Abstract
The aim of this study was to better understand the frequency of autoimmune thyroid and diabetes antibodies in patients with type 1 diabetes mellitus (T1DM) compared with their siblings. Glutamic acid decarboxylase antibodies (GADA), islet cell antibodies (ICA), insulin autoantibodies (IAA), and thyroid autoantibodies were studied in all subjects. The rates of positive GADA and IAA were significantly higher in probands compared to in siblings (p<0.001) or controls (p<0.001). All pancreatic autoantibodies were not significantly different between the siblings and the healthy controls. Thyroid antiperoxidase antibody (TPOAb) and antithyroglobulin antibody (TGAb) were significantly different between the probands and the control subjects (p=0.002 and p=0.018, respectively). The rates of TPOAb and TGAb positivity in siblings were higher than in those of the controls, but there was no significant difference between the two groups. However, thyroid autoimmunity (TA) was significantly different among the groups (p=0.004). Siblings of the TA-positive probands were shown to have a greater prevalence of thyroid antibodies than did the controls (p=0.022), but siblings of the TA-negative probands did not have such a prevalence compared with the control subjects. The prevalence of pancreatic and thyroid antibodies positivity in probands was statistically significant compared with the siblings and the controls. Siblings of TA-positive probands revealed a greater prevalence of thyroid antibodies than did the controls. Therefore, the screening for TA in siblings, particularly siblings of TA-positive probands, is as important as it is in probands.
Type 1 diabetes mellitus (T1DM) results from lack of insulin secretion caused by the destruction of pancreatic β cells.1 Most patients with T1DM have the diabetes autoantibodies such as insulin autoantibodies (IAA), glutamic acid decarboxylase (GADA), and islet cell antibody (ICA).2 T1DM patients are at an increased risk for additional autoimmune diseases like that Graves' disease, Hashimoto's thyroiditis, and Addison's disease.3 The most common autoimmune disorder related with T1DM is autoimmune thyroid disease (AIT).4567 The frequency of thyroid autoantibody positivity in children with T1DM has been reported in about 50% in different ethnicity.8 Thyroid disorders occurred within 3 to 4 years in fifty percent of the thyroid autoantibody positive subjects.59 It has been suggested that T1DM and AIT have common genetic sources since they often co-occur in patients and families.10 The risk for this autoimmune disorder is known to increase in first-degree relatives of T1DM subjects, and 8% of first-degree families have AIT.1112
To our best knowledge, the frequency of autoantibodies for diabetes and thyroid in Korean children with T1DM and their siblings have not been investigated. So, in this study, we aim to investigate the frequency of autoimmune thyroid and diabetes antibodies in patients of T1DM, their siblings, and healthy controls.
The subject pool consisted of 31 children and adolescents with T1DM who visited the Pediatric Endocrine Clinic between July 2011 and December 2013. All subjects satisfied the criteria of the American Diabetes Association for T1DM.3 Forty siblings of T1DM patients were recruited and monozygotic twin sibling pairs were eliminated from this study. The 40 healthy controls with no family history of autoimmune disorder (autoimmune thyroiditis, T1DM etc) were selected from the same ethnic population and were matched with the siblings for age and sex. The control subjects had no chronic disease or any other autoimmune disorder, such as thyroiditis and T1DM. This study had the approval of the Institutional Review Board (CNUH-2011-058).
Fasting blood glucose, glycosylated hemoglobin (HbA1c), GADA, ICA, and IAA were evaluated at the time of diagnosis. AIT evaluation was done using measurements of free thyroxine (FT4), thyroid stimulating hormone (TSH), thyroid antiperoxidase antibody (TPOAb), antithyroglobulin antibody (TGAb), and TSH receptor antibodies (TSHRAb). The mean duration of diabetes occurrence was 2.3 years when AIT screening was done. The positivity of AIT was confirmed by the following criteria: TSH levels outside the assay reference (range 0.35–5.5 µIU/mL) plus positive thyroid antibodies. Thyroid autoimmunity (TA) was determined by a positive test for at least one thyroid autoantibody. GADA was examined by a radioimmunoassay kit (RSR Ltd., Cardiff, UK), IAA by an enzyme immunoassay kit (Orgentec diagnostika, Mainz, Germany), and ICA by the indirect fluorescent antibody technique (SCIMEDX, Denville, NJ, USA). TPOAb and TGAb were assessed using an electrochemiluminescence immunoassay kit (COBAS, Roche Diagnostics GmbH, Mannheim, Germany) and TSHRAb was determined by using a radioimmunoassay (RSR Ltd, Cardiff, UK).
Data was presented as mean±standard deviation or proportion (%). The one-way ANOVA test was done to compare continuous variables. The chi-square test or Fisher's exact probability test depending on the number of the cases was used to compare frequencies of autoimmune diseases among the groups. Results showed diabetes autoantibody positivity and TA. All statistical analyses were studied with IBM SPSS ver. 21.0 (IBM Co., Armonk, NY, USA). The p value of less than 0.05 was deemed significant.
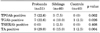
The clinical data of the study population is summarized in Table 1. Thirty one T1DM patients were enrolled in our study, 13 were boys (41.9%) and 18 (58.1%) were girls. Ages and the ratio of females to males were similar in siblings and control subjects. Blood glucose and HbA1c levels were significantly higher in T1DM subjects compared to their siblings and the control subjects (p<0.001). However, the values of TSH and FT4 among the groups were not significantly different. Twenty five T1DM patients (80.6%) had positivity for GADA, 11 (35.5%) for IAA, and 2 (6.5%) for IAA, respectively. Only one sibling showed GADA positivity (2.5%), and all siblings of probands were revealed to be negative for IAA and ICA. Of the control groups, two subjects (5%) had GADA positivity, but none had positivity for IAA and ICA. So the frequency of GADA and IAA positivity was significantly higher in probands compared to the siblings and the controls (p<0.001). All pancreatic autoantibodies were not significantly different between the siblings and the controls.
The prevalence of thyroid autoantibodies in probands, their siblings and the control subjects is shown in Table 2. The positivity of TPOAb, TGAb, and TSHRAb was 22.6%, 22.6%, and 0% in patients with T1DM, respectively. In their siblings, the rates of TPOAb, TGAb and TSHRAb positivity were 7.5%, 10.0%, and 2.5%, respectively. Only one control subject showed TGAb positivity and others were all negative for thyroid autoantibodies. TPOAb and TGAb were found to be significantly different among the groups (p=0.002 and 0.026, respectively), also TA was significantly different among the groups (p=0.004). Our data showed a higher prevalence of thyroid autoantibodies in the sibling groups (15%) than that of the control subjects (2.5%), but the difference was not found to be significant (p=0.108). We examined both FT4 and TSH levels as well as clinical characteristics. AIT was detected in 2 of 31 probands (6.5%). One of 40 siblings (2.5%) showed clinical and biochemical evidence of hyperthyroidism and was treated with methimazole.
Siblings of the TA-positive probands revealed a greater prevalence of thyroid antibodies than did the controls (p=0.022), but siblings of the TA-negative probands did not have such an difference compared with the control subjects (Table 3).
Most cases of T1DM are autoimmune diseases and the majority of T1DM patients have immunological, self-reactive autoantibodies.13 Holmberg et al.14 had found IAA and GADA positivity in 55.2% and 76.0% of Swedish subjects and in 39.6% and 59.4% of Lithuanian patients with T1DM, respectively. Positivity of pancreatic autoantibodies in T1DM patients in Japan are 60–70% for GADA, 45–50% for IAA, and 60–65% for IA-2 antibodies at the time of diagnosis.15 Our results indicated that GADA, IAA and ICA were positive in 80.6%, 35.5% and 6.5% of Korean patients with T1DM.
Many studies have shown that siblings of patients with T1DM are at an increased risk of diabetes-related autoimmunity. 1112 Knip et al.16 reported that pancreas autoantibodies were positive in 24.1% of siblings of T1DM subjects. Onengut-Gumuscu et al.17 revealed that the pancreas autoantibodies were showed in 9% of first-degree relatives of T1DM patients in European countries. Our study revealed that only 1 of 40 (2.5%) siblings had GADA positivity and two subjects (5%) in the control groups had GADA positivity. So, pancreatic autoantibody positivity was very low in siblings of T1DM patients. This is due partly to the lowest incidence rates of T1DM in the Korean population.
T1DM is well known to be associated with other autoimmune diseases and autoantibodies due to similar pathophysiologic mechanisms.18192021 The most common autoimmune disorder related with T1DM is AIT. The autoimmune damage of thyroid gland may occur in either hypothyroid or hyperthyroid conditions.18 The incidence of thyroid disorders may increase with the positivity of thyroid antibodies. TGAb and/or TPOAb show a longtime before the onset of dysfunction of the thyroid gland.51021 Therefore, the detection of these antibodies could be helpful in the diagnosis in the early stages of the disease before thyroid dysfunction develops. In German and Austrian populations, Kordonouri et al.822 revealed a prevalence of 21% TA, but a prevalence of 50% has been shown in T1DM Caucasians.9 These studies of TA positivity in the Asian population with T1DM showed rates of 21.8% in Taiwanese patient and 18% in Japanese patients.2324 In our study, TGAb and TPOAb were positive in 22.6% and 22.6 % of Korean children and adolescents with T1DM, respectively. The overall positivity of TA was 29.0% in Korean patients with T1DM. It was similar to the reports in other studies. AIT was detected in 2 of 31 probands (6.5%). One patient suffered from hypothyroidism and another was hyperthyroidism. Both were treated with medication.
Karagüzel et al.18 reported that the positive rates of TPOAb, TGAb, and TSHRAb were 13.5%, 2.2% and 13.5% in siblings of Turkish T1DM probands. Hanukoglu et al.11 reported that the TA was 25% for first-degree relatives. In this study, the positivity of TGAb, TPOAb and TSHRAb in siblings of probands was 7.5%, 10.0%, and 2.5%, respectively. Of the healthy controls, one subject showed TGAb positivity and others were all negative for thyroid autoantibodies. Our data showed a higher prevalence of thyroid autoantibodies in sibling groups (15%) than in the control subjects (2.5%), but the difference was not statistically significant (p=0.108).
Siblings of TA-positive probands were found to have a significantly increased prevalence of thyroid antibodies than did the controls (p=0.022), but siblings of TA-negative probands did not show much of a differnce compared with the control subjects (Table 3). This result showed the significant positivity of TA in siblings of TA-positive probands. One sibling of a TA-positive proband also revealed Graves' disease and treated with methimazole.
The present study reports on the prevalence of pancreatic and thyroid autoantibodies in Korean children and adolescents with T1DM, their siblings, and healthy control subjects. This study did have some limitations, most notably the small number of enrolled subjects and the inability to include all first-degree relatives except siblings. Nevertheless, beyond these limitations, this study was the first regarding the prevalence of TA and pancreatic autoantibodies in Korean children and adolescents with T1DM, their siblings, and healthy control subjects. It is important that 6.5% of our T1DM subjects already had AIT and one sibling showed Graves' disease. All of them were treated with medication.
In conclusion, the prevalence of pancreatic and thyroid antibody positivity in probands was statistically significant compared with the sibling and control groups. TA was found to have an increased risk in siblings of T1DM patients in contrast with the healthy control subjects. Furthermore, siblings of TA-positive probands revealed a statistically significant prevalence of thyroid antibodies compared to control subjects. So the screening for TA in siblings, particularly siblings of TA-positive probands, was as important as in probands.
Figures and Tables
TABLE 1
Clinical features in patients with type 1 diabetes mellitus, their siblings and control subjects

ACKNOWLEDGEMENTS
This study was financially supported by Dong-A Pharm. Co., Ltd. Grant (IRB No. CNUH-2011-058).
References
2. Ziegler AG, Nepom GT. Prediction and pathogenesis in type 1 diabetes. Immunity. 2010; 32:468–478.

3. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014; 37:Suppl 1. S81–S90.
4. Perros P, McCrimmon RJ, Shaw G, Frier BM. Frequency of thyroid dysfunction in diabetic patients: value of annual screening. Diabet Med. 1995; 12:622–627.

5. Umpierrez GE, Latif KA, Murphy MB, Lambeth HC, Stentz F, Bush A, et al. Thyroid dysfunction in patients with type 1 diabetes: a longitudinal study. Diabetes Care. 2003; 26:1181–1185.
6. Barker JM, Yu J, Yu L, Wang J, Miao D, Bao F, et al. Autoantibody "subspecificity" in type 1 diabetes: risk for organ-specific autoimmunity clusters in distinct groups. Diabetes Care. 2005; 28:850–855.
7. Barker JM. Clinical review: type 1 diabetes-associated autoimmunity: natural history, genetic associations, and screening. J Clin Endocrinol Metab. 2006; 91:1210–1217.

8. Kordonouri O, Klinghammer A, Lang EB, Grüters-Kieslich A, Grabert M, Holl RW. Thyroid autoimmunity in children and adolescents with type 1 diabetes: a multicenter survey. Diabetes Care. 2002; 25:1346–1350.
9. Burek CL, Rose NR, Guire KE, Hoffman WH. Thyroid autoantibodies in black and in white children and adolescents with type 1 diabetes mellitus and their first degree relatives. Autoimmunity. 1990; 7:157–167.

10. Mantovani RM, Mantovani LM, Dias VM. Thyroid autoimmunity in children and adolescents with type 1 diabetes mellitus: prevalence and risk factors. J Pediatr Endocrinol Metab. 2007; 20:669–675.

11. Hanukoglu A, Mizrachi A, Dalal I, Admoni O, Rakover Y, Bistritzer Z, et al. Extrapancreatic autoimmune manifestations in type 1 diabetes patients and their first-degree relatives: a multicenter study. Diabetes Care. 2003; 26:1235–1240.

12. Williams AJ, Norcross AJ, Lock RJ, Unsworth DJ, Gale EA, Bingley PJ. The high prevalence of autoantibodies to tissue transglutaminase in first-degree relatives of patients with type 1 diabetes is not associated with islet autoimmunity. Diabetes Care. 2001; 24:504–509.

13. Gianani R, Campbell-Thompson M, Sarkar SA, Wasserfall C, Pugliese A, Solis JM, et al. Dimorphic histopathology of long-standing childhood-onset diabetes. Diabetologia. 2010; 53:690–698.

14. Holmberg H, Vaarala O, Sadauskaite-Kuehne V, Ilonen J, Padaiga Z, Ludvigsson J. Higher prevalence of autoantibodies to insulin and GAD65 in Swedish compared to Lithuanian children with type 1 diabetes. Diabetes Res Clin Pract. 2006; 72:308–314.

15. Kawasaki E, Eguchi K. Is type 1 diabetes in the Japanese population the same as among Caucasians? Ann N Y Acad Sci. 2004; 1037:96–103.

16. Knip M, Vähäsalo P, Karjalainen J, Lounamaa R, Akerblom HK. Natural history of preclinical IDDM in high risk siblings. Childhood Diabetes in Finland Study Group. Diabetologia. 1994; 37:388–393.
17. Onengut-Gumuscu S, Concannon P. Mapping genes for autoimmunity in humans: type 1 diabetes as a model. Immunol Rev. 2002; 190:182–194.
18. Karagüzel G, Simşek S, Değer O, Okten A. Screening of diabetes, thyroid, and celiac diseases-related autoantibodies in a sample of Turkish children with type 1 diabetes and their siblings. Diabetes Res Clin Pract. 2008; 80:238–243.

19. Sabbah E, Savola K, Ebeling T, Kulmala P, Vähäsalo P, Ilonen J, et al. Genetic, autoimmune, and clinical characteristics of childhood-and adult-onset type 1 diabetes. Diabetes Care. 2000; 23:1326–1332.

20. Levin L, Tomer Y. The etiology of autoimmune diabetes and thyroiditis: evidence for common genetic susceptibility. Autoimmun Rev. 2003; 2:377–386.

21. Unnikrishnan AG, Kumaravel V, Nair V, Rao A, Jayakumar RV, Kumar H, et al. TSH receptor antibodies in subjects with type 1 diabetes mellitus. Ann N Y Acad Sci. 2006; 1079:220–225.

22. Kordonouri O, Charpentier N, Hartmann R. GADA positivity at onset of type 1 diabetes is a risk factor for the development of autoimmune thyroiditis. Pediatr Diabetes. 2011; 12:31–33.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download