Abstract
The current study aimed to determine the efficacy of probing with adjunctive mitomycin C (MMC) as a treatment for nasolacrimal duct obstruction (NLDO) in adults and to study the association of probing success with demographic and obstruction characteristics. This was a prospective, randomized, double-blind, placebo-controlled trial including 140 patients (each with a unilateral NLDO) scheduled for nasolacrimal probing who were randomly assigned to receive MMC (0.2 mg/ml, 70 patients; group A) or placebo (normal saline, 70 patients; group B). Irrigation was carried out with 0.5 cc of MMC (0.2 mg/mL) in the duct with a nasal pack for 10 minutes in group A. Patients' postprobing epiphora was evaluated at 2 weeks and 1, 3, 6, and 9 months postoperatively. Probing was judged to be a success if there was no or mild watering for at least 9 months after the procedure. There were no significant differences between the two study groups in demographic characteristics or duration of the operation (p=0.062). The overall success rate of probing with MMC was 47/70 (67.1%), which was significantly higher than the success rate of the procedure with placebo (p=0.0027). When the sex of the patients was controlled for by logistic regression, a significant association between the failure rate of probing and increasing age was found in cases and controls (p=0.004 vs. p=0.006, respectively). No significant side effects of probing with MMC were noted after 9 months of follow-up. Administering MMC in a dosage of 0.2 mg/mL during nasolacrimal probing significantly increased the success rate of probing. The failure rate of probing increased with age. A low dose of MMC is cheap, safe, and easily accessible; thus, it is recommended during nasolacrimal probing, especially in patients who refuse dacryocystorhinostomy surgery.
Nasolacrimal duct obstruction (NLDO) is a common disorder in adults that can lead to intermittent or constant tearing (epiphora), watery eye with blurred vision, and chronic or acute dacryocystitis.1 It is thought that inflammation and cellular debris with congenital, cicatricial, infectious, traumatic, idiopathic, neoplastic, involutional, or iatrogenic factors can lead to occlusive fibrosis in the nasolacrimal duct.2,3,4
There are different surgical methods for NLDO treatment. Although dacryocystorhinostomy is a common treatment for NLDO, it is an invasive and bothersome procedure for patients. Probing was a common method until the 1920s and nowadays is a quick, cost-effective, simple, and safe alternative with fewer complications than surgery. However, the major problem with probing is recurrent obstruction from further fibrosis and induced trauma.5,6
Some topical ocular medications may inhibit fibroblast proliferation and are thus thought to be useful after NLDO surgical treatment. Mitomycin C (MMC) is a chemotherapeutic antibiotic that has been used as an adjunct to prevent recurrence after pterygium surgery and glaucoma surgery.7 Several studies have reported that topical MMC is effective in squamous cell carcinoma treatment,8 conjunctival corneal intraepithelial neoplasia,9 primary acquired melanosis,10 and conjunctival melanoma treatment.11 Few studies have investigated the utility of MMC for lacrimal probing to treat NLDO. Although a preliminary study12 showed that MMC, as an adjuvant for nasolacrimal duct probing, can improve subjective and objective outcomes, that study was done on only 32 patients and included no control group for comparison. In this case, a comparative study with an adequately large sample size would have been needed to conclusively determine the effect of MMC as an adjunct for a nasolacrimal probing procedure.
Given this background, we performed the present study to confirm the effect of using a low dose of MMC as an adjunct for nasolacrimal duct probing to treat adults with primary and complete NLDO. We also aimed to determine the association of probing success with demographic and obstruction characteristics.
The present study was a prospective, randomized, double-blind, placebo-controlled trial performed in Peymanie and Motahari Hospitals, which are tertiary health care centers affiliated with Jahrom University of Medical Sciences, during April 2008 and December 2010. One hundred seventy consecutive adult patients with unilateral NLDO who suffered from epiphora were referred to our center. A total of 140 patients aged 18 or older were enrolled in the study, as shown in Fig. 1. The study protocol was based on the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of the Jahrom University of Medical Sciences. We obtained the approval of the Ethics Committee of the hospitals before the study, and all participants gave their written informed consent. One hundred forty adult patients scheduled for nasolacrimal duct probing under local anesthesia were enrolled. Before the surgical procedure, all patients underwent a complete ophthalmologic examination. The diagnosis of NLDO was confirmed through the patient's ophthalmic history, including the symptoms of discharge, epiphora, and chronic dacryocystitis. Diagnosis was also made by use of slit-lamp examination to rule out disorders of the ocular surface and by eyelid examination for possible laxity or misdirected lashes and proper closure. When needed, the tear break-up time, Schirmer I and II tests, Jones I test, or a fluorescein staining and dye-disappearance test were performed. Lacrimal irrigation with saline solution showed the location of the obstruction. We excluded patients with a previous history of surgical intervention, diabetes mellitus, eye trauma, nasal structural abnormalities, lacrimal system tumors, severe atrophic rhinitis, and acute or recurrent dacryocystitis. We also excluded those with epiphora due to wind or cold, nasal cavity pathologies, eyelid deformities, congenital epiphora, or lacrimal pump dysfunction.
One day before the operation, the patients were referred to centers for preoperative evaluation. They were registered to participate in the study in the order of referral by a nurse who was blinded to the study. Each patient selected a sealed envelope containing a number. The envelope was opened by an assistant who was also blinded to the study groups. Randomization was done by use of a computer-based random digit generator. According to the random number table, the sealed white and black boxes containing MMC and placebo, respectively, were received by each patient. Thus, the participants were randomly allocated to receive either MMC (Advacare, US) in a dosage of 0.2 mg/mL (70 patients; group A) or matched placebo (normal saline; 70 patients; group B) during the surgery.
All patients were visited to be informed about the study protocol and for pre-anesthetic assessment the day before the surgery. A surgeon who was blinded to the study protocol operated on all patients and the same anesthetic protocol was used for all patients. For all patients, the procedure was carried out under topical anesthesia induced with 0.5% tetracaine and adrenaline with lidocaine 2% for local infiltration (nasociliary, infratrochlear, and infraorbital blocks). Probing was carried out through the upper canaliculum with a Bowman 0- and 00- probe. The probe was pushed through by use of gentle pressure and was advanced to the point of obstruction. To stop possible bleeding, the probe was held in the nasal cavity for 1 minute. Patency after probing was confirmed by syringing. In group A, irrigation was carried out by 0.5 cc of MMC (0.2 mg/mL) into the duct with a nasal pack for 10 minutes. We asked the patients not to swallow the solution, and water for gargling was provided to clear any residual MMC. Then the ocular surface was irrigated with normal saline. In group B, irrigation was carried out by use of normal saline only. Patients were treated with antibiotic ointment and topical steroid (chloramphenicol) four times daily for a period of 7 to 14 days. If patency was lost, the procedure was repeated 2 months after the first treatment.
The patients were followed up at 2 weeks and 1, 3, 6, and 9 months after the procedure. During every checkup, patency was confirmed by irrigation, and the patients were questioned concerning whether they had been free of watering for the purpose of subjective evaluation of improvement. Slit-lamp examination of the caruncle, punctum, cornea, conjunctiva, iris, lens, and anterior chamber and nasal mucosa examination was done to look for side effects. The following four groups were used for patients' post-probing epiphora: no watering, watering outdoors (mild watering) only, indoors (moderate watering) watering, and severe watering. If there had been no or mild watering for at least 9 months following the procedure, probing was judged to be a success. All data were recorded by a blinded evaluator.
Fifty patients were required for each study group to have a power of 0.9 to find any significant differences regarding patency after the operation (p=0.05, 2-sided). Finally, we enrolled 70 patients in each group to compensate for any refusal as a result of possible nonevaluable data. The Statistical Package for the Social Sciences (SPSS) for Windows, version 14 (SPSS Inc., Chicago, IL), was used for data analysis. Quantitative variables such as age, height, weight, body mass index (BMI), and duration of operation were analyzed between the two groups by using an independent sample t-test. McNemar's sample test was used to compare the patency of NLDO within the groups at different time points. The chi-square sample test was used to compare proportions between groups. Various types of subjective improvement in epiphora after probing were analyzed between the two groups by using Friedman's test. A logistic regression model was used to determine which demographic variables (age and sex) and other variables (proximal, distal, right, and left side of NLDO) had significant effects on the success rate of probing. Data are reported as mean±standard deviation, frequency and percentage (%), and odds ratio (OR) and 95% confidence interval. A 2-sided p value<0.05 was considered statistically significant.
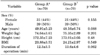
Of the 140 patients who were enrolled in the study, none were lost to follow-up; thus, the number of patients who finished the study was 140. There were no demographic differences (age, gender distribution, height, weight, BMI, and duration of the operation) between the two study groups (Table 1). Obstruction was seen on the proximal side of the nasolacrimal duct in 71 patients, on the distal side in 69 patients, on the left side in 68 patients, and on the right side in 72 patients.
Of the 140 patients after 9 months of follow-up, 22 eyes (15.7%) had an outcome of no watering, 43 (30.7%) had mild watering, 15 (10.7%) had moderate watering, and 60 (42.9 %) still suffered from severe watering after probing. There were significant differences between the two study groups in patient's post-probing epiphora grades during 9 months of follow-up (Fig. 2). There were statistically significant differences between the two study groups in patency rates at any follow-up (Fig. 3), with 21 eyes (30%) of cases and 5 eyes (7.1%) of controls remaining complete free of obstruction, whereas 26 eyes (37.1%) of cases and 13 eyes (18.5%) of controls remained slightly free of obstruction at 9 months. The overall success rate of probing with MMC was 47/70 (67.1%), which was significantly higher than the procedure with placebo (p=0.0027). Four patients suffered from a little bloody discharge after probing from the punctum; however, they were treated with phenylephrine drops. No significant side effects of probing with MMC were noted after 9 months of follow-up.
Analysis of the success rate of probing in different sexes showed no relationship in the two study groups when age was controlled for by logistic regression. A significant association was found between the failure rate of probing and increasing age in the two study groups when sex was controlled by logistic regression (Table 2). No significant association between the side of obstruction (proximal, distal, right, and left) and the success rate of probing was found (Table 3).
The findings in this prospective randomized clinical trial confirmed the efficacy of MMC in decreasing the symptom of epiphora after probing in NLDO. Our results demonstrated that the overall success rates of probing at the end of the study were 67.1% and 47.1% in the cases and controls, respectively. We also noticed that the patency rate was significantly better in patients treated with MMC during probing than in those treated with normal saline for the whole study period. Although the rate of moderate watering was not significantly different between the two study groups during the 9 months of follow-up, this rate was lower in cases than in controls. According to the results of this study, the failure rate of probing increased with age. In addition, this study indicated no significant side effects of probing with MMC after 9 months of follow-up.
MMC is a chemotherapeutic antibiotic isolated from Streptomyces caespitosus. Its mode of action is to mimic the effects of ionizing radiation. MMC inhibits DNA synthesis in all phases of the cell cycle because of cross-linkage between the DNA base pairs adenine and guanine. MMC also induces breakage of single-stranded DNA. Despite its non-cell cycle-specific action, rapidly dividing cells are rather sensitive to these effects.7,8,9 Moreover, MMC prevents fibroblast proliferation and modifies the wound healing response, leading to less scarring and fibrosis around the common osteotomy and canaliculus site.10,11
Here, the success rates of probing with MMC were 82.8% after 2 weeks of follow-up, 71.4% after 1 month of follow-up, 68.5% after 3 and 6 months of follow-up, and 67.1% after 9 months of follow-up. Of the 70 patients after 9 months of follow-up, 25.7% had no watering, 41.4% had mild watering, 8.5% had moderate watering, and 24.2% had severe watering. In a similar study, Tsai et al.12 reported full absence of watering in 25%, moderate improvement in 47%, mild improvement in 11%, and no improvement in 17% of patients with NLDO who were treated by probing with MMC after 9 months of follow-up. Tsai et al. performed a noncomparative study, in which no control group of probing with saline was included. In that study, the overall patency rate after probing with MMC was 89%. Likewise, the overall improvement after probing with MMC in a study from Sinha et al.13 was 65% and the patency rate was 30% after 3 months of follow-up. Their findings are similar to ours in that probing with MMC was significantly better than probing with saline after 1 month of follow-up. Nevertheless, they did not show a significant difference in the patency rate between their two study groups after 3 months of follow-up. In addition, there were some concerns in their study that undermine the ability to make a definite conclusion from the reported results.14 However, we showed that the patency rate of probing with MMC was significantly better than probing with normal saline throughout the study period. A similar study by Choontanom15 showed that a dose of 0.2 mg/mL MMC significantly reduced the epiphora symptom after probing in NLDO compared with that in patients in the normal saline solution group. In contrast to these studies, Razeghinezhad et al.16 reported no, mild, moderate, and severe watering in 23.6%, 11.7%, 17.7%, and 47% of eyes, respectively, when probing with MMC was used. We achieved the same findings as Tabatabaii et al.17 regarding the efficacy of probing with MMC for NLDO. They performed a noncomparative study with 6 months of follow-up. Nasolacrimal probing is a less-invasive procedure for healing NLDO in adults compared with dacryocystorhinostomy. Using a 0.2-mg/mL dose of adjunctive MMC is suggested to achieve long-term patency of the nasolacrimal duct and to prevent toxic effects such as glaucoma, iritis, keratitis, late-onset corneal necrosis, and scleral necrosis after probing.18
Also, the results showed that the success rate of probing with or without MMC significantly reduced with increasing age. Many factors are believed to influence the success rate of probing the nasolacrimal duct: bilaterality, age, prior failed conservative treatments, prior failed probing attempts, dilated sacs, and nonmembranous NLDO. A study from Kashkouli et al.19 indicated a decline in success with increasing age. Although the exact reason for the discrepant effect of age on the success rate of probing is not entirely clear, some hypotheses persist. First, elongated inflammation in the lacrimal drainage system may result in fibrosis, which increases with age.20 Likewise, some suggest that more complex cases may present later, whereas less severe obstructions may unexpectedly clear out. Thus, at the time of probing, the success rate is not influenced by age; rather, it is affected by the high frequency of mixed and severe obstructions in elderly patients.21 As such, our findings mirror those of De Angelis et al.,22 who studied the histopathology of NLDO in adults and reported bony inflammation in 14% and inflammatory changes in 94% of patients. However, additional studies addressing the impact of probing and complex NLDO in elderly patients are required to definitively characterize this association. Although the severity and duration of the disease before treatment may be associated with the outcome, these were not considered in the analysis.
One of the advantages of the present study was the large sample size of our studied population, which indicated significant differences between proportions and variables. Also, we did not dichotomize the data for continuous variables, which additionally impacted the precision of our analysis.
In conclusion, our results confirmed the efficacy of probing with MMC in reducing the symptoms of epiphora with fewer side effects in patients with NLDO during 9 months of follow-up. The overall success rate of nasolacrimal probing with MMC was 67.14% after 9 months, which reduced with increasing age. On the basis of these findings, we contend that nasolacrimal probing with MMC can induce subjective improvement in epiphora with regard to a good success rate for a period of less than 1 year. Moreover, it would be invaluable to conduct studies to investigate the factors that increase fibrosis and inflammation after interventional or surgical procedures. Hence, it is suggested that future studies focus on the success rate of probing in NLDO with MMC in patients with a history of any conditions that increase inflammation and fibrosis, such as diabetes mellitus.
Figures and Tables
FIG. 2
The number of eyes in each grade of epiphora after probing during 9 months of follow-up. Group A: patients who were treated with mitomycin C. Group B: controls.
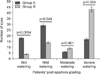
FIG. 3
Success rate of probing according to the number of eyes and duration of follow-up. Group A: patients who were treated with mitomycin C. Group B: controls.
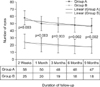
TABLE 1
Demographic and surgery characteristics of the two study groups of patients undergoing probing
ACKNOWLEDGEMENTS
We would like to thank all the patients and their respectful families who participated in the present study. We also acknowledge the authorities of Jahrom University of Medical Sciences for financial support. Also, the authors would like to thank Dr. Nasrin Shokrpour at the Center for Development of Clinical Research of Nemazee Hospital for editorial assistance. The protocol of this trial has been registered and is available publicly at www.irct.ir (identifier number IRCT2013040310241N1).
References
1. Ali MJ. Lacrimal disorders and surgery: historical perspectives. In : Ali MJ, editor. Principles and Practice of Lacrimal Surgery. New Delhi: Springer;2015. p. 1–8.
2. Sobel RK, Carter KD, Allen RC. Bilateral lacrimal drainage obstruction and its association with secondary causes. Ophthal Plast Reconstr Surg. 2014; 30:152–156.

3. Kamal S, Ali MJ. Primary Acquired Nasolacrimal Duct Obstruction (PANDO) and Secondary Acquired Lacrimal Duct Obstructions (SALDO). In : Ali MJ, editor. Principles and Practice of Lacrimal Surgery. New Delhi: Springer;2015. p. 133–141.
4. Nemet AY, Vinker S. Associated morbidity of nasolacrimal duct obstruction--a large community based case-control study. Graefes Arch Clin Exp Ophthalmol. 2014; 252:125–130.

5. Baig R, Khan QA, Ahmad K. Long-term outcome of primary external dacryocystorhinostomy. J Coll Physicians Surg Pak. 2013; 23:641–644.
6. Ekinci M, Çağatay HH, Oba ME, Yazar Z, Kaplan A, Gökçe G, et al. The long-term follow-up results of external dacryocystorhinostomy skin incision scar with W incision. Orbit. 2013; 32:349–355.

7. Kaufman SC, Jacobs DS, Lee WB, Deng SX, Rosenblatt MI, Shtein RM. Options and adjuvants in surgery for pterygium: a report by the American Academy of Ophthalmology. Ophthalmology. 2013; 120:201–208.
8. Kashkouli MB, Heirati A, Pakdel F, Kiavash V, Naseripour M, Aghamohammadi F. Long-term follow-up of invasive ocular surface squamous cell carcinoma treated with excision, cryotherapy, and topical mitomycin C. Graefes Arch Clin Exp Ophthalmol. 2012; [Epub ahead of print].

9. Birkholz ES, Goins KM, Sutphin JE, Kitzmann AS, Wagoner MD. Treatment of ocular surface squamous cell intraepithelial neoplasia with and without mitomycin C. Cornea. 2011; 30:37–41.

10. Lichtinger A, Pe'er J, Frucht-Pery J, Solomon A. Limbal stem cell deficiency after topical mitomycin C therapy for primary acquired melanosis with atypia. Ophthalmology. 2010; 117:431–437.

11. Lim LA, Madigan MC, Conway RM. Conjunctival melanoma: a review of conceptual and treatment advances. Clin Ophthalmol. 2013; 6:521–531.

12. Tsai CC, Kau HC, Kao SC, Hsu WM, Liu JH. Efficacy of probing the nasolacrimal duct with adjunctive Mitomycin-C for epiphora in adults. Ophthalmology. 2002; 109:172–174.

13. Sinha MK, Bajaj MS, Pushker N, Ghose S, Chandra M. Efficacy of probing with mitomycin-C in adults with primary acquired nasolacrimal duct obstruction. J Ocul Pharmacol Ther. 2013; 29:353–355.

14. Ghobadifar MA, Degani N, Dezhkam I, Rezaei N. Probing with mitomycin-C in adults with nasolacrimal duct obstruction. J Ocul Pharmacol Ther. 2013; 29:515.

15. Choontanom R. Probing and syringing with 3% solution of NaCl and/or 0.2 mg/ml mitomycin-C in nasolacrimal duct obstruction patients. J Med Assoc Thai. 2010; 93:Suppl 6. S197–S202.
16. Razeghinezhad MR, Banihashemi SA, Bagheri B. Probing with adjunctive Mitomycin-C In adult patients with nasolacrimal duct obstruction. Med J Hormozgan Univ. 2005; 9:219–220.
17. Tabatabaii SZAD, Sadeghi TA, Kasaei AAF. Efficacy of nasolacrimal duct probing with adjuctive Mitomycin C for adult partial nasolacrimal duct obstruction (Pnldo). Iran J Ophthalmol. 2005; 18:6–10.
18. Rubinfeld RS, Pfister RR, Stein RM, Foster CS, Martin NF, Stoleru S, et al. Serious complications of topical mitomycin-C after pterygium surgery. Ophthalmology. 1992; 99:1647–1654.

19. Kashkouli MB, Beigi B, Parvaresh MM, Kassaee A, Tabatabaee Z. Late and very late initial probing for congenital nasolacrimal duct obstruction: what is the cause of failure? Br J Ophthalmol. 2003; 87:1151–1153.

20. Stager D, Baker JD, Frey T, Weakley DR Jr, Birch EE. Office probing of congenital nasolacrimal duct obstruction. Ophthalmic Surg. 1992; 23:482–484.

21. Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology. 1986; 93:1055–1063.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download