THE CASE: WHAT IS THE CAUSE OF IMPAIRED RENAL FUNCTION?
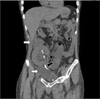
A 30-year-old male presented to Chonnam National University Hospital complaining of pitting edema of both lower extremities. He had received a kidney transplantation 1 month previously. A double J stent had been inserted to prevent urine leakage after kidney transplantation. The patient's medications consisted of tacrolimus, mycophenolate mofetil, and methylprednisolone. The physical examination showed a soft abdomen with right costovertebral angle tenderness. Laboratory studies were as follows: blood urea nitrogen, 24.7 mg/dl; serum creatinine, 1.4 mg/dl; and C-reactive protein, 3.5 mg/dl. One week later, the follow-up serum creatinine level had increased from 1.4 mg/dl to 3.0 mg/dl. The renal ultrasound showed a resistive index (RI index) of 0.53 and hypoechoic fluid collection in the pelvic cavity and around the transplanted kidney. Follow-up renal ultrasound showed hydronephrosis of the transplanted kidney (Fig. 1) and pelvic cavity fluid collection, which was confirmed by abdominal computed tomography (Fig. 2).
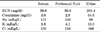
We performed dynamic renal scintigraphy by use of technetium99m diethylenetriamine penta-acetic acid. The scan showed focal tracer accumulation in the pelvic area, and there was evidence of abnormal leakage from the transplanted kidney and ureter (Fig. 3). To distinguish between lymphocele and urinoma, we conducted sono-guided percutaneous drainage of the fluid collected in the pelvic cavity (Fig. 4). Serum, urine, and aspirated peritoneal fluid chemistries were analyzed. The chemistry of the peritoneal fluid was more equivalent to the serum values than to the urinary values (Table 1).
THE DIAGNOSIS: LYMPHOCELE AFTER KIDNEY TRANSPLANTATION
The common etiologies of perirenal fluid collections occurring after kidney transplantation include urinomas, hematomas, abscesses, and lymphoceles.1 Examination of the aspirate fluid is an essential method for specifying the kind of perirenal and pelvic cavity fluid collection. Analysis of fluid composition is also helpful in identifying urine leakage, because higher creatinine and potassium concentrations and lower sodium concentrations are detected in urine than in lymphocele fluid.2,3 Indeed, urine fistulae may be responsible for perirenal collection, particularly early after surgery, through ureteral or bladder leaks. Perirenal hematomas occur during the postoperative period or after traumatism and are easily diagnosed by examining the fluid composition. Abscesses are also easily identified by aspirate white blood cell composition and bacterial cultures.1
The cause of lymphocele formation is unclear, but it is believed to result from transection of the lymphatic vessels accompanying the external iliac vessels during transplantation surgery and subsequent lymph accumulation in a nonepithelialized cavity in the extra-peritoneal plane adjacent to the transplanted kidney.4 The therapeutic options for lymphoceles occurring after kidney transplantation include simple aspiration under imaging control drainage with or without sclerotherapy and more invasive options of laparoscopic or open surgery to fenestrate the lymphocele into the peritoneal cavity. However, treatment decisions seem to be center-dependent.5 Our patient underwent simple aspiration and antibiotic treatments. His serum creatinine level decreased to within the normal range, and the hydronephrosis was resolved.
Because treatments of lymphocele and urinoma differ, it is important to clarify the cause of the perirenal fluid collection after kidney transplantation. In addition, early detection of transplantation-associated complications is expected to preserve renal function in patients with kidney transplantation.
In summary, we have presented a case of perirenal and pelvic cavity fluid collection after kidney transplantation. This case suggests that physicians should remember how to differentiate lymphocele and urinoma in postobstructive nephropathy in patients who have received a kidney transplant.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download