimens could strengthen the MDR-TB treatment while increasing treatment success rates, and reducing side effects and the cost of treatment.
The emergence of MDR/XDR-TB is a growing problem worldwide. Currently, MDR-TB treatment requires the use of many drugs including injectables and a prolonged duration of treatment, causing many side effects. Advances in TB drug development over the past decade are leading to the development of enhanced MDR-TB treatments with simple and short regimens. Before widespread usage of these new drugs, however, many issues must be addressed, including dose optimization, selection of the best regimens with increased efficacy and reduced drug interactions, and various safety concerns. Additionally, efforts must be made to reduce the development of resistance to these valuable new TB drugs during treatment.
Figures and Tables
FIG. 1
New tuberculosis drugs in the current development pipeline. Details for projects and ongoing projects without a lead compound series can be viewed at the Working Group on New TB Drugs (http://www.newtbdrugs.org/). GPL: good laboratory practice, OBR: optimized background regimen.

TABLE 1
Sputum culture conversion rates and treatment outcomes in C208 stage 1, C208 stage 2, and C209 phase IIb studies for evaluation of the efficacy and safety of bedaquiline in patients with multi-drug resistant tuberculosis232425
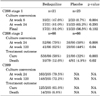
C208 stage 1 and C208 stage 2: randomized, double-blind, placebo-controlled studies for evaluation of the efficacy of bedaquiline for 2 months (C208 stage 1) or 6 months (C208 stage 2) treatment or placebo in combination with a background regimen.
C209: an open-label, single-arm trial for evaluation of the efficacy of bedaquiline for 6 months treatment with a background regimen.
References
1. World Health Organization. Global tuberculosis report 2016. Geneva: WHO;2016.
3. Zumla A, Nahid P, Cole ST. Advances in the development of new tuberculosis drugs and treatment regimens. Nat Rev Drug Discov. 2013; 12:388–404.

4. Keshavjee S, Gelmanova IY, Farmer PE, Mishustin SP, Strelis AK, Andreev YG, et al. Treatment of extensively drug-resistant tuberculosis in Tomsk, Russia: a retrospective cohort study. Lancet. 2008; 372:1403–1409.

5. Kim DH, Kim HJ, Park SK, Kong SJ, Kim YS, Kim TH, et al. Treatment outcomes and long-term survival in patients with extensively drug-resistant tuberculosis. Am J Respir Crit Care Med. 2008; 178:1075–1082.

6. Kwon YS, Kim YH, Suh GY, Chung MP, Kim H, Kwon OJ, et al. Treatment outcomes for HIV-uninfected patients with multi-drug-resistant and extensively drug-resistant tuberculosis. Clin Infect Dis. 2008; 47:496–502.

7. Mitnick CD, Shin SS, Seung KJ, Rich ML, Atwood SS, Furin JJ, et al. Comprehensive treatment of extensively drug-resistant tuberculosis. N Engl J Med. 2008; 359:563–574.

8. Johnston JC, Shahidi NC, Sadatsafavi M, Fitzgerald JM. Treatment outcomes of multidrug-resistant tuberculosis: a systematic review and meta-analysis. PLoS One. 2009; 4:e6914.

9. Orenstein EW, Basu S, Shah NS, Andrews JR, Friedland GH, Moll AP, et al. Treatment outcomes among patients with multi-drug-resistant tuberculosis: systematic review and meta-analysis. Lancet Infect Dis. 2009; 9:153–161.

10. Dheda K, Shean K, Zumla A, Badri M, Streicher EM, Page-Shipp L, et al. Early treatment outcomes and HIV status of patients with extensively drug-resistant tuberculosis in South Africa: a retrospective cohort study. Lancet. 2010; 375:1798–1807.

11. Jacobson KR, Tierney DB, Jeon CY, Mitnick CD, Murray MB. Treatment outcomes among patients with extensively drug-resistant tuberculosis: systematic review and meta-analysis. Clin Infect Dis. 2010; 51:6–14.

12. Kim DH, Kim HJ, Park SK, Kong SJ, Kim YS, Kim TH, et al. Treatment outcomes and survival based on drug resistance patterns in multidrug-resistant tuberculosis. Am J Respir Crit Care Med. 2010; 182:113–119.

13. Mitnick CD, Franke MF, Rich ML, Alcantara Viru FA, Appleton SC, Atwood SS, et al. Aggressive regimens for multidrug-resistant tuberculosis decrease all-cause mortality. PLoS One. 2013; 8:e58664.

14. Pietersen E, Ignatius E, Streicher EM, Mastrapa B, Padanilam X, Pooran A, et al. Long-term outcomes of patients with extensively drug-resistant tuberculosis in South Africa: a cohort study. Lancet. 2014; 383:1230–1239.

15. Kwon YS, Jeong BH, Koh WJ. Tuberculosis: clinical trials and new drug regimens. Curr Opin Pulm Med. 2014; 20:280–286.
16. Kwon YS, Jeong BH, Koh WJ. Delamanid when other anti-tuberculosis-treatment regimens failed due to resistance or tolerability. Expert Opin Pharmacother. 2015; 16:253–261.

17. Kwon YS, Koh WJ. Synthetic investigational new drugs for the treatment of tuberculosis. Expert Opin Investig Drugs. 2016; 25:183–193.

18. Cholo MC, Mothiba MT, Fourie B, Anderson R. Mechanisms of action and therapeutic efficacies of the lipophilic antimycobacterial agents clofazimine and bedaquiline. J Antimicrob Chemother. 2017; 72:338–353.

19. Andries K, Verhasselt P, Guillemont J, Göhlmann HW, Neefs JM, Winkler H, et al. A diarylquinoline drug active on the ATP synthase of Mycobacterium tuberculosis. Science. 2005; 307:223–227.

20. Reddy VM, Einck L, Andries K, Nacy CA. In vitro interactions between new antitubercular drug candidates SQ109 and TMC207. Antimicrob Agents Chemother. 2010; 54:2840–2846.

21. Tasneen R, Betoudji F, Tyagi S, Li SY, Williams K, Converse PJ, et al. Contribution of oxazolidinones to the efficacy of novel regimens containing bedaquiline and pretomanid in a mouse model of tuberculosis. Antimicrob Agents Chemother. 2015; 60:270–277.

22. Rustomjee R, Diacon AH, Allen J, Venter A, Reddy C, Patientia RF, et al. Early bactericidal activity and pharmacokinetics of the diarylquinoline TMC207 in treatment of pulmonary tuberculosis. Antimicrob Agents Chemother. 2008; 52:2831–2835.

23. Diacon AH, Pym A, Grobusch M, Patientia R, Rustomjee R, Page-Shipp L, et al. The diarylquinoline TMC207 for multidrug-resistant tuberculosis. N Engl J Med. 2009; 360:2397–2405.

24. Diacon AH, Pym A, Grobusch MP, de los Rios JM, Gotuzzo E, Vasilyeva I, et al. Multidrug-resistant tuberculosis and culture conversion with bedaquiline. N Engl J Med. 2014; 371:723–732.

25. Pym AS, Diacon AH, Tang SJ, Conradie F, Danilovits M, Chuchottaworn C, et al. Bedaquiline in the treatment of multi-drug-and extensively drug-resistant tuberculosis. Eur Respir J. 2016; 47:564–574.

26. Ndjeka N, Conradie F, Schnippel K, Hughes J, Bantubani N, Ferreira H, et al. Treatment of drug-resistant tuberculosis with bedaquiline in a high HIV prevalence setting: an interim cohort analysis. Int J Tuberc Lung Dis. 2015; 19:979–985.

27. Guglielmetti L, Le Dû D, Jachym M, Henry B, Martin D, Caumes E, et al. Compassionate use of bedaquiline for the treatment of multidrug-resistant and extensively drug-resistant tuberculosis: interim analysis of a French cohort. Clin Infect Dis. 2015; 60:188–194.

28. Hartkoorn RC, Uplekar S, Cole ST. Cross-resistance between clofazimine and bedaquiline through upregulation of MmpL5 in Mycobacterium tuberculosis. Antimicrob Agents Chemother. 2014; 58:2979–2981.

29. Pule CM, Sampson SL, Warren RM, Black PA, van Helden PD, Victor TC, et al. Efflux pump inhibitors: targeting mycobacterial efflux systems to enhance TB therapy. J Antimicrob Chemother. 2016; 71:17–26.

30. Centers for Disease Control and Prevention. Provisional CDC guidelines for the use and safety monitoring of bedaquiline fumarate (Sirturo) for the treatment of multi-drug-resistant tuberculosis. MMWR Recomm Rep. 2013; 62:1–12.
31. World Health Organization. The use of bedaquiline in the treatment of multidrug-resistant tuberculosis: interim policy guidance. Geneva: WHO;2016.
32. World Health Organization. Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis. Geneva: WHO;2014.
33. Matsumoto M, Hashizume H, Tomishige T, Kawasaki M, Tsubouchi H, Sasaki H, et al. OPC-67683, a nitro-dihydro-imidazooxazole derivative with promising action against tuberculosis in vitro and in mice. PLoS Med. 2006; 3:e466.

34. Diacon AH, Dawson R, Hanekom M, Narunsky K, Venter A, Hittel N, et al. Early bactericidal activity of delamanid (OPC-67683) in smear-positive pulmonary tuberculosis patients. Int J Tuberc Lung Dis. 2011; 15:949–954.

35. Gler MT, Skripconoka V, Sanchez-Garavito E, Xiao H, Cabrera-Rivero JL, Vargas-Vasquez DE, et al. Delamanid for multidrug-resistant pulmonary tuberculosis. N Engl J Med. 2012; 366:2151–2160.

36. Skripconoka V, Danilovits M, Pehme L, Tomson T, Skenders G, Kummik T, et al. Delamanid improves outcomes and reduces mortality in multidrug-resistant tuberculosis. Eur Respir J. 2013; 41:1393–1400.

37. World Health Organization. The use of delamanid in the treatment of multidrug-resistant tuberculosis: interim policy guidance. Geneva: WHO;2014.
38. Lachâtre M, Rioux C, Le Dû D, Fréchet-Jachym M, Veziris N, Bouvet E, et al. Bedaquiline plus delamanid for XDR tuberculosis. Lancet Infect Dis. 2016; 16:294.

39. Tadolini M, Lingtsang RD, Tiberi S, Enwerem M, D'Ambrosio L, Sadutshang TD, et al. First case of extensively drug-resistant tuberculosis treated with both delamanid and bedaquiline. Eur Respir J. 2016; 48:935–938.

40. Tadolini M, Lingtsang RD, Tiberi S, Enwerem M, D'Ambrosio L, Sadutshang TD, et al. Cardiac safety of extensively drug-resistant tuberculosis regimens including bedaquiline, delamanid and clofazimine. Eur Respir J. 2016; 48:1527–1529.

41. Migliori GB, Pontali E, Sotgiu G, Centis R, D'Ambrosio L, Tiberi S, et al. Combined use of Delamanid and Bedaquiline to treat multidrug-resistant and extensively drug-resistant tuberculosis: a systematic review. Int J Mol Sci. 2017; 18:E341.

42. Stover CK, Warrener P, VanDevanter DR, Sherman DR, Arain TM, Langhorne MH, et al. A small-molecule nitroimidazopyran drug candidate for the treatment of tuberculosis. Nature. 2000; 405:962–966.

43. Singh R, Manjunatha U, Boshoff HI, Ha YH, Niyomrattanakit P, Ledwidge R, et al. PA-824 kills nonreplicating Mycobacterium tuberculosis by intracellular NO release. Science. 2008; 322:1392–1395.

44. Diacon AH, Dawson R, von Groote-Bidlingmaier F, Symons G, Venter A, Donald PR, et al. 14-day bactericidal activity of PA-824, bedaquiline, pyrazinamide, and moxifloxacin combinations: a randomised trial. Lancet. 2012; 380:986–993.

45. Dawson R, Diacon AH, Everitt D, van Niekerk C, Donald PR, Burger DA, et al. Efficiency and safety of the combination of moxifloxacin, pretomanid (PA-824), and pyrazinamide during the first 8 weeks of antituberculosis treatment: a phase 2b, open-label, partly randomised trial in patients with drug-susceptible or drug-resistant pulmonary tuberculosis. Lancet. 2015; 385:1738–1747.

46. Williams KN, Brickner SJ, Stover CK, Zhu T, Ogden A, Tasneen R, et al. Addition of PNU-100480 to first-line drugs shortens the time needed to cure murine tuberculosis. Am J Respir Crit Care Med. 2009; 180:371–376.

47. Williams KN, Stover CK, Zhu T, Tasneen R, Tyagi S, Grosset JH, et al. Promising antituberculosis activity of the oxazolidinone PNU-100480 relative to that of linezolid in a murine model. Antimicrob Agents Chemother. 2009; 53:1314–1319.

48. Wallis RS, Jakubiec W, Kumar V, Bedarida G, Silvia A, Paige D, et al. Biomarker-assisted dose selection for safety and efficacy in early development of PNU-100480 for tuberculosis. Antimicrob Agents Chemother. 2011; 55:567–574.

49. Wallis RS, Jakubiec WM, Kumar V, Silvia AM, Paige D, Dimitrova D, et al. Pharmacokinetics and whole-blood bactericidal activity against Mycobacterium tuberculosis of single doses of PNU-100480 in healthy volunteers. J Infect Dis. 2010; 202:745–751.

50. Wallis RS, Dawson R, Friedrich SO, Venter A, Paige D, Zhu T, et al. Mycobactericidal activity of sutezolid (PNU-100480) in sputum (EBA) and blood (WBA) of patients with pulmonary tuberculosis. PLoS One. 2014; 9:e94462.

51. Van Deun A, Maug AK, Salim MA, Das PK, Sarker MR, Daru P, et al. Short, highly effective, and inexpensive standardized treatment of multidrug-resistant tuberculosis. Am J Respir Crit Care Med. 2010; 182:684–692.

52. Aung KJ, Van Deun A, Declercq E, Sarker MR, Das PK, Hossain MA, et al. Successful ‘9-month Bangladesh regimen’ for multi-drug-resistant tuberculosis among over 500 consecutive patients. Int J Tuberc Lung Dis. 2014; 18:1180–1187.

53. Kuaban C, Noeske J, Rieder HL, Aït-Khaled N, Abena Foe JL, Trébucq A. High effectiveness of a 12-month regimen for MDR-TB patients in Cameroon. Int J Tuberc Lung Dis. 2015; 19:517–524.

54. Piubello A, Harouna SH, Souleymane MB, Boukary I, Morou S, Daouda M, et al. High cure rate with standardised short-course multidrug-resistant tuberculosis treatment in Niger: no relapses. Int J Tuberc Lung Dis. 2014; 18:1188–1194.

55. World Health Organization. WHO treatment guidelines for drug-resistant tuberculosis. 2016 update. Geneva: WHO;2016.
56. Sotgiu G, Tiberi S, Centis R, D'Ambrosio L, Fuentes Z, Zumla A, et al. Applicability of the shorter ‘Bangladesh regimen’ in high multidrug-resistant tuberculosis settings. Int J Infect Dis. 2017; 56:190–193.

57. Mok JH, Kang BH, Lee T, Lee HK, Jang HJ, Cho YJ, et al. Additional Drug Resistance Patterns among Multidrug-Resistant Tuberculosis Patients in Korea: Implications for Regimen Design. J Korean Med Sci. 2017; 32:636–641.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download