Abstract
Clinical and laboratory data from Western countries suggest that pregnant women are at an increased risk for severe illness and complications associated with 2009 pandemic influenza A (H1N1). However, previous data among Korean women suggested a less severe outcome. In this study performed at a single referral center in Korea, rates of admission, pneumonia, intensive care unit admission, and death related to 2009 pandemic influenza A (H1N1) were significantly higher in 33 pregnant women than in 723 nonpregnant women of reproductive age (p<0.05 each). We report two cases of 2009 pandemic influenza A (H1N1) in pregnant Korean women who were admitted to the intensive care unit because of severe pneumonia that led to maternal and fetal death in one of the patients. This case series suggests that pregnant Korean women were also at increased risk of severe illness and complications during the 2009 pandemic influenza A (H1N1) outbreak.
The 2009 pandemic influenza A virus (H1N1; hereafter, H1N1 2009) was reported for the first time in Mexico in April 2009 and subsequently spread globally. The virulence of the H1N1 2009 virus was not higher than that of seasonal influenza viruses, but the H1N1 2009 virus had higher transmissibility. For this reason, most of the infected patients recovered within a week without antiviral therapy, as typically occurs with seasonal influenza. However, complications and mortality related to H1N1 2009 were more frequently observed in patients with comorbidities, such as asthma, diabetes mellitus, cardiac disorder, pulmonary disorder, or neurologic disorder, and in the aged and infants, as is also the case for seasonal influenza.
It has been reported that pregnant women are at increased risk for severe illness and complications associated with not only seasonal influenza but also H1N1 2009, with the rates of spontaneous abortion and preterm birth being higher in infected pregnant women.1-5 Thus, current guidelines categorize pregnant women as high-risk patients for complications. In contrast to the current guidelines and reports from Western countries, a recent multi-center study performed in Korea suggested that the consequences of H1N1 2009 among pregnant Korean women were mild, because no serious cases were observed.6 However, the latter suggestion is controversial, because there is no theoretical basis supporting the difference in outcome between Korean and Western pregnant women with H1N1 2009.
We report two cases of severe H1N1 2009 infection in pregnant Korean women, one of which resulted in maternal and fetal death. These cases suggest that H1N1 2009 was not mild in Korean pregnant women.
From September 2009 to January 2010, 33 pregnant patients were confirmed by reverse-transcriptase polymerase chain reaction (RT-PCR) as being infected with H1N1 2009 in Chonnam National University Hospital. Thirty-one patients did not have complications but the other two (severe cases 1 and 2) were treated in the intensive care unit (ICU) owing to pneumonia and acute respiratory distress syndrome. The outcomes of H1N1 2009 between pregnant women and nonpregnant woman of reproductive age who visited Chonnam National University Hospital during the study period are shown in Table 1. Rates of admission, pneumonia, ICU admission, and death were significantly higher in pregnant women than in nonpregnant woman of reproductive age. The clinical characteristics of the admitted pregnant women with H1N1 2009 are shown in Table 2.
A 30-year-old female at 30 weeks of pregnancy had fever and cough. She had been diagnosed as having gestational diabetes mellitus (GDM) at 28 weeks of pregnancy and had been receiving insulin therapy. On the third day of fever, she was admitted to a nearby hospital and was administered ampicillin/sulbactam 1.5 g every 8 hours intravenously for 2 days. Despite treatment, her symptoms did not improve and hemoptysis occurred. She was transferred to Chonnam National University Hospital for correct diagnosis and further therapy.
Crackle was present in both lower lung fields on chest auscultation. Her vital signs were as follows: blood pressure of 90/60 mmHg, pulse rate of 88 beats/min, respiratory rate of 24/min, and body temperature of 36℃. The initial laboratory examination revealed a white blood cell count of 5,000/mm3, a hemoglobin level of 10.6 g/dl, and a platelet count of 157,000/mm3. The blood urea nitrogen level was 8.2 mg/dl, serum creatinine was 0.5 mg/dl, serum glucose was 110 mg/dl, and C-reactive protein was 8.7 mg/dl. On the initial arterial blood analysis performed after supplying oxygen 10 L/min by facial mask, the values of pH, PaO2, PaCO2, and bicarbonate ions were pH 7.5, 104 mmHg, 22.6 mmHg, and 18 mmol/L, respectively. Multifocal pulmonary infiltration in both lobes and pleural effusion were observed on chest radiography and computed tomography (Fig. 1).
After blood and sputum sampling for respiratory virus RT-PCR and bacterial culture, oseltamivir (300 mg/day), amantadine (200 mg/day), and ribavirin (900 mg/day) were administered on the basis of the clinical decision of nonsurvival of the fetus and the informed consent of the patient. Antibiotic therapy with piperacillin/tazobactam and clarithromycin was also initiated. On the second day of hospitalization, the patient was intubated and mechanical ventilation was started because of clinical deterioration. The Acute Physiology and Chronic Health Evaluation (APACHE) II score of the patient at the time of ICU admission was 12. The initial sputum RT-PCR for H1N1 2009 was reported to be positive. Bacterial culture revealed no specific pathogen. An H275Y neuraminidase gene mutation was not observed on sequence analysis performed at the Korea Centers for Disease Control and Prevention.7 On day 4 of admission, the fetal heart rate was lost. On day 11, natural birth after fetal death occurred and the antibiotics were changed to meropenem and teicoplanin. On day 23, extracorporeal membrane oxygenation (ECMO) was started. Despite administration of antibiotics, mechanical ventilation, inotropics, and ECMO, the pneumonia worsened and led to multi-organ failure. The patient died on day 25 of hospitalization.
A 34-year-old female at 26 weeks of pregnancy was diagnosed as having GMD but did not receive any medication. She displayed fever, chills, and cough. The next day, she visited Chosun University Hospital owing to persistent symptoms and the development of dyspnea. Influenza RT-PCR of throat and sputum samples was performed, with a positive result. Oseltamivir treatment was begun and the patient was transferred to Chonnam National University Hospital for further therapy.
Crackle was present in both lung fields on chest auscultation. Her vital signs were as follows: blood pressure of 150/90 mmHg, pulse rate of 131 beats/min, respiratory rate of 32/min, and body temperature of 36.6℃. The initial laboratory examination revealed a white blood cell count of 8,300/mm3, a hemoglobin level of 12.4 g/dl, and a platelet count of 142,000/mm3. The blood urea nitrogen level was 5.7 mg/dl, serum creatinine was 0.5 mg/dl, serum glucose was 115 mg/dl, and C-reactive protein was 12.5 mg/dl. On initial arterial blood analysis, the values of pH, PaO2, PaCO2, and bicarbonate ions were pH 7.45, 52 mmHg, 25 mmHg, and 20 mmol/L, respectively. Multifocal peribronchial and subpleural consolidations and ground glass opacities with air-bronchogram in both lungs were observed on chest radiography and computed tomography (Fig. 2). Urinary antigen tests for Streptococcus pneumoniae and Legionella were negative.
Oseltamivir (300 mg/day) and zabamivir inhaler were administered for 5 days. Ceftriaxone and azithromycin were also administered empirically for 7 days and 5 days, respectively. On day 3 of hospitalization, she was transferred to the intensive care unit owing to aggravation of metabolic acidosis and hypoxia. The APACHE II score of the patient at the time of ICU admission was 18. Bacterial culture revealed no specific pathogens. Her symptoms gradually improved and the patient was discharged on day 13 without any remnant morbidity or fetal complication. Delivery by cesarean section because of macrosomia associated with GDM occurred 13 weeks later.
In this study, we report two complicated cases of pregnant Korean women infected with H1N1 2009.
Although clinical data from Western countries have shown that pregnant women are at an increased risk for severe illness and complications associated with H1N1 2009,1-5 little is known about the biological reasons for the risk of pregnant women. However, a recent study showed that pregnant women have attenuated innate interferon responses to H1N1 2009 virus, and that vaccination can significantly improve the attenuated innate and adaptive immunity in pregnancy.8 Another study reported a decreased concentration of adiponectin in pregnant and obese patients, which is the potential activator of the innate immune system against H1N1 2009 infection, involving molecules including interleukin (IL)-1 receptor associated kinase M, IL-10, and nuclear factor-kappa B.9
Although immunological and clinical data from Western countries showed that pregnant women are immunologically more susceptible to influenza and at risk of severe illness, a previous multicenter study performed in Korea suggested that H1N1 2009 among pregnant Korean women was mild, because no serious cases were observed in that study.6 However, a fatal case in a pregnant woman was subsequently reported in one of the participating hospitals.10 In that case, antiviral agents had not been administered out of concern for the possible impact on the fetus. In the present study, the outcomes of H1N1 2009 were significantly worse in pregnant women than in nonpregnant women of reproductive age. In our study, antiviral agents were also administered belatedly in the fatal case, although antibacterial agents were empirically administered earlier. These cases suggest that H1N1 2009 can also be serious and fatal in Korean pregnant women, and an early diagnostic test for influenza and empirical antiviral administration is required in the case of community-acquired pneumonia in pregnant women in the influenza epidemic period in Korea, as in Western countries,4 rather than reluctance to treat owing to the impact of antiviral agents on the fetus.
In our study, both women with complicated H1N1 2009 had GDM and a high body mass index. There are no conclusive results about an increased risk of complications of H1N1 2009 in pregnant women with GDM. However, diabetes mellitus and obesity are known independent risk factors of pandemic influenza infection and complications, and it has been suggested that there is an increase in complications in pregnant women with underlying medical conditions.5 Thus, more care and treatment with early diagnosis and aggressive vaccination of pregnant women with GDM, a high body mass index, or other risk factors may be warranted.
Figures and Tables
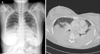 | FIG. 1Results of the chest radiography and the computed tomography performed on the day of admission in Case 1. Multifocal pulmonary infiltration in both lobes and pleural effusion were observed on chest radiography and computed tomography. |
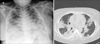 | FIG. 2Results of the chest radiography and the computed tomography performed on the day of admission in Case 2. Multifocal peribronchial and subpleural consolidations and ground glass opacities with air-bronchogram in both lungs were observed on chest radiography and computed tomography. |
TABLE 1
Comparison of the outcomes of 2009 pandemic influenza A (H1N1) between pregnant women and nonpregnant women of reproductive age who visited Chonnam National University Hospital during the period of September 2009 to January 2010

References
1. Jamieson DJ, Honein MA, Rasmussen SA, Williams JL, Swerdlow DL, Biggerstaff MS, et al. Novel Influenza A (H1N1) Pregnancy Working Group. H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet. 2009; 374:451–458.
2. Louie JK, Acosta M, Jamieson DJ, Honein MA. California Pandemic (H1N1) Working Group. Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med. 2010; 362:27–35.

3. Siston AM, Rasmussen SA, Honein MA, Fry AM, Seib K, Callaghan WM, et al. Pandemic H1N1 Influenza in Pregnancy Working Group. Pandemic 2009 influenza A(H1N1) virus illness among pregnant women in the United States. JAMA. 2010; 303:1517–1525.

4. ANZIC Influenza Investigators and Australasian Maternity Outcomes Surveillance System. Critical illness due to 2009 A/H1N1 influenza in pregnant and postpartum women: population based cohort study. BMJ. 2010; 340:c1279.
5. Hewagama S, Walker SP, Stuart RL, Gordon C, Johnson PD, Friedman ND, et al. 2009 H1N1 influenza A and pregnancy outcomes in Victoria, Australia. Clin Infect Dis. 2010; 50:686–690.

6. Kim BN, Kwak YG, Moon CS, Kim YS, Kim ES, Lee KS, et al. Pandemic influenza (H1N1 2009) among pregnant Korean women. Infect Chemother. 2011; 43:55–59.

7. Hong SD, Park SH, Kang SJ, Kwon YS, Kee SJ, Park KH, et al. First fatal oseltamivir-resistant 2009 pandemic influenza A (H1N1) case in an adult in Korea. Chonnam Med J. 2011; 47:127–129.

8. Forbes RL, Wark PA, Murphy VE, Gibson PG. Pregnant women have attenuated innate interferon responses to 2009 pandemic influenza A virus subtype H1N1. J Infect Dis. 2012; 206:646–653.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download