INTRODUCTION
Despite the fact that the relative burden of Chronic Obstructive Pulmonary Disease (COPD) in women is high in both the developing and developed countries, the occurrence of COPD in women is not widely appreciated. The historical perception that COPD is principally a disease occurring in men has been challenged by the fact that, COPD-related events including the prevalence, mortality and number of emergency hospital admissions have been swiftly increasing among women over the past two decades.12 The recent data suggests that COPD causes more than 3 million deaths every year, making it the 4th leading cause of death in the world.3 It has been estimated that by the year 2030, COPD will become the third major cause of death. In the South East Asian region, as per the World Health Organization estimations, COPD is responsible for more deaths than that of people with HIV-AIDS, Malaria and Tuberculosis all put together. The more disturbing fact that needs to be addressed, is that the death rates due to COPD are expected to surge by over 160% in the next two decades.4
Half a million people die every year due to COPD in India, which is over four times the number of people who die due to COPD in the USA and Europe.5 This area also represents a large population of women. There is a wide discrepancy in the prevalence of COPD across different studies, ranging 1.2%-19% in women in our country.6 These studies have used respiratory health questionnaires, which have not been validated for the diagnosis of COPD. It is worth mentioning that all studies conducted thus far did not use a spirometer as diagnostic tool, and therefore, the prevalence of COPD in Indian women has been grossly underestimated. Since the prevalence of smoking in Indian women is negligible, health care providers are more likely to misdiagnose them as showing bronchial asthma or attribute their symptoms to cardiac diseases and/or age related issues. This accounts for the significant delays found in the diagnosis of COPD in women.
Tobacco smoking is the most common and best-known cause of COPD, but it is not the only cause. Increasing evidence suggests that a significant number of subjects with COPD have never smoked. The wealth of knowledge available from various studies suggest that 30% of COPD patients have never smoked and that 80% of these non-smokers are women. There is limited knowledge of the risk factors associated with spirometrically confirmed COPD in non-smokers in the general population as well as in women.7 It has been demonstrated that the exposure to high levels of indoor air pollution due to the burning of biomass fuels such as animal dung, crop residues, or wood substantially enhances the risk of COPD relative to smoking tobacco.7
In India, around 60-70 % of the population resides in rural areas. This huge population mostly depends on solid fuels for cooking energy needs. About 80% of rural homes in India still continue to use biomass fuel as their primary cooking and heating energy source. This resource is available almost cost-free. Another factor that describes its high usage rate among these residents is its easy availability. Almost all the kitchens in these dwellings are unventilated without any modern protective amenities. In Indian rural settings, early diagnosis of COPD in women is a daunting task. As women in the early stages of COPD are relatively less symptomatic, they tend to ignore and do not bring it to the notice of healthcare provider. Nevertheless, even if they do complain, measurements of airflow limitation by spirometer that is essential for the diagnosis are often not accessible.8910 Early detection of airflow limitation is crucial as many women, by the time they have been diagnosed as COPD, would be suffering from advanced symptoms of the disease. Hence we undertook this study to find the true prevalence of COPD in women exposed to biomass fuel using sa pirometer in both rural and urban dwellings. The study also aimed to examine the determinants of under-diagnosis of COPD in these participants.
MATERIALS AND METHODS
This is a cross sectional study conducted at a tertiary care hospital with 3 rural and 3 urban health centers attached to it under a Govt. of India's Public-Private partnership that ranged between November 2013 and November 2014. Women aged 40 years and above with a history of exposure to biomass fuel for more than 10 years were enrolled in the study after obtaining informed consent. Biomass fuel exposure was defined as a lifetime exposure of 10 or more years from the use of indoor fire using (1) coal or coke; (2) wood, crop residues or dung as the primary means of cooking or heating. Subjects with Cardiac illness, active or past history of pulmonary Tuberculosis, HIV infections, chest wall deformities, other chronic pulmonary diseases like ILD, Bronchiectasis, Bronchial asthma etc and both current and ex smokers were excluded from the study. Also patients with abnormalities on routine chest radiograph were excluded from the study. Ethical clearance was obtained from University ethical committee for clinical trials.
1. Procedure
All women attending six health centers and tertiary care hospital were first screened for the inclusion criteria. Women who met the criteria of 10 or more years of exposure to biomass fuel as defined above were enrolled in the study. This information was obtained by inquiring about what type of kitchen they had. Then they were asked what was the source of energy and type of stove they used for cooking and heating. Detailed inquiry for causes of delayed diagnosis including the availability of spirometry were done and recorded. Previous prescriptions and investigations along with treating doctor's advice was noted. A thorough assessment of chest radiographs and medications used by the women currently or previously was carried out. Baseline data was documented which included level of education, socioeconomic status, age, years of exposure to biomass fuel, year at which the exposure started, BMI and respiratory symptoms. Furthermore, details of previous admissions and exacerbations were also recorded. Dyspnoea was assessed using the modified Medical Research Council dyspnoea scale (MMRC). The body mass index (BMI) was calculated as the weight in kg divided by height in m2. Then these subjects underwent screening for COPD.
2. COPD diagnosis, staging and BODE index
COPD definition derived from the Global Initiative for Chronic Obstructive Lung Disease (GOLD) based on Postbronchodilator FEV1/FVC<0.70 was applied.11 Pre and postbronchodilation spirometry measurements were performed in all study subjects and forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and FEV1/FVC ratio were recorded. Postbronchodilator values (30 minutes after the administration of 400 µg salbutamol with a spacer) were used for the evaluation of COPD severity, according to GOLD guidelines. The BODE index consisting of: BMI (B); airflow obstruction (O), as measured by the post-bronchodilator FEV1% pred; dyspnoea (D), assessed by the MMRC score; and exercise tolerance (E) measured by 6MWD. The variables were graded from 0-3 and added to provide a total score ranging 0-10 as per previously published works.12 The St George's Respiratory Questionnaire (SGRQ) was used to determine health related quality of life (HRQoL) in all participants.13
Characteristics of the participants in the screening were tabulated against the COPD status defined as "women with no COPD", "women with new COPD" and "women with known COPD". Patients with the label "women with no COPD" did not have a previous diagnosis of COPD and had no COPD according to the panel. Patients with new COPD had no prior diagnosis of COPD, but received such a diagnosis by the panel. The group "women with known COPD" was composed of patients known to have COPD that was confirmed by the panel. The panel included a Pulmonologist, General physician and a cardiologist who assessed the patients for the presence of COPD. All the published ATS/ERS recommendations for the diagnosis of COPD using spirometry were followed meticulously.141516
3. Statistical analysis
Mean values (±SDs) were calculated for normally distributed numerical outcomes. Mean values (±SD) for demo-graphic characteristics among all the groups were analyzed using the Mann Whitney test. The chi-square test was used to compare non-numerical variables. Logistic regression analysis was used for multivariable analysis of the duration of exposure and the age at which the exposure began. The significance level was kept at a p value≤0.05. The analysis was done after adjustment for confounding variables like age, nutritional status (BMI), and socioeconomic status with level of education.
RESULTS
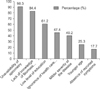
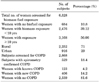
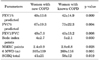
Of 6,328 women screened for biomass fuel exposure, 3,168 women have met the criteria of exposure for ≥10 years. About 300 subjects were excluded from the study due to numerous causes. (131-bronchial asthma, 27-pulmonary tuberculosis, 71-serious cardiac illness, 24-bronchiectasis, 17-inability to perform spirometry, 30-did not attend the tertiary care centre for evaluation). Finally, 2,868 women were screened for COPD using spirometry. A total of 529 (18.4%) women were confirmed to have COPD in which 123 (4.2%) were "women with known" COPD and 406 (14.2%) "women with new COPD" . Other details of the screening are represented in Table 1. Participants with known COPD had prolonged exposure to biomass fuel compared to newly diagnosed subjects. They also experienced significant delays in diagnosis. Similarly, they had statistically significantly more severe diseases, exercise limitations, and high symptom scores as compared to newly diagnosed COPD women. More detailed information on demographics, exposure status, respiratory symptoms, and pulmonary function details are presented in Tables 2, 3. Multivariable logistic regression analysis demonstrated a strong association between the duration of exposure and the development of COPD with an OR 1.2, 95% CI (1.1-1.9) for patients with between 10-15 years of exposure and an OR 2.9, 95% CI (2.5-3.1) for exposure >25 years, p<0.001. There was also significant negative relationship between the age at which exposure started and the risk of COPD (Table 4). Among these participants with COPD, the unavailability of spirometry, low levels of education and lack knowledge of the hazards of biomass fuel in women were the important predictors in the under-diagnosis or delayed diagnosis of COPD (Fig. 1).
DISCUSSION
The present study has four novel findings. First, the prevalence of COPD among women exposed to biomass fuel was very high. Second, there was a significant delay in the diagnosis, which led to advanced disease by the time they were identified as cases of COPD. Third, the duration of exposure and the age at which the exposure to biomass fuel begins, has great influence on the development of COPD. Fourth, the absence of tobacco smoking, unavailability of spirometry, low level of education, ignorance of health care providers and the lack knowledge of hazards of biomass fuel in women were the important predictors of under-diagnosis or delayed diagnosis of COPD in female patients.
Internationally, nearly 50% of COPD deaths in developing countries could be due to biomass, with -75% of these occurring in women. Biomass fuels produce tremendously high levels of indoor air pollution. 24-hour levels of PM10 (particles with a 50% cut-off aerodynamic diameter of <10 µm) in biomass-using homes range between 300-3000 µg·m−3 in Latin America.17 It may peak as high as 10 000 µg·m−3 during cooking.18 This is in contrast to the standard annual mean PM10 levels in outdoor air, which were set at 50 µg·m−3 by various agencies.19 Around 70-80%% of the homes, in India use biomass fuel for cooking and these kitchens are poorly ventilated. A woman who spends between 2-3 hours for cooking every day inhales a volume of 25 million litres of highly polluted air in her life time, thereby exposing her to extremely high levels of particulate matter and gaseous air pollutants.8
In the current study, the prevalence of COPD among women exposed to biomass fuel was 18.4%, which is in agreement with the results of a meta-analysis by Hu et al of six Asian and nine non-Asian published studies from Mexico, Columbia, Brazil, Bolivia, Spain, Saudi Arabia, Turkey, Pakistan, India, Nepal, and China. Exposure to biomass fuel smoke was found to be associated with a 2.3-fold increased odds of COPD compared with no exposure to biomass smoke. They also demonstrated that overall, people exposed to biomass smoke have an OR of 2.44 (95% CI, 1.9-3.33) for developing COPD, relative to those not exposed to biomass smoke, which is similar to the findings of our current analysis.19 Our study is comparable to another case control study by Ekici and colleagues of 596 women who have never smoked in Turkey, which reported the prevalence of COPD due to biomass smoke to be 23% after adjustment for confounding factors.20 It should be noted that, even developed countries such as the USA have a substantial burden of COPD due to exposure to biomass smoke. A study by Sood and colleagues, reported that exposure to wood smoke was associated with a 70% (95% CI 30-220) increased risk of having COPD in both men and women and that this association remained even after adjustment for age, tobacco smoking, and educational attainment, in adults living in New Mexico, USA.21
In addition to this, we also established that there was significant delay in diagnosis of COPD in these women. In the present study, "women with known COPD" had mean age at diagnosis of COPD was 61±5.2 years as compared to 47±3.6 years in "women with new COPD". Therefore the disease had advanced quite far with a substantial influence on the HRQoL. It is worth mentioning that BODE index points, MMRC points and SGRQ scores were statistically high in "women with known COPD" suggesting late diagnosis and progressive impairment of pulmonary functions with uninterrupted exposure.
Another remarkable observation in the present analysis was that the risk of COPD significantly and statistically increases with early exposure to biomass fuel. We have confirmed that women who were exposed to biomass fuel at the younger age of 5-9 years had higher odds of developing COPD than those who were exposed at the age 20 years (OR2.9, CI 95% [2.2-3.1] vs OR1.3 .95%CI [0.9-1.6]). As girls in India spend more time with their mothers and help them with domestic work at a very early age, they are more vulnerable to developing respiratory symptoms because they have been exposed to biofuels for >40-50 years.22 This chronic insult, beginning in childhood, may act as an early stimulus for airway damage and impaired pulmonary functions. Our study highlights observations of some studies that suggest increased lower respiratory tract infection during childhood due to exposure to biofuels is a risk factor for developing chronic airway obstruction in adulthood.23
Our results indicate that COPD underdiagnosis was frequent in women in the study cohorts. Determinants of COPD under-diagnosis in our study cohorts were younger, never having smoked, had a lower level of education, an absence of reported symptoms, an unavailability of spirometry, a lack of knowledge of hazards of biomass fuel and a milder severity of airflow limitation. In India, smoking among women is socially unacceptable and hence the prevalence of smoking is negligible. Women do not seek medical attention until they have significant symptoms. Furthermore, the age-old perception that COPD is principally a disease of men who smoke tobacco still remains embeded in the minds of the health care providers. Spirometry, which is the gold standard diagnostic test, remains poorly utilized in clinical practice. Clinicians are not aware that relying on history and clinical examinations only to diagnose COPD under-estimates the disease in over 50% of cases.24 Clinicians need to accept the fact that spirometry is the most important diagnostic test for COPD.
Women should be made aware of the consequences of biomass fuel both by clinicians and environmental experts to a larger extent. Women should be educated about use of "clean" fuel (e.g., liquid propane gas or natural gas) or electricity. However, this may not be appropriate or affordable in the Indian circumstance. Other interventions such as outdoor relocation of cooking using biomass fuel, addition of windows to the kitchen and using improved cook stoves with better ventilation systems such as a chimney can be implemented. Stoves with higher heat transfer ratios and complete combustion capacities should be recommended. 25 These preventive measures with early diagnosis of COPD in these subjects which could lead to improvement in the quality of life, reduce their symptoms, prevent exacerbations and hospitalizations and even improve survival.
This study has a number of postive points. To our knowledge, it is the first and largest assessment of COPD in women exposed to biomass fuel in India using spirometry, unlike many questionnaire-based evaluations. Both spirometry and bronchodilator testing were conducted with similar standard protocols, which was likely to reduce bias due to methodological issues. Availability of thorough exposure details of all subjects made it possible to demonstrate a clear relationship between biomass fuel and COPD risk in a larger number of subjects representing both rural and urban houses. Some limitations must be noted. Mainly, it is single center study and women who were current or ex-smokers remained excluded from the study even though some of these smokers had concomitant exposure to biomass fuel as well. Various comorbidities associated with these women with COPD were not taken into account. However, this will not affect the outcome of the study, as the primary objective of the trial was to assess the impact of biomass fuel on COPD diagnosis in non-tobacco smoking women.
CONCLUSION
The prevalence of COPD among women exposed to biomass fuel is very high. There is strong correlation between the risk of COPD and duration of exposure along with the age at which the exposure to biomass fuel begins. Under-diagnosis of COPD was frequent in women due to the unavailability of spirometry, a lack knowledge of hazards of biomass fuel, the low level of education of the subjects, and the ignorance of the health care providers being the important determinants of under-diagnosis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download