Abstract
Oral lichen planus (OLP) is a chronic inflammatory mucosal disease of unknown etiology. Many studies have implicated the protective role of antioxidants in such diseases. The aim of this study was to compare salivary total antioxidant capacity (TAC and malondialdehyde (MDA) and antioxidant vitamin (vitamin s A, C and E) levels in patients with erosive OLP and healthy individuals. Thirty six patients with OLP (14 males, 22 females) and 36 control subjects (15 males, 21 females), matched for age and sex were enrolled in this case control study. The salivary levels of MDA, TAC, and antioxidant vitamin levels were measured in both case and control groups. The salivary level of MDA was significantly higher (p<0.001) in patients than in controls. In patients with OLP, the TAC of saliva was significantly lower than that in healthy subjects (p<0.001). Compared with controls, the levels of salivary antioxidant vitamins were significantly decreased in patients with OLP (p<0.001). In addition, a positive correlation was found between the decrease in the salivary amount of vitamin C and that in vitamin E in patients and controls. In addition to the lower salivary levels of antioxidant vitamins and the lower TAC, the higher level of MDA in patients with OLP suggests that free radicals and the resulting oxidative damage may be important in the pathogenesis of OLP lesions.
The exact causes of oral lichen planus (OLP) which is a long standing mucocutaneous illness are not completely discovered. However infiltration of large numbers of lymphocytes could be found in the affected erea.1,2
Oral pain resulted from OLP could be ranged from a little bothersome to annoying pain inhibits patients from their daily function.3 OLP could be found with different manifestation including white stria or papules, erythematouse lesions and also bullae.4 Buccal mucosa, tongue as well as gums are the common sites for OLP. OLP could be found in about 2% of people all around the world, more commonly in women aged between 40 to 60 years old.5
There are different factors could play as triggers to induce OLP. Genetic susceptibility, immunological illnesses, malnutrition as well as infectious agents are factors which could be considered as triggers for OLP.6 Besides all factors mentioned above upper level of reactive oxygen species (ROS) and lipid peroxidation may be related to OLP.7
Any certain condition which leads to increased level of ROS or reduced function of antioxidant including over production of ROS or impaired ROS removal is called oxidative stress. ROS could be toxic to cells via inactive enzymes, denaturizing proteins, DNA destruction, and lipid peroxidation. These events lead to damaged cell membrane and increase reactive aldehydic materials like malondialdehyde (MDA). MDA is a useful determinant to show high level of lipid peroxidation8 which lead to impaired cell function. Previous studies mentioned there is a relation between high oxidative stress and low anti oxidant activity in those who have OLP.9
There are different types of scavengers for free radicals consist of different enzymes, minerals as well as vitamins.10 vitamin A and E inhibits lipid peroxidation of cell membrane and vitamin C plays as a cofactor for many enzymes which stabilizing collagen triples helical structure. Besides, vitamin C could help to reproduce vitamin E from its radical root.10
Saliva according to its non-invasive and easy collection and also its composition changes due to many illnesses could be considered as a suitable media for diagnosis different conditions. As it was shown by different studies saliva is useful for diagnosis and also monitoring general health status.11 However, using saliva for determination of OLP indicators is not a common practice. It is assumed that markers of oxidative stress are associated with different local oral condition. The level of antioxidant is a potential determinant of susceptibility to be affected by OLP. This suggest that oxidative stress is major triggers for OLP.11,12,13
Evaluation salivary total antioxidant capacity (TAC) may result in valuable data about different condition in patients' systems which result in higher risk for diseases such as OLP.13 Based on knowledge we have, although there are some data about the relationship between salivary antioxidant of lichen planus, no survey evaluate the effect of vitamin A level on OLP incidence. The aim of the present study was to compare the level of lipid peroxidation, TAC and antioxidant vitamins in those with OLP and healthy subjects.
This case-control investigation has done in Oral Medicine department of Dental faculty, Hamadan University of Medical Sciences, Islamic Republic of Iran in 2012-2013. Admission form was taken from each participant and the investigation protocol was approved by ethical department. 36 patients who had OLP (22 women and 14 men) and referred oral medicine department participated in the study. Because oral erosive LP is a precancerous lesion, that may be contribut to alter the amounts of antioxidants. We choose these patients as the case group. The mean age of patients was 43.1=9.6 years. The sex and age of the cases were matched to controls who were chosen from the healthy staff of the faculty. Controls also participated in the study after providing written constant. All of 36 healthy subjects (21 women and 15 men) who were free of oral mucosal disease participated in control group (mean age: 40.1=6.1 years).
The history of using alcohol and cigarette, social factors were taken in a questionnaire.
The inclusion criteria were a biopsy-proven diagnosis of erosive OLP that had two microscopic characters: the first one was band like infiltration of lymphocytes and the other was degeneration of the basement membrane layer. Exclusion criteria were lichenoied reaction to amalgam restoration or drug induced reaction.
Systemic disease (including any autoimmune disease or malignancy or diabetes mellitus), use of any oral drugs and vitamins in last 3 months. History of trauma, surgery about 1 month age was other exclusion criteria.14
Saliva collection can be done from an individual gland or from all of glands that exert oral fluid (whole saliva).
In our study we needed to have whole saliva so for this purpose we decided to use spitting method. In this method samples should be collected 90 minutes after the last eating or drinking at the same time of day. In the first step the patients were rinsed his mouth with water, then sitting in a relax position, after 5 minutes the accumulated saliva (unstimulated saliva), expectorates into preweighted tube.
The collected saliva samples were centrifuged at 4,000 g at 4℃ for 10 minutes, immediately. The supernatants were stored at 80℃ for analysis.
The TAC was identified by measuring the ability to decrease Fe3+ to Fe2+ by use of the ferric reducing ability of plasma (FRAP) test as mentioned in aprevious study.15 Briefly, in this method the medium was exposed to Fe3+ and the anti oxidants was appeared in the medium beginning to produce fe2+ as an activation of antioxidant. By mixing 300 mM acetate buffer (pH=3.6), 10 mM 2, 4, 6 tripyridyl-s-trazine (TPTZ) solution and 20 mM FeCl3. 6 H2O in a 10:1:1 ratio. The working FRAP reagent was produced, just before use and heating the mixture to 37℃. By preparing a solution of 10 m M TPTZ in 40 m M HCl, the TPTZ was made. An H2O-diluted sample was then added to 300 ml freshly prepared reagent warmed at 37℃. A blue color has appeared from the complex between Fe2+ and TPTZ. The colored complex was absorbed and recorded at 593 nm by use of a Tecan Sunrise Microsplate Reader (Tecan, Groding, Ausria).
The level of salivary MDA was measured by a method based on reaction with thiobarbituric acid (TBA) at 96 to 100℃.16 In this test MDA and TBA influence together for produce a pink pigment that absorbed maximum at 532 nm.
The reaction was performed at a pH of 2 to 3 at 90℃ for 15 minutes for precipitating the protein it was needed. The sample mixed with 2 volumes of cold 10% (w/v) trichloroacetic acid. The protein was pelleted by centrifugation, and an aliquot of the supernatant was reacted with an equal volume of 61% (w/v) TBA in a boiling water bath for 10 minutes. The absorption area was read at 552 nm after cooling. According to a standard diagram the results were assessed as M mol/l which was prepared with a serial dilution of standard 1, 1, 3, 3-tetramelhoxypropane.
The level of salivary vitamin A and vitamin E was Analyzed in duplicate by using commercially available ELISA kits (Shanghai Crystal Day Biotech Co., LTD, China), and the mean values of the duplicates were used to analyze the results. These ELISA kits are based on the principle of the double-antibody sandwich technique to detect human vitamin A and vitamin E in saliva samples. The sensitivity of the kits was 1.21 ng/ml and 0.011 nmol/ml for assay of vitamin A and vitamin E, respectively. The intra and inter assay coefficients of variation were <10% and <12%, respectively.
Total vitamin C analysis was conducted according to the method of Roe and Kuether,17 which is based on the development of a color product as a result of the reaction of dehydroascorbic acid with dinitrophenylhydrazine.
The data were statistically analyzed by using the SPSS statistical package (SPSS, version 17.0, Chicago, IL, USA). Student's t-test for independent samples was used to determine the statistical significance amounts of unstimulated whole saliva MDA, TAC, vitamin C, vitamin E, and vitamin A within both patient and control groups. Correlation assessments were performed by using the Spearman correlation analysis.
Statistical difference was explained the correlation assessments by using the spearman correlation analysis. Statistical difference was considered significant at p<0.05.
There were no statistically significant differences in the ages or sex distributions of the patients and the controls (p=0.06, p=0.66, respectively).
Fig. 1 shows the comparison of salivary MDA and TAC levels between the cases and controls.
Our study revealed higher salivary MDA in cases than in controls. The mean value of salivary MDA in cases was 5.59±2.05 µmol/l, whereas , the mean value in controls was 3.42±1.44 µmol/l. This difference was statistically significant with a p value of <0.001. The mean salivary TAC level (0.136±0.01 mmol/l) in patients with OLP was significantly lower than that of controls (0.205±0.02 mmol/l); (p<0.001), as illustrated in Fig. 1B.
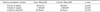
The comparison of salivary antioxidant vitamin levels between cases and controls is shown in Table 1. Salivary vitamin A ,C, and E levels were lower in cases as than in controls and The difference was statistically significant.
There was a significant positive correlation between the decrease in vitamin C and that in vitamin E in patients and controls (r=0.37, p=0.001); (Fig. 2).
ROS and antioxidants imbalances may have a main role in OLP development.12,18 Therefore, in the current study the we evaluated the levels of MDA, TAC and the antioxidant vitamins A, C and E in the saliva of patients with OLP. The antioxidant defense systems are highly complex,8,12 and effective against ROS. It is essential to evaluate the amounts and the action of the different antioxidants for in vivo evaluation of antioxidant status. Considerable evidence suggests a role for nutrients, particularly the so-called antioxidants vitamin A, vitamin C, and vitamin E in the pathogenesis of OLP.19 In the current study, we observed that the levels of the antioxidant vitamins A, C and E in saliva were significantly lower in patients with OLP than healthy control group. The possible protective effects of vitamins in reducing the risk of OLP may be related to antioxidant role in eliminating free radical damage and single oxygen.20 The fact that antioxidant vitamins are effective against oxidative stress may explain the significant difference between healthy individuals and patients with OLP. Consistent with our findings, Barikbin et al.,21 found a significant decrease in salivary levels of vitamin C and vitamin E in patients with OLP. In contrast to our study, Nagao in a case control study about serum antioxidant in patients with OLP showed higher levels of retinol in OLP.7
There was a significant positive relation between the decrease invitamin C and that in vitamin E in patients and controls in the present study. Vitamin C interact with vitamin E in the watery environment of the cells and lipid rich areas of the cell and regenerating vitamin E by a non-enzymatic mechanism.22
Our study showed a decline in TAC in patients with OLP which is in agree with a number of previously published studies. The antioxidant capacity reduction in our study may show cellular damage by oxidative processes.13
Our finding indicated that salivary MDA level was higher in patients with OLP than healthy control group. We believe that, decreased antioxidant defense mechanism led to increased ROS and MDA production. Increased oxidative stress may be primary pathogenic event or a because of the inflammatory process in OLP.23 Higher MDA levels in our findings was similar to other studies. Hassan et al.,24 demonstrated high MDA level in lichen. Altered oxidative DNA damage, protein oxidation, enzymatic antioxidant defenses increase MDA level. In Sezer et al.,12 study MDA serum levels was also increased in lichen planus group than the control group. MDA levels also was high in lichen planus, leukoplakia, and cancer.25
Our findings highlight that saliva may be easy and valid diagnostic fluid in patients with OLP.
In current study we matched the subjects' ages and sex, so we excluded the effect of these variables on results. Antioxidant defense decreases with age and male sex because estrogens and estradiol have antioxidant properties.26
In conclosion, there was relationship between oxidative stress and MDA with OLP. The TAC levels also was low in patients with lichen planus. Our results indicate that salivary antioxidant vitamin (vitamin A, vitamin E, and vitamin C) levels are significantly lower in patients with OLP. In addition, vitamin C and vitamin E showed a positive correlation. All together , further studies need to be done to demonstrate oxidative stress role in OLP etiopathogenesis.
Figures and Tables
FIG. 1
The unstimulated whole saliva concentrations of (A) malondialdehyde (MDA) and (B) total antioxidant activity (TAC) in cases (patients with erosive oral lichen planus) and controls (healthy subjects). *Indicates significant difference with control (p<0.001).

ACKNOWLEDGEMENTS
The present research has been done according to the post graduate thesis submitted to Hamadan University of Medical Sciences. The researchers want to express their sincere to vice chancellor for research and technology of Hamadan University of medical sciences for their supports.
References
1. Porter SR, Kirby A, Olsen I, Barrett W. Immunologic aspects of dermal and oral lichen planus: a review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997; 83:358–366.
2. Walsh LJ, Savage NW, Ishii T, Seymour GJ. Immunopathogenesis of oral lichen planus. J Oral Pathol Med. 1990; 19:389–396.

3. Thongprasom K, Chaimusig M, Korkij W, Sererat T, Luangjarmekorn L, Rojwattanasirivej S. A randomized-controlled trial to compare topical cyclosporin with triamcinolone acetonide for the treatment of oral lichen planus. J Oral Pathol Med. 2007; 36:142–146.

4. Roopashree MR, Gondhalekar RV, Shashikanth MC, George J, Thippeswamy SH, Shukla A. Pathogenesis of oral lichen planus--a review. J Oral Pathol Med. 2010; 39:729–734.
5. Chainani-Wu N, Silverman S Jr, Lozada-Nur F, Mayer P, Watson JJ. Oral lichen planus: patient profile, disease progression and treatment responses. J Am Dent Assoc. 2001; 132:901–909.
6. Nielsen F, Mikkelsen BB, Nielsen JB, Andersen HR, Grandjean P. Plasma malondialdehyde as biomarker for oxidative stress: reference interval and effects of life-style factors. Clin Chem. 1997; 43:1209–1214.

7. Nagao T, Warnakulasuriya S, Ikeda N, Fukano H, Yamamoto S, Yano M, et al. Serum antioxidant micronutrient levels in oral lichen planus. J Oral Pathol Med. 2001; 30:264–267.

8. Alfadda AA, Sallam RM. Reactive oxygen species in health and disease. J Biomed Biotechnol. 2012; 2012:936486.

9. Scully C, Beyli M, Ferreiro MC, Ficarra G, Gill Y, Griffiths M, et al. Update on oral lichen planus: etiopathogenesis and management. Crit Rev Oral Biol Med. 1998; 9:86–122.

10. Keller KL, Fenske NA. Uses of vitamins A, C, and E and related compounds in dermatology: a review. J Am Acad Dermatol. 1998; 39:611–625.

11. Yang LL, Liu XQ, Liu W, Cheng B, Li MT. Comparative analysis of whole saliva proteomes for the screening of biomarkers for oral lichen planus. Inflamm Res. 2006; 55:405–407.

12. Sezer E, Ozugurlu F, Ozyurt H, Sahin S, Etikan I. Lipid peroxidation and antioxidant status in lichen planus. Clin Exp Dermatol. 2007; 32:430–434.

13. Azizi A, Farshchi F. Comparison of salivary and plasma antioxidant levels in lichen planus patients and healthy subjects. J Oral Pathol Med. 2012; 41:524–526.

14. Al-Hashimi I, Schifter M, Lockhart PB, Wray D, Brennan M, Migliorati CA, et al. Oral lichen planus and oral lichenoid lesions: diagnostic and therapeutic considerations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:Suppl. S25.e1–S25.e12.

15. Benzie IF, Strain JJ. Ferric reducing/antioxidant power assay: direct measure of total antioxidant activity of biological fluids and modified version for simultaneous measurement of total antioxidant power and ascorbic acid concentration. Methods Enzymol. 1999; 299:15–27.
16. Esterbauer H, Zollner H. Methods for determination of aldehydic lipid peroxidation products. Free Radic Biol Med. 1989; 7:197–203.

17. Roe JH, Kuether CA. The determination of ascorbic acid in whole blood and urine through the 2,4-dinitrophenylhydrazine derivative of dehydroascorbic acid. J Biol Chem. 1943; 147:399–407.

18. Aly DG, Shahin RS. Oxidative stress in lichen planus. Acta Dermatovenerol Alp Pannonica Adriat. 2010; 19:3–11.
19. Mohit B, Shelja V, Nidhi G, Sunint S. Antioxidants - Its Preventive Role In Oral Cancer. Indian J Dent Sci. 2012; 4:103–105.
21. Barikbin B, Yousefi M, Rahimi H, Hedayati M, Razavi SM, Lotfi S. Antioxidant status in patients with lichen planus. Clin Exp Dermatol. 2011; 36:851–854.

22. Chan AC. Partners in defense, vitamin E and vitamin C. Can J Physiol Pharmacol. 1993; 71:725–731.

23. Agha-Hosseini F, Mirzaii-Dizgah I, Mikaili S, Abdollahi M. Increased salivary lipid peroxidation in human subjects with oral lichen planus. Int J Dent Hyg. 2009; 7:246–250.

24. Hassan I, Keen A, Majid S, Hassan T. Evaluation of the antioxidant status in patients of lichen planus in Kashmir valley - A hospital based study Iffat Hassan. J Saudi Soc Dermatol Dermatol Surg. 2013; 17:13–16.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download