Abstract
The purpose of this study was to review the computed tomography (CT) features of thyroglossal duct cysts (TDCs) in children less than 11 years of age. A retrospective chart review was performed at Chonnam National University Hospital for the period of March 2005 to June 2011. CT scans of 16 patients having TDCs were evaluated for the following features: site of the mass, relationship to the midline, walls, margins, internal septa, rim enhancement, internal density, and the presence or absence of the thyroid gland. Of the 16 lesions, 8 (50%) were located in the midline and 12 (75%) were infrahyoid in location. Twelve (75%) of the 16 patients had well-circumscribed walls and peripheral rim enhancement. Internal septa were seen in four of the cysts, and all but one of the cysts demonstrated homogeneous or low-density attenuation. The most common CT findings of TDCs in children less than 11 years of age were a homogeneous or low-density lesion. TDCs in children under the age of 11 years were mostly located in the infrahyoid neck.
Thyroglossal duct cyst (TDC) is the most common congenital neck mass, accounting for 70% of all congenital neck lesions.1 In most circumstances, a clinical history and physical examination are sufficient to make a correct preoperative diagnosis.2 However, in some cases, the diagnosis of TDC is not clinically apparent. Therefore, preoperative imaging is important to confirm the diagnosis, to identify the presence of functioning thyroid tissue in the neck, and to detect any possibility of malignant change within the cyst.3
The radiologic features of TDCs have been described on computed tomography (CT) in adults,4,5 but there are no reports describing the appearance of TDCs on CT in children. The contrast-enhanced CT is the mainstay of initial assessment for palpable or symptomatic lesions in the neck.6 Therefore, we reviewed the computed tomographic features of TDCs in children under 11 years of age and documented their appearances.
After we obtained approval from the Institutional Review Board of Chonnam National University Hwasun Hospital, we performed a retrospective review to evaluate patients with a diagnosis of TDC at the Department of Otolaryngology-Head and Neck Surgery, Chonnam National University Hospital, for the period of March 2005 to June 2011. The inclusion criteria were age 10 years or younger and patients in whom TDC was diagnosed on the basis of final pathologic results after surgical excision. Patients who did not have a preoperative CT with enhancement or recurrent TDC were excluded. Sixteen patients aged less than 11 years and with a diagnosis of TDC were identified from the medical records.
The CT scans of the 16 children with TDC were retrospectively reviewed by one radiologist. The CT scans of the 16 patients were evaluated for the following features: site of the mass, relationship to the midline, walls, margins, internal septa, rim enhancement, internal density, and the presence or absence of the thyroid gland. The site was characterized in relation to the hyoid bone and midline. The low density ranged between 10 and 25 Hounsfield units.3,4
All patients underwent contrast-enhanced CT. Nonionic iodinated contrast agent (Ultravist®, Schering AG, Berlin, Germany) was intravenously administrated (a total of 100 ml, 2 ml/s) and the CT scans were obtained with two different multi-detector CT scanners (Light speed VCT and Sensation Cardiac 64). Scanning parameters were as follows: 120 kV, 200-250 mAs, pitch of 1.2, 0.5 s gantry rotation time, 40 mm detector coverage, 2.5-3.0 mm slice thickness, 2.5-3.0 mm interval. The CTDI for this protocol of acquisition ranged between 25 and 30 mGy and the DLP ranged between 705 and 1111 mGy×cm depending on the scanning range. We used tube current modulation to reduce the radiation dose.
All cases of TDCs were confirmed histopathologically. The criteria for diagnosing TDCs were based on the presence of ductular or cystic structures lined with cuboidal or columnar epithelium or nonkeratinizing stratified epithelium without epidermal appendages.
We studied 16 patients with TDCs. This group of children included nine (56.2%) males and seven (43.8%) females. The age of the patients ranged from 2 to 10 years with a mean of 6.4 years. The most common clinical presentation of the TDC was an anterior neck mass, which was observed in all patients. Preoperative evaluations included clinical history, physical examination, and radiologic procedures.
The radiological findings are summarized in Table 1 (Figs. 1-3). Of the 16 lesions, 8 (50%) were located in the midline and 8 were located just to one side of the midline (right=2, left=6). Twelve (75%) were infrahyoid in location, four (25%) were at the level of the hyoid, and none was suprahyoid. Twelve (75%) of 16 patients had well-circumscribed walls and peripheral rim enhancement. Internal septa were seen in four of the cysts. All but one of the cysts demonstrated homogeneous or low-density attenuation. The thyroid was normal in all cases.
There were no complications resulting from radiological or surgical intervention, and disease recurrence was not observed in any of the patients.
TDC is the most common congenital neck mass.1 TDCs can be located anywhere along the course of the thyroglossal duct from the base of the tongue to the thyroid gland. The location is in the midline or paramedian and is closely related to the hyoid bone.6,7 TDCs may be suprahyoid, infrahyoid, or at the level of the hyoid bone. Half of the TDCs in this study were midline and another half were slightly off midline. Contrary to previous reports,8,9 TDCs in this study were more located just to one side of the midline. It was previously reported that 20 to 25% of TDCs are suprahyoid in position, 15 to 50% occur at the level of the hyoid, and 25 to 65% are in the infrahyoid neck.10 However, in this study, none of TDCs was suprahyoid and most were in the infrahyoid neck (75%).
The typical CT appearance of a TDC is a low-density, usually unilocular but occasionally septated, well-circumscribed lesion with well-defined walls.3,4,6 Peripheral rim enhancement is sometimes observed on post-contrast images. In this study, 12 (75%) of 16 patients had well-circumscribed walls and peripheral rim enhancement, and the internal septa were seen in 4 (25%) of the cysts. The most common CT finding of the TDCs in this study was a homogeneous or low-density lesion (94%).
CT is an excellent modality for defining and localizing a congenital neck mass.5 This technique can provide useful information about the cyst location, size, and relation to surrounding structures.11 CT is superior for detecting calcification and, when contrast material is administered, the vascularity of lesions.12 CT can also prove to be a valuable aid in both the diagnosis and subsequent planned surgical intervention.5 Moreover, CT is usually more readily available, particularly in the emergent setting, and has quicker scan times. However, CT scans are not performed as frequently on children as on adults because children require sedation and limiting radiation exposure.3,13 In addition, CT is not helpful in differentiating TDCs from other neck masses in children.14
MRI is advantageous because it imparts no ionizing radiation exposure and evaluation of tissue signal intensity and enhancement characteristics allows confident assessment of many lesions.6,15 However, MRI requires sedation in infants and young children, which can be problematic. Therefore, CT or MRI of TDCs in children should be performed selectively.
Ultrasonography (US) should serve as the primary initial imaging modality in children for palpable masses and assessment of superficial glandular structures, such as the thyroid gland and salivary glands.6,16 The advantages of US include ready availability and quick interpretation, cost-effectiveness, lack of radiation exposure, and no requirement for sedation.6,9 US also provides valuable information used to identify cysts and thyroid glands. Huoh et al. demonstrated that US is equally accurate compared to MRI and CT with superiority over the other two modalities in cost and safety.17 Therefore, US was the preferred exam given its comparable accuracy, ease of administration, and lower cost.17
The Sistrunk operation is the most commonly used procedure for treating TDCs in children and is associated with very low recurrence rates.18 Morbidity is minimal and postoperative complications are generally minor. This operation requires little time for local excision and should be used when treating any masses that may be TDCs.19 In this study, there were no complications resulting from surgical intervention, and disease recurrence was not observed in any of the patients.
In conclusion, the most common CT finding of a TDC in children under the age of 11 years was a homogeneous or low-density lesion (94%). TDCs in children under the age of 11 years were mostly located in the infrahyoid neck (75%).
Figures and Tables
FIG. 1
Thyroglossal duct cyst in a 5-year-old female (case number 1). Axial contrast-enhanced CT scans show a homogeneous and low-density lesion in the anterior midline of the neck.
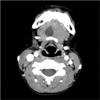
FIG. 2
Thyroglossal duct cyst in a 7-year-old male (case number 8). Axial contrast-enhanced CT scans show a well-circumscribed and septated lesion in the left side of the midline neck.
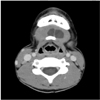
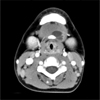
FIG. 3
Thyroglossal duct cyst in a 4-year-old male (case number 14). Axial contrast-enhanced CT scans show a peripheral rim enhancement of the lesion.
References
2. Davenport M. ABC of general surgery in children. Lumps and swellings of the head and neck. BMJ. 1996. 312:368–371.

3. Ahuja AT, Wong KT, King AD, Yuen EH. Imaging for thyroglossal duct cyst: the bare essentials. Clin Radiol. 2005. 60:141–148.

5. Ward RF, Selfe RW, St Louis L, Bowling D. Computed tomography and the thyroglossal duct cyst. Otolaryngol Head Neck Surg. 1986. 95:93–98.

7. Woo EK, Connor SE. Computed tomography and magnetic resonance imaging appearances of cystic lesions in the suprahyoid neck: a pictorial review. Dentomaxillofac Radiol. 2007. 36:451–458.

8. Wadsworth DT, Siegel MJ. Thyroglossal duct cysts: variability of sonographic findings. AJR Am J Roentgenol. 1994. 163:1475–1477.

9. Ahuja AT, King AD, Metreweli C. Sonographic evaluation of thyroglossal duct cysts in children. Clin Radiol. 2000. 55:770–774.

11. Byrd SE, Richardson M, Gill G, Lee AM. Computer-tomographic appearance of branchial cleft and thyroglossal duct cysts of the neck. Diagn Imaging. 1983. 52:301–312.
12. Koeller KK, Alamo L, Adair CF, Smirniotopoulos JG. Congenital cystic masses of the neck: radiologic-pathologic correlation. Radiographics. 1999. 19:121–146.
13. Lin ST, Tseng FY, Hsu CJ, Yeh TH, Chen YS. Thyroglossal duct cyst: a comparison between children and adults. Am J Otolaryngol. 2008. 29:83–87.

14. Lee DH, Jung SH, Yoon TM, Lee JK, Joo YE, Lim SC. Preoperative computed tomography of suspected thyroglossal duct cysts in children under 10-years-of-age. Int J Pediatr Otorhinolaryngol. 2012. [Epub ahead of print].

15. King AD, Ahuja AT, Mok CO, Metreweli C. MR imaging of thyroglossal duct cysts in adults. Clin Radiol. 1999. 54:304–308.

16. Gupta P, Maddalozzo J. Preoperative sonography in presumed thyroglossal duct cysts. Arch Otolaryngol Head Neck Surg. 2001. 127:200–202.

17. Huoh KC, Durr ML, Meyer AK, Rosbe KW. Comparison of imaging modalities in pediatric thyroglossal duct cysts. Laryngoscope. 2012. 122:1405–1408.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download