THE CASE: SEVERE RIGHT THIGH PAIN AND NUMBNESS AFTER ADJOINED LAMINAR FRACTURE
A 56-year-old man was admitted to the hospital because of traumatic brain injury after falling down some stairs. On admission to our emergency department, multiple bruises and laceration of the scalp were noted. On physical examination, he scored 13/15 on the Glasgow Coma Scale. A computed tomography (CT) scan showed cerebral epidural hematoma with a linear skull fracture at the right temporoparietal region. We undertook craniotomy and hematoma removal. After surgery, the patient's mental state recovered rapidly. About 1 month later, he was found to be neurologically intact. Two months later, he presented with lower back pain and right leg pain that had insidiously developed. As time passed, the patient's symptoms had become aggravated and he had difficulty walking despite analgesic medication. The pain radiated to the right L5 dermatome. The patient's capacity on a straight leg raise was diminished to 50 degrees on the right leg. Sensation was diminished in the right L5 and S1 dermatomes. Motor function was normal.
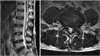
Magnetic resonance imaging (MRI) revealed a large cystic lesion on the lumbar spine (Fig. 1A, B). A CT scan showed a minimal fracture on the L4 lamina and adjoined L5 superior facet joint (Fig. 1C). The cyst was noted around the right L4-L5 facet joint, which ventrally compressed the dural sac and right-traversing L5 root. MRI revealed a well-defined, large-sized mass with variable intensity on T2-weighted images surrounding the L4-5 facet joint. The mass was enhanced after injection of gadolinium and revealed effusion in the interfacet joint, which suggested hemorrhage and contusion of the lesion.
DIAGNOSIS: GANGLION CYST ARISING FROM JOINT INSTABILITY
The patient underwent surgery through a posterior lumbar approach. A standard microsurgical hemi-partial laminectomy was performed. A large-sized, thick-walled capsulated mass was noted from the ruptured ligamentum flavum. The mass compressed adjacent muscles posteriorly and compressed the dural sac ventrally, which seemed to be connected to the facet joint capsule. The cystic mass was partially excised and cleaved by using a blade, Ronger, and Kerrison punch near the facet capsule. There was no connection to the disc or posterior longitudinal ligament. The radiating pain was alleviated immediately after the operation without neurological deficits. Photomicrographs showed thick collagenous fibrous tissue and myxoid degeneration without a synovial lining. Eight months later, the postoperative MRI scan showed remarkable regression of the cyst (Fig. 2).
Several terms for these cysts, including synovial cyst, ganglion cyst, and pseudocystic lesion have been used.1,2 A true cyst, a so-called "synovial cyst," has a synovial lining membrane, whereas a "ganglion cyst" has no synovial lining membrane. Here we presented a case of a ganglion cyst without a synovial lining membrane that seemed to be associated with facet joint instability possibly caused by a laminar fracture close to the facet joint.
Ganglion and synovial cysts can be classified by the presence of the synovial lining and communication with the facet joint; it is difficult to differentiate them clinically. Differentiation between the two types of cysts is only of histological value, because they share similar clinical and radiological characteristics. The pathogenesis of ganglion cysts is controversial. Posttraumatic degeneration of connective tissue and inflammation have been regarded as causes of these cysts.3 One of the causes of the formation of the ganglion cyst in this case seemed to be related to joint instability induced by laminar fracture close to the facet joint.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download