INTRODUCTION
Gastric cancer is one of the most common cancers in Korea, and at the time of diagnosis, approximately 20% of gastric cancer patients have stage IV disease that commonly involves the liver, lung, and bone.1,2 Brain metastases of gastric cancer are uncommon and have been reported in <1% of clinical cases.3,4 The most common form of brain metastasis of gastric cancer is meningeal carcinomatosis, whereas solitary metastases to the brain parenchyma are extremely rare.2-4 Brain metastasis, when presenting as a sign of gastric cancer, is usually a late clinical course disease manifestation and is associated with short overall survival.2,3,5 We report an exceptionally rare case of gastric cancer in which the only initial presenting symptoms were unilateral facial palsy and hearing loss that mimicked acoustic neuroma and that were due to a solitary brain metastasis in the cerebellopontine angle.
CASE REPORT
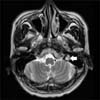
A 57-year-old man visited our hospital in April 2012 with the complaints of left hearing loss and left facial paralysis of approximately 3 weeks' duration. He had no significant previous medical history and no complaints of gastrointestinal symptoms such as nausea, abdominal pain, melena, hematochezia, or weight loss. In the abdominal examination, neither a palpable mass nor hepatosplenomegaly was noted. A neurological examination showed the loss of left-side forehead creases, the patient's inability to close his left eye, left facial muscle weakness, a rightward deviation of the mouth angle upon smiling, and a loss of the left nasolabial fold. His sensory and motor functions in the upper and lower extremities were normal. Cytological examination of the cerebrospinal fluid revealed no evidence of malignancy. Magnetic resonance imaging (MRI) of the brain showed a 1×1.5 cm tumor in the cerebellopontine angle that extended to the inner auditory canal. The tumor was clinically diagnosed as an acoustic neuroma (Fig. 1). Owing to the diagnosis of a benign tumor such as acoustic neuroma, the patient underwent surgery via the translabyrinthine approach, and the tumor was completely removed. In contrast with our initial diagnosis, however, the pathological examination of the surgical specimen revealed cells from a poorly differentiated metastatic carcinoma. Immunohistochemical staining did not help to identify the primary site. A further investigation to identify the primary lesion was performed postoperatively. Blood chemistry analysis indicated a serum carcinoembryonic antigen level of 1.34 ng/ml (reference range, 0-5 ng/ml). Other tumor markers were within normal limits. Abdomen/pelvic and thoracic computed tomography (CT) scans revealed no evident masses or regional lymphadenopathy that would suggest malignancy, except for a hepatic cyst, renal cyst, and mild splenomegaly. A positron emission tomography (PET)-CT scan revealed an abnormal hypermetabolic lesion in the stomach antrum but no other metastatic lesions. An upper gastrointestinal endoscopy examination found active ulcerative lesions on the anterior wall of the gastric antrum that were compatible with Borrmann type II gastric cancer. The pathological examination of the gastric antrum revealed cells from a poorly differentiated carcinoma. A total gastrectomy was performed and a pathological analysis of the surgical specimen revealed a poorly cohesive carcinoma that was histopathologically identical to that of the resected brain tumor (Fig. 2). On the basis of the results of the pathological examination, the case was finally diagnosed as gastric cancer with a solitary brain metastasis and was graded according to the TNM staging system as pT2 (invasion of proper muscle), N3b (involvement of 21 of 43 lymph nodes), and M1 (brain metastasis). According to the final pathology report, lymphovascular and venous invasion of gastric cancer were observed in the surgical specimen. The patient received palliative combination chemotherapy with intravenous oxaliplatin 130 mg/m2 of body surface area (BSA) on day 1 and oral capecitabine 2,000 mg/m2 of BSA on days 1 to 14 every 3 weeks. After 3 cycles of the combination chemotherapy, follow-up abdomen/pelvic CT scan and brain MRI showed no evidence of recurrence. The patient continued to receive the palliative combination chemotherapy on an outpatient basis, with a disease-free survival duration of 45 weeks.
DISCUSSION
Previously, the incidence of stage IV gastric cancer at the time of diagnosis was reported to range from 20% to 30%.2 York et al.2 reported that during a 40-year period, only 24 of 3,320 patients (0.7%) with gastric cancer at the MD Anderson Cancer Center were found to have brain metastases. In Korea, where the incidence of gastric cancer is among the highest in the world, cases of gastric cancer with brain metastases are extremely rare and occur in <1% of gastric cancer patients.6 The most common sites of metastasis of gastric cancer are the liver, lungs, and bones.2,3 The small number of reported cases of metastasis to unusual sites such as the mouth, penis, and skin is apparent.7-9 In most cases, brain metastatic lesions of gastric cancer are among multiple systemic metastatic lesions that occur during the clinical course. Although central nervous system (CNS) involvement in gastric cancer is relatively rare, the most common CNS metastatic form is leptomeningeal carcinomatosis, with an incidence of 0.06% of all Korean gastric cancer cases.6 In contrast, isolated metastases to the cerebral parenchyma are exceptionally rare. As far as we know, this is the first case report in Korea of a solitary brain parenchyma metastasis as the initial presentation of gastric cancer, without the involvement of other organs.
Gastric cancer usually presents with gastrointestinal symptoms such as abdominal pain, anorexia, nausea, and vomiting.2 Symptoms due to distant metastasis alone are uncommon in gastric cancer, with an incidence of <5% of published cases.3,6 Brain metastasis of gastric cancer is usually a late event in the clinical disease course. In most reports, metastases were detected after the appearance of the primary tumor. In our case, however, no definite gastrointestinal symptoms were present in the initial findings. Based on the location and radiological characteristics of the tumor on conventional MRI, and the patient's clinical manifestations, the preoperative diagnosis of the brain lesion was clinically acoustic neuroma, which is the most frequently occurring tumor in the cerebellopontine angle. Most acoustic neuromas are benign and present with variable clinical symptoms, such as hearing loss, tinnitus, and balance abnormalities. Puri et al.10 reported 3 unusual cases in which symptoms associated with a distant metastasis were the first presentation of gastric cancer. In their report, 3 patients presented with metastases in the extremity skin, bone, and lung. Similar to our case, no symptoms related to the primary cancer were noted in those cases.
The overall prognosis of patients with brain metastasis of gastric cancer is very poor, with a median survival of approximately 9 to 54 weeks in published reports.1-3 York et al.2 performed a retrospective review of 24 patients who received 3 treatment modalities, including the administration of steroids alone (group 1), whole-brain radiation therapy (WBRT) plus steroids (group 2), and WBRT plus steroids in addition to surgical resection (group 3). The overall survival outcomes of each treatment group were similar, with a median survival of 9 weeks. Kasakura et al.5 reported that a longer median survival was observed in patients who were treated with surgical resection (median survival, 28 weeks) than in those with WBRT (median survival, 10.8 weeks). Cases of solitary brain metastasis of gastric cancer are few in number. According to published reports, resection and/or radiotherapy are the main treatment options for patients with solitary brain metastases.2,5 However, even if the brain lesion is operable, resection might not be feasible if the patient is in poor general condition. Thus, in relatively young patients with less advanced systemic disease and good performance status, surgical resection alone or surgical resection followed by WBRT could lead to a relatively long survival.2,5 In our case, because the initial preoperative diagnosis was a benign tumor, our patient underwent surgical resection alone. Because the solitary brain tumor was completely removed and had negative pathological margins, additional WBRT was not done after resection of the primary gastric cancer. A disease evaluation performed after each 3 cycles of the combination chemotherapy revealed no evidence of local recurrence in follow-up brain MRI, and the patient had a disease-free survival duration of 45 weeks. In appropriate patients, surgical resection of a solitary brain metastasis could effectively increase survival duration.
In conclusion, we report an exceptionally rare case of gastric cancer in which the only initial presenting symptoms were unilateral facial palsy and hearing loss that mimicked acoustic neuroma, but that were due to a solitary brain metastasis in the cerebellopontine angle. Brain parenchyma metastases are rare. To increase patient survival, surgical resection of solitary brain metastases of gastric cancer may be considered.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download