Abstract
The aim of this study was to evaluate the clinical effect of a continuous infusion of urokinase in cerebral stoke patients who were late admitted over 6 hours after onset. From January to December in 2008, acute cerebral stroke patients (n=143) treated with intravenous urokinase infusion (Group I, n=93) or not (Group II, n=50) after 6 hours and within 72 hours of stroke onset were reviewed. Continuous intravenous infusion of urokinase was done for 5 days. The clinical outcome for each patient was evaluated by using the modified National Institutes of Health Stroke Scale (NIHSS) on admission and on the day of discharge. The NIHSS score was decreased at discharge compared with admission in the urokinase treatment group (Group I; from 4.8±2.2 to 3.8±1.9; p=0.002). There was an improvement in the patients who initiated urokinase treatment within 24 hours from stroke onset in Group I (from 5.1±1.9 to 3.9±1.5; p=0.04). In patients with initiated urokinase treatment within 24 hours from stroke onset, intravenous urokinase infusion could be an effective modality in acute ischemic stroke patients admitted later than 6 hours after onset.
In several Korean hospitals, injecting urokinase intravenously has been applied for stroke patients who are admitted later than 6 hours after onset and in whom intraarterial thrombolysis or rt-PA (recombinant tissue-plasminogen activator) is not indicated because of the therapeutic time window of the these drugs, which is within 3 hours or 6 hours.1 However, studies on the intravenous injection of urokinase to stroke patients later than 6 hours after onset are meager and are lacking evidence of safety and effectiveness, except for a few studies in Korea and other countries.2
In the present study, the safety and clinical effectiveness of the continuous injection of urokinase to stroke patients later than 6 hours after onset were examined by comparison with control patients who were not treated with thrombolytics.
The study was conducted on patients treated with continuous injection of urokinase and patients treated with antiplatelet agents only who were selected from acute cerebral ischemic patients admitted between 6 hours and 72 hours after onset to the Department of Neurosurgery, Kwangju Christian Hospital, from January 2008 to December 2008. The demographic characteristics of the patients, risk factors, ischemic stroke subtypes, the interval from the onset of stroke to the administration of urokinase, and the interval from hospitalization to the administration of urokinase were analyzed. Patients treated with continuous intravenous urokinase injection were assigned as Group I, and patients treated with antiplatelet drugs only were assigned as Group II. In Group I (n=93), 47 patients were male, 46 patients were female, and the age distribution was from 43 years to 95 years (mean age, 73 years). In Group II (n=50), 28 patients were male, 22 patients were female, and the age distribution was from 41 years to 90 years (mean age, 66 years). Stroke types were classified according to the classification method of the Trial of Org 10172 in Acute Stoke Treatment (TOAST). Before the administration of urokinase, brain magnetic resonance imaging or brain computed tomography was performed in all patients, and cases with brain hemorrhage were excluded. In addition, cases in which the administration of thrombolytic agents was contraindicated, such as patients prone to bleeding, those with liver dysfunction, severe stroke patients close to brain herniation at the time of admission, and patients with poor general condition, were excluded from the study.
During the administration of urokinase, if neurological symptoms deteriorated or new symptoms developed, urokinase injection was terminated, brain computed tomography was performed immediately, and the presence or absence of hemorrhagic side effects was assessed. If hemorrhagic findings were not detected, the injection was resumed. In addition, in cases showing hemorrhage in other organs, cases with fever without infection, or cases showing hypersensitivity reactions, urokinase injection was not conducted. This study was approved by the institutional review board in our hospital.
To patients under 70 years of age whose general condition was good except for neurological symptoms, 500,000 units of urokinase was administered intravenously in 30 minutes as the loading dose. Afterward, 50,000 units/hour (500,000/day) of urokinase was administered continuously during 10 hours for 5 days by use of drug injection pumps. For patients older than 70 years or in poor general condition, the loading dose was omitted.
Among the entire 214 patients, for 143 patients included in the retrospective analysis, the National Institutes of Health Stroke Scale (NIHSS) score was calculated on the basis of neurological tests reported in the patients' medical records. Safety was evaluated by the incidence of symptomatic cerebral hemorrhage and mortality. Symptomatic cerebral hemorrhage was defined as cases in which hemorrhagic transformation was shown in radiological findings and was associated with the consequent deterioration of neuropathy.
Statistical analysis was performed by using the Statistical Package for the Social Sciences (SPSS) version 16.0. Depending on the variables to be analyzed, partial t-test, chi-square test, or repeated-measure ANOVA was performed. Statistical significance was defined as p-values <0.05.
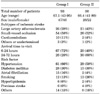
Among the entire 214 patients hospitalized for ischemic stroke, urokinase was administered to 93 patients (43.5%). The mean age of the patients was 67±13 years, and the number of males and females was 47 (50.5%) and 46 (49.5%), respectively. The median NIHSS value of the patients at the time of admission was 8 points (range, 5-34 points), and the average hospitalization period was 9.4 days (range, 5-34 days). As risk factors, hypertension was found in 61 patients (66%), which was most prevalent, followed by diabetes in 28 (30%), arterial fibrillation in 15 (16%), smoking in 12 (13%), and hyperlipidemia in 6 (6%). Regarding the subtype of stroke of 143 subjects according to the TOAST classification, small-vessel occlusion was found in 80 patients (55.9%), followed by large-artery atherosclerosis in 47 (32.9%), cardioembolism in 12 (8.3%), undetermined in 4 (2.8%), and other in 2 (2%) (Table 1).
There was a significant decrease in the NIHSS score at discharge in the urokinase treatment group (Group I). There was no significant difference in the NIHSS score before and after treatment in the non-urokinase-treatment group (Group II). The average NIHSS score (mean±SD) before and after treatment in the urokinase treatment group (Group I) was 4.8±2.2 and 3.8±1.9, respectively (p=0.02; Fig. 1). In Group II, the scores were 3.6±2.5 and 2.9±2.0 before and after treatment, respectively (p=0.1; Fig. 1). The NIHSS score of patients treated with urokinase within 24 hours of onset was significant (Group I), showing a, NIHSS score of 5.1±1.9 and 3.9±1.5, respectively (p=0.04) (Fig. 2, Table 2). In the case of early treatment within 24 hours, the change in the NIHSS score before and after treatment was significantly different.
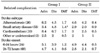
Complications developed during treatment in 17 of 93 patients (8.3%) in Group I. Among them, 2 patients showed intracranial hemorrhagic transformation; nonetheless, it was not fatal hemorrhage, and none of the patients died (Table 3). Eight patients developed nonfatal hemorrhage in other organs, and the trend of mild systemic hemorrhage was increased. In Group II, only 2 of 50 patients developed medical complications, which were unrelated to the treatment of stroke directly.
Intravenous injection of rt-PA is the only treatment for which effectiveness for acute ischemic stroke has been approved. This is based on the result of clinical research on rt-PA conducted by the National Institute of Neurological Disorders and Stroke (NINDS) in 1995, and rt-PA is the only drug approved by the US Food and Drug Administration that has to be injected within 3 hours after onset.3,4 Despite the proven effectiveness of rt-PA, the treatment time of rt-PA within 3 hours is the biggest limitation to rt-PA thrombolysis treatments, and many patients fail to arrive at hospitals within the eligible period and thus cannot be included among the treatment subjects. As is well known, the major purpose of treatment with rt-PA and intraarterial urokinase is the reperfusion of occluded blood vessels by immediate recanalization, because reperfusion through the recanalization of blood vessels is the most important prognostic factor assessing the success of treatment.5 Considering that thrombolytic agents not only recanalize occluded blood vessels immediately but also remove fibrins in blood plasma, this treatment can reduce blood viscosity and prevent the dissemination of thrombi, thus increasing the cerebral blood flow volume and preventing the expansion of the cerebral infarction. Hence, even if the appropriate time for rt-PA treatment has elapsed, the effectiveness of treatments with other thrombolytic agents for cases with remaining viable ischemic areas has been suggested, and many studies have been reported in terms of treatment in these subjects.6 As one such thrombolytic agent, intravenous injection of urokinase for patients later than 6 hours after onset has been used in several Korean hospitals.2
On the basis of the results of studies of the intravenous injection of urokinase to cerebral infarction patients conducted in Japan and Europe, the possibility of urokinase as a therapeutic for cerebral infarction was suggested, and it has been used in several hospitals in Korea. As opposed to intravenous rt-PA treatment or intraarterial urokinase treatment, intravenous urokinase treatment lacks selectivity and thus simultaneously reacts with not only plasminogen attached to thrombi but also plasminogen present in blood and exerts its thrombolytic action unselectively; its half-life is short, just a few minutes, and thus it is difficult to determine the appropriate dosages. Furthermore, because of the possibility of systemic side effects, it has been classified as grade 3 or grade C, which is a drug with insufficient data on effectiveness and safety in the guidelines for the treatment of acute ischemia of the American Stroke Association.7
In a previous Korean study on the effectiveness of intravenous injection of urokinase in cerebral infarction patients later than 6 hours after onset, the studies were conducted without a control group, and thus the clinical conclusion was unclear.2 In that study, for both the neurological evaluation and the functional evaluation after the administration of urokinase, the authors evaluated the level of the improvement of symptoms objectively by applying the European Stroke Scale (ESS) and the Barthel Index Score (BIS). The scores were significantly improved after the administration of urokinase from 7 days after onset, and at the time of discharge, noticeable improvement was shown. Those authors concluded that for patients who could not be treated with rt-PA intravenous injection or intraarterial urokinase injection owing to the restriction of the therapeutic time window, intravenous injection of urokinase is effective to some degree. This is later than the generally accepted treatment time based on the theory that the time window is not clear in humans and that in addition to ischemic duration, the factors determining improvement of cerebral infarction are regional cerebral blood flow and the level of development of collateral circulation. In addition, ischemic severity is also important. Thus, even if more than 6 hours has elapsed after onset, a role of thrombolytic agents could be anticipated.8-10
However, it was not clear whether the improvement in scores was actually due to the effect of urokinase or was the result of the natural course of the disease. In our study, the effect of the urokinase treatment group was directly compared with that of the control group, which is different from studies conducted until now. For the assessment of the treatment effect of urokinase, the most accurate method is comparison with a placebo control group. In real clinical practice, however, it is not possible to treat cerebral infarction patients with placebos only. Regarding the systemic treatment method of injecting thrombolytic agents intravenously. Reported that intravenous injection of urokinase was ineffective. Nevertheless, Mori et al.10 reported that when urokinase was injected intravenously within 6 hours of onset, the rate of reperfusion of blood vessels was 50%, which was markedly superior to the 17% of the control group. In our study, in the patient group administered urokinase within 24 hours of the onset of stroke, in comparison with the control group, clinical improvement was significant, which agrees with the action of thrombolytic agents reported by previous investigators. In other words, it could be considered that the effect of urokinase in terms of the increase in cerebral blood flow to ischemic brain tissues and prevention of the spread of cerebral thrombi was significant even in patients later than 6 hours after onset if urokinase is administered as early as possible after the onset of stroke. In the evaluation of the treatment of thrombolytic agents, one major concern is the hemorrhagic transformation of cerebral infarction. For the evaluation of the safety of the groups according to treatment methods, in brain computed tomography taken after treatments, the incidence of brain hemorrhage was examined. Only 2 patients of 93 patients in the urokinase treatment group showed minor hemorrhagic transformation. This value is noticeably lower than in previous studies.11 It is speculated that the method of the injection of urokinase used in our study as well as the control of doses reduced the incidence of hemorrhagic transformation. However, mild hemorrhage in the gastrointestinal tract and hemorrhage in the oral cavity that could be controlled readily by drugs were shown in 8 of 93 patients. It was pointed out that we should consider the several confounding variables, such as risk factors for cardiovascular diseases of the subjects. Also, the baseline comparison between the two groups was not sufficient because of differences in the NIHSS score at admission. Studies on long-term effects are required because only the short-term effect of urokinase was evaluated in this study.
In conclusion, if intravenous urokinase is administered within 24 hours, the rate of clinical improvement is better in acute stroke patients treated with intravenous injection of urokinase later than 6 hours after onset than in the control group. Because of the limitations of our study, it appears that broader and more comprehensive clinical studies are required in the future.
Figures and Tables
FIG. 1
Changes in the NIHSS score in the two groups. There was a significant decrease in the NIHSS score at discharge in the urokinase treatment group (Group I). There was no significant difference before and after treatment in Group II. *p<0.05. NIHSS: National Institutes of Health Stroke Scale, Group I: urokinase treatment group, Group II: non-urokinase-treatment group.
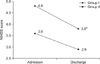
FIG. 2
Changes in the NIHSS score in Group I and Group II according to treatment start time. There was a significant decrease in the NIHSS score in group I with early treatment, no later than 24 hours after onset (6-24 hours). *p<0.05. NIHSS: National Institutes of Health Stroke Scale, Group I: urokinase treatment group, Group II: non-urokinase-treatment group.

References
1. Doh WB, Lee BC, Lee IH, Kim SM, Kwon KH. Safety and effect of continuous intravenous urokinase therapy in acute ischemic stroke (Open Clinical Trial). J Korean Neurol Assoc. 1999. 17:189–194.
2. Lee JH, Kim JS, Lee MC, Seo DC, Lee MS. A comparison study on therapeutic efficacy of urokinase vs. heparin in acute ischemic stroke. J Korean Neurol Assoc. 1994. 12:225–236.
3. Wahlgren N, Ahmed N, Dávalos A, Ford GA, Grond M, Hacke W, et al. SITS-MOST investigators. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet. 2007. 369:275–282.

4. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995. 333:1581–1587.
5. Chang DI, Yoon SS, Shin WC, Chung KC. Intravenous rt-PA fibrinolytic therapy in acute carotid territory ischemic stroke with severe neurologic deficits: the implication of arterial recanalization for stroke outcome. J Korean Neurol Assoc. 2003. 21:1–6.
6. Hacke W, Albers G, Al-Rawi Y, Bogousslavsky J, Davalos A, Eliasziw M, et al. DIAS Study Group. The Desmoteplase in Acute Ischemic Stroke Trial (DIAS): a phase II MRI-based 9-hour window acute stroke thrombolysis trial with intravenous desmoteplase. Stroke. 2005. 36:66–73.

7. Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. American Stroke Association Stroke Council. Clinical Cardiology Council. Cardiovascular Radiology and Intervention Council. Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007. 38:1655–1711.

8. von Kummer R, Hacke W. Safety and efficacy of intravenous tissue plasminogen activator and heparin in acute middle cerebral artery stroke. Stroke. 1992. 23:646–652.

9. Slivka A, Levy D. Natural history of progressive ischemic stroke in a population treated with heparin. Stroke. 1990. 21:1657–1662.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download