Abstract
An aneurysm of the subclavian artery is rare. Recently, we experienced a case of a ruptured subclavian artery aneurysm presenting as hemoptysis. The patient had experienced atypical chest discomfort, and computed tomography (CT) revealed a small aneurysm of the left subclavian artery (SCA). Hemoptysis occurred 2 weeks later. Follow-up CT showed a ruptured aneurysm at the proximal left SCA. Endovascular treatment with a graft stent was performed by bilateral arterial access with a 12-Fr introducer sheath placed via cutdown of the left axillary artery and an 8-Fr sheath in the right femoral artery. A self-expandable Viabahn covered stent measuring 13×5 mm was introduced retrogradely via the left axillary sheath and was positioned under contrast guidance with an 8-Fr JR4 guide through the femoral sheath. After the procedure, hemoptysis was not found, and the 3-month follow-up CT showed luminal patency of the left proximal SCA and considerable reduction of the hematoma.
A subclavian artery aneurysm (SAA) is a rare peripheral aneurysm.1 Although rare, an SAA can cause life-threatening complications such as rupture, thrombosis, and embolism.2 Recently, we experienced a case of a ruptured SAA presenting as hemoptysis, which was successfully treated by endovascular stenting.
An 83-year-old man was transferred to our hospital complaining of hemoptysis. Two weeks previously, he had visited the local hospital for atypical chest discomfort that had increased over the past 2 weeks. At that time, computed tomography (CT) of the thorax had revealed a small aneurysm of the left proximal subclavian artery (Fig. 1A). He had no history of trauma, infection, or systemic vasculitis. Two weeks later, the patient visited our emergency department owing to hemoptysis. Contrast-enhanced CT showed 7 cm of loculated fluid collection with peripheral wall enhancement in the upper hemithorax and an approximately 2.5-cm irregular contrast filling sac in the proximal portion of the left subclavian artery with scattered vascular calcification (Fig. 1B, Fig. 2). No other aneurysms were noted in the brain, neck, chest, or abdomen CT scans.
Because of the patient's refusal to undergo an operation, endovascular treatment with a graft stent was performed. The procedure is shown in Fig. 3. An angiogram using a pigtail catheter via the right femoral approach was performed to delineate the anatomy and confirm the aneurysmal leakage. Because the diameter of the SAA was very large on the angiogram, the endovascular stent was approached by a bilateral access technique in which the bulky stent graft was introduced retrogradely via cutdown of the left axillary artery and an 8-Fr sheath in the right femoral artery.3 Under local anesthesia, a 12-Fr Magnum catheter was placed via an ipsilateral, retrograde axillary cutdown approach. A stiff guidewire was placed through the 12-Fr catheter. A self-expandable Viabahn covered stent (W.L. Gore and Associates Inc., USA) measuring 13×5 mm was then deployed over the stiff wire in the subclavian artery under fluoroscopic guidance, with particular attention to not cover the orifice of the internal mammary or vertebral artery. Minimal contrast leakage remained in the aneurysm but the flow was very slow. The sheath and the wire were removed, and manual pressure was placed over the axillary artery. The entire procedure was performed successfully and there were no neurological sequels.
After the procedure, no hemoptysis was found and the patient was discharged on the seventh day after the procedure. Three months later, follow-up CT showed luminal patency of the left proximal subclavian artery and considerable reduction of the hematoma (Fig. 4).
This is the first case report of the successful treatment of a ruptured SAA with a covered stent in Korea. Because a large stent cannot be easily introduced into the subclavian artery via a femoral access, we used bilateral arterial access with cutdown of the left axillary artery and right femoral artery. This hybrid approach has rarely been reported worldwide.
SAAs are rare, as seen in a report by Dent et al.1 in which SAAs represented only 0.1% of an extensive series of atherosclerotic aneurysms. The common causes of SAAs were atherosclerosis, thoracic outlet syndrome, infection, trauma, and congenital arterial anomalies such as Marfan syndrome.1,2 In particular, proximal aneurysms were caused by atherosclerosis (19%), collagen disorder (18%), trauma (15%), infection (13%), and in-hospital procedures (12%).2 Our reported case did not have a history of trauma, infection, or vasculitis. Instead, the scattered vascular calcification of the aneurysm suggested that the cause might be atherosclerosis. An atherosclerotic SAA in an intrathoracic location usually occurs in patients over 60 years of age of either sex, but appears to be more common in men.
Although SAAs can be asymptomatic, they can also cause life-threatening complications such as rupture, thrombosis, or embolism and can result in symptoms caused by local compression.2 In a meta-analysis of 394 native SAAs, rupture occurred in 9% of patients, with an associated mortality of 19%.4 Rupture is a rare complication with a high mortality and can produce intra- or extrathoracic bleeding, including hemoptysis from rupture and erosion into the apex of the lungs. Most patients have an episode of hemoptysis, which might be an early sign of rupture.2
The indication for treatment of an SAA is usually based on prevention of complications, such as thrombosis, embolization, and rupture. The development of these complications may depend on variable aneurysm-related characteristics including etiology and localization. Therapeutic options include open surgical repair, endovascular stenting, and conservative management. Since Halsted first successfully combined ligation with resection of an SAA in 1892,5 surgical repair was recommended for all patients with an SAA to prevent potential complications.3 Endovascular stent graft treatment for arterial injuries began appearing in the literature over a decade ago.6,7,8,9 The evolution of endovascular technology has improved the stents available to vascular surgeons and interventionists in the management of SAAs. The subclavian artery is mobile and is exposed to rotational forces during abduction and anteflexion of the arm. Therefore, a flexible stent graft might be a better option in the SAA in particular patients.10 In our case, we successfully applied a self-expandable Viabahn covered stent.
The natural history of SAAs is unknown and there are no guidelines concerning the timing of intervention or treatment modalities. In our case, the severe complication of aneurysmal rupture occurred after 2 weeks despite the small size of the aneurysm and optimal medical therapy. Regardless of the size of the aneurysm, high mortality from rupture has been reported. Thus, early intervention including open surgery or endovascular stenting might be needed to prevent potential complications if patients have symptoms.
Figures and Tables
FIG. 1
(A) Chest computed tomography angiogram (CTA) showed a small aneurysm of the proximal left subclavian artery. (B) Follow-up chest CTA showed 7 cm of loculated fluid collection with peripheral wall enhancement in the upper hemithorax and an irregular contrast filling sac of about 2.5 cm.

FIG. 2
Neck computed tomography angiogram showed an irregular contrast filling sac of 2.5 cm arising from the left proximal subclavian artery with scattered vascular calcifications.
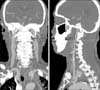
FIG. 3
(A) Angiogram using a pigtail catheter via a right femoral approach was performed to delineate the anatomy and confirmed the aneurysmal leakage. (B) A self-expandable Viabahn covered stent (W.L. Gore and Associates Inc. U.S.A.) measuring 13×5 mm was introduced over the stiff wire in the subclavian artery retrogradely via the left axillary sheath. (C) The stent graft was deployed over the stiff wire in the subclavian artery under fluoroscopic guidance. (D) Minimal contrast leakage remained in the aneurysm but the flow was very slow.

References
1. Dent TL, Lindenauer SM, Ernst CB, Fry WJ. Multiple arteriosclerotic arterial aneurysms. Arch Surg. 1972; 105:338–344.

2. Vierhout BP, Zeebregts CJ, van den Dungen JJ, Reijnen MM. Changing profiles of diagnostic and treatment options in subclavian artery aneurysms. Eur J Vasc Endovasc Surg. 2010; 40:27–34.

3. Chen YF, Su CS, Liu TJ, Chang MS, Jong GP, Ting CT, et al. Endovascular treatment of a nontraumatic left subclavian artery pseudoaneurysm. J Chin Med Assoc. 2012; 75:474–478.

4. Andersen ND, Barfield ME, Hanna JM, Shah AA, Shortell CK, McCann RL, et al. Intrathoracic subclavian artery aneurysm repair in the thoracic endovascular aortic repair era. J Vasc Surg. 2013; 57:915–925.

5. Halsted WS. Ligation of the first portion of the left subclavian artery and excision of a subclavian axillary aneurysm. Bull Johns Hopkins Hosp. 1892; 24:93.
6. Phipp LH, Scott DJ, Kessel D, Robertson I. Subclavian stents and stent-grafts: cause for concern? J Endovasc Surg. 1999; 6:223–226.

7. Sitsen ME, Ho GH, Blankensteijn JD. Deformation of self-expanding stent-grafts complicating endovascular peripheral aneurysm repair. J Endovasc Surg. 1999; 6:288–292.

8. Kasirajan K, Matteson B, Marek JM, Langsfeld M. Covered stents for true subclavian aneurysms in patients with degenerative connective tissue disorders. J Endovasc Ther. 2003; 10:647–652.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download