INTRODUCTION
Pseudomyxoma peritonei (PMP) is a rare clinical condition that results in the accumulation of mucinous ascites.1,2 PMP is generally thought to originate from an appendiceal mucinous neoplasm, most commonly a mucinous adenoma.1 Rare origins such as the ovary, pancreas, urachus, and ascending colon have also been reported in the literature.1-5 Mucus produced by mucinous tumor cells gradually fills the abdominal cavity and progressively causes symptoms related to the compression of intra-abdominal organs. Although the clinical symptoms of PMP vary according to the extent and origin of the mucinous ascites, the most common presentation is abdominal distention and pain that can mimic acute appendicitis or bowel obstruction. Constitutional symptoms such as poor oral intake and weight loss are often present. Given these non-specific clinical signs and symptoms, as well as the lack of laboratory findings to aid in diagnosis, debulking surgery is often performed before the diagnosis of PMP. Computed tomography (CT) with contrast is considered the optimal diagnostic imaging tool to characterize the extent of involvement of the intra-abdominal organs. Here, we present a case of oliguric acute kidney injury (AKI) caused by external compression by untreated PMP.
CASE REPORT
A 53-year-old man presented to the emergency department with poor oral intake and abdominal distension. He had been admitted to other hospitals with abdominal distention twice over the previous year, at which time abdominal CT had shown moderate ascites. He underwent gastroduodenoscopy and colonoscopy to rule out gastrointestinal malignancy, but the results were unrevealing. He refused further evaluation at that time and had stopped seeking conventional medical care in favor of alternative medicine. At the present admission, he complained of a 5-kg weight loss over the previous month and intermittent vomiting for several weeks. The physical examination revealed a tense, distended abdomen with no palpable mass. His blood pressure was 110/70 mmHg and his pulse was 92 beats/minute. His mucous membranes were dry, his skin turgor was poor, and his initial urine output was less than 10 ml/hour for 12 hours. Laboratory evaluation showed severe azotemia (blood urea nitrogen, 66.3 mg/dl [normal range, 3-23 mg/dl]; creatinine, 2.86 mg/dl [normal range, 0.3-1.6 mg/dl]), decreased serum sodium and chloride (Na, 130 mmol/L [normal range, 133-146 mmol/L]; Cl, 85 mmol/L [normal range, 99-110 mmol/L]), and decreased urine sodium and chloride (Na<10 mmol/L, Cl<10 mmol/L). The fractional excretion of sodium was reduced to 0.1%. Tumor markers were elevated: CEA was 25.0 ng/ml (normal range, 0-5 ng/ml) and CA 19-9 was 142.6 IU/ml (normal range, 0-37 IU/ml). Other biochemical findings were normal. A chest x-ray showed subsegmental atelectasis of both lower lungs. His creatinine level was markedly elevated compared with the last level of 0.9 mg/dl measured 9 months previously and continued to rise steadily up to 3.4 mg/dl at 48 hours after admission. The findings were consistent with AKI as defined by the Acute Dialysis Quality Initiative group.6
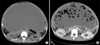
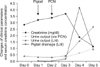
Owing to the patient's volume depletion, we initiated volume resuscitation with normal saline (4 L/day). His urine output did not improve, however, so we obtained a non-contrast CT of the abdomen, which revealed massive ascites of the abdomen and pelvis, diffuse peritoneal thickening, infiltration of the greater omentum, and hydronephrosis and hydroureter of the right kidney without an obstructing lesion in the urinary tract (Fig. 1A). Ultrasound-guided paracentesis yielded thick mucoid pus. A pigtail catheter was placed but was unable to drain the extremely thick fluid. Owing to the progression of azotemia and metabolic acidosis, a right percutaneous nephrostomy was performed, yielding urine amounts of less than 100 ml per day, which had no effect on the progressive kidney injury. The following day, after several attempts to irrigate, the pigtail catheter allowed nearly 4 L of thick ascites to drain, after which urine output increased to 2.7 L in 24 hours (Fig. 2) and creatinine dropped to 1.16 mg/dl. The follow-up CT with contrast is shown in Fig. 1B. Unfortunately, the patient's symptoms did not improve along with restoration of his renal function. Accordingly, gastroduodenoscopy and colonoscopy were performed, which showed chronic gastritis and several colon polyps that were biopsied and found to be tubulovillous adenomas with high-grade dysplasia. Exploratory laparoscopy confirmed massive mucin-rich ascites suggestive of PMP.
Debulking surgery was performed to remove the mucinous ascites. Histopathologic findings of samples from the cystic wall and peritoneum of the ascending colon confirmed the diagnosis of PMP and mucinous cystadenoma. The findings of the surface encased with mucus and mucinous epithelium with minimal atypia indicated low-grade PMP (Fig. 3A) and immunohistochemistry was positive for cytokeratin 20 and negative for cytokeratin 7, which suggested an origin of the lower gastrointestinal tract (Fig. 3B).
DISCUSSION
PMP is a rare clinical condition with an incidence of 1 to 2 cases per 1 million persons annually that causes the progressive accumulation of mucinous ascites.1,7 Presenting symptoms are usually vague and associated with increased abdominal girth. The serum tumor markers CEA and CA 19-9 are reported to be elevated in approximately 50% of patients with PMP.1 Without treatment, patients gradually develop partial or complete intestinal obstruction from the compressing tumor and ascites. In our case, the accumulation of massive ascites resulted predominantly in the compression of the right ureter, which contributed to oliguric post-renal AKI. Furthermore, the partial bowel obstruction had resulted in vomiting and poor oral intake for a prolonged period, which had caused severe volume depletion, thus contributing to pre-renal AKI. Notably, volume repletion alone had little effect on resolution of the AKI.
Although we did not measure the intra-abdominal pressure (IAP), previous animal experiments suggested that IAP above 20 mmHg is associated with oliguria and values above 40 mmHg are associated with anuria.8 Because urine output was increased after decompression of the ascites by pigtail insertion with irrigation, it is suggested that increased IAP may have been the predominant cause of the acute oliguric kidney injury in this case. In several reported cases, the right kidney is usually involved with or without direct invasion of the urinary tract, with the PMP originating in the retroperitoneal spaces. In the literature, there are few case reports of AKI as a complication of PMP.9 In our case, combined treatment with volume repletion and decompression of the ascites rapidly restored our patient's renal function.
Most cases of PMP originate from mucinous tumors of the appendix,7 although rare cases originating from the ovary, colon, gall bladder, pancreas, and retroperitoneum have been reported. In our case, a colorectal or appendiceal origin was confirmed only by immunohistochemical markers, because explorative laparoscopy revealed no visible tumor mass in the appendix. Also, chronic inflammatory changes associated with delayed treatment caused severe intraperitoneal adhesions that prevented the dissection of the tumor from the entangled peritoneum.
After confirmation of PMP, surgical management is indicated owing to the disease's progressive nature. Untreated, PMP will gradually compress intra-abdominal organs and cause peritoneal adhesions, as in our case. In 1980, reported 5- and 10-year survival rates were only 54% and 18% without adequate treatment. PMP is usually treated with resection of the original tumor site with debulking surgery, which may be repeated several times as described in previous case reports.10 New treatments using chemotherapy in combination with surgery have been proposed in several reports but have not yet been evaluated in systematic trials.
PMP is usually manifested by mucinous ascites that eventually leads to gross abdominal distension. Most reported cases do not show evidence of renal dysfunction. However, IAH induced by progressive mucinous ascites could induce abdominal compartment syndrome and result in AKI. Finally, multiple organ systems can be affected with disastrous outcomes. For these reasons, a high index of clinical suspicion and intervention is critical for appropriate management of AKI. Although there have been a few case reports of AKI in patients with PMP, this case serves as a good reminder of a potentially treatable cause of AKI.
In conclusion, we report a rare case of oliguric AKI caused by untreated PMP that resolved rapidly after decompression of massive ascites. Owing to the disease's progressive nature and poor prognosis, prompt recognition and decompression therapy can improve the clinical course.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download