Abstract
We present a case of a false-positive anti-myeloperoxidase (MPO) antibody result on an ELISA in a patient with anti-thyroid microsomal antibody (TMA)-positive hypothyroidism. A 41-year-old woman presented with dyspnea on exertion. The initial evaluation revealed pericardial effusion associated with hypothyroidism. In addition, microscopic hematuria with normal renal function and positive cytoplasmic anti-neutrophil cytoplasmic antibodies (c-ANCA) on immunofluorescent assay were found. In further evaluation, elevated anti-TMA and MPO antibodies by ELISA. While no definite signs of vasculitis were present, the clinical state improved with thyroid hormone replacement and diuretics. Anti-MPO antibody was still positive in the follow-up tests, and microscopic hematuria persisted. On the basis of previous reports that thyroid peroxidase and MPO molecules contain cross-reactive epitopes that are exposed in denaturated molecules, we suggest that in a patient with anti-TMA-positive hypothyroidism, anti-MPO antibody might also be positive on ELISA without clinical signs of vasculitis.
Anti-neutrophil cytoplasmic antibody (ANCA) is a useful autoantibody in the diagnosis of idiopathic small-vessel vasculitides (SVV). Its target antigens include proteinase-3 (PR3), myeloperoxidase (MPO), elastase, lactoferrin, lactoperoxidase, lysozyme, azurocidin, and cathepsin G. Anti-MPO is particularly known as an important marker for the diagnosis of vasculitis, such as idiopathic crescentic glomerulonephritis and microscopic polyarteritis nodosa (MPA).1 The ANCA tests include the indirect immunofluorescence assay (IFA) in which neutrophils are fixed on the slide (ANCA IFA) and the enzyme-linked immunosorbent assay (ELISA) using individual antigens (i.e., anti-MPO ELISA, anti-PR3 ELISA).
A previous case report presented an anti-MPO antibody-positive patient who was also positive for the anti-thyroid microsomal antibody (anti-TMA).2 A recent study reported that thyroid peroxidase (TPO) is a major antigen of anti-TMA.3 According to the observation of considerable similarity in the peptide sequences of TPO and MPO,4 a possible cross-reactivity between the anti-TPO antibody and the anti-MPO antibody was studied. That study used synthetic peptides for MPO and TPO, and found that the denaturation exposed cross-reactive epitopes on those antigens, which might lead to a false-positive result in the solid phase of the ELISA assay.5 There was a case report in which a patient with anti-TPO-positive thyrotoxicosis also had anti-MPO-positive vasculitis,6 but false-positivity has not been reported in Korea. Here we present a case of a false-positive anti-MPO ELISA result in a patient with anti-TPO-positive hypothyroidism.
Patient: Age 41, female
Chief complaints: Dyspnea and abdominal pain
Present medical history: Epigastric pain and dyspnea had developed 2 days previously, which led her to visit a neighborhood clinic, where pleural and pericardial effusion were confirmed by abdominal CT. She was then transferred to our hospital.
Past medical history: No specific findings.
Family history: No specific findings.
Findings on physical examination: Vital signs at the time of the visit were as follows: blood pressure, 91/65 mmHg; heart rate, 97/min; body temperature, 36.5℃; and respiratory rate, 16/min. The patient appeared acutely ill, with presentation of a swollen face and bilateral jugular venous dilatation. Heart sounds were reduced, and edema was present in both legs.
Laboratory findings: A routine blood test at the initial visit revealed a white blood cell (WBC) count of 13,030/uL (normal: 4,800-10,800/uL), hemoglobin of 13.6 g/dL (normal: 13-18 g/dL), and platelets of 313,000/uL (normal: 130,000-400,000/uL). C-reactive protein (CRP) was 3.37 mg/dL (normal: <0.5 mg/dL) by immunoturbidimetry. Serum chemistry analysis showed blood urea nitrogen (BUN) was 31.0 mg/dL (normal: 6-20 mg/dL), creatinine was 0.61 mg/dL (normal: 0.9-1.5 mg/dL), Na was 135 mmol/L (normal: 136-146 mmol/L), and K was 4.3 mmol/L (normal: 3.3-5.1 mmol/L). The following were found to be elevated: GOT, 56 U/L (normal: <37 U/L); GPT, 56 U/L (normal: <41 U/L); ALP, 108 IU/L (normal: 35-129 IU/L); and GGT, 128 U/L (normal: 8-61 U/L). Total protein was 6.5 g/dL (normal: 6.7-8.3 g/dL), and albumin was 3.5 g/dL (normal: 3.2-4.8 g/dL). The urinalysis results were as follows: SG, 1.020 (normal: 1.003-1.03); pH 5.5 (normal: 4.5-8.0); urine protein (-); urine glucose (±); red blood cell (RBC) count, many/HPF; and WBC, many/HPF. Other readings included Pro-BNP of 10,550 pg/mL (normal: 0-194 pg/mL), CK-MB of 6.4 ng/ mL (normal: 0-3.6 ng/mL), and cardiac troponin I of 5.24 ng/mL (normal: 0-0.1 ng/mL).
Radiological findings: Simple chest X-ray showed an increased cardiothoracic ratio. Echocardiography confirmed pericardial effusion, and the inferior vena cava was dilated. Abdominal ultrasonography also showed findings of dilatation of the hepatic vein and the inferior vena cava, along with a small amount of ascites. There was no sign of hepatic enlargement. Thyroid ultrasonography revealed diffuse bilateral goiter and benign nodules.
Treatment and progress: The results of the post-admission thyroid function test were as follows: TSH, 9.1 uIU/mL (normal: 0.3-4 uIU/mL); free T4, 1.4 ng/dL (normal: 0.8-1.8 ng/dL); T3, 0.4 ng/mL (normal: 0.6-1.9 ng/mL); and anti-TMA, 403.2 U/mL (normal: 0-60 U/mL). The patient was ANA (antinuclear antibody)-negative and ANCA IFA-positive [cytoplasmic pattern (C-ANCA), titer 1:20]. Anti-MPO ELISA and anti-PR3 ELISA titers were 449 AAU (normal: 0-150 AAU) and 56 AAU (normal: 0-150 AAU), respectively. Renal function was normal with a BUN of 14.8 mg/dL and a creatinine level of 0.62 mg/dL. The pericardial and pleural effusion fluid was thought to be related to hypothyroidism, and levothyroxine treatment was started (0.025 mg for the 1st week and 0.05 mg thereafter for 1 month). Diuretics (torsemide 20 mg and spironolactone 100 mg) were given upon admission for treatment of heart failure, and dyspnea improved. Echocardiography performed 2 weeks later showed decrease in the pericardial effusion fluid. Urinalysis performed at the time of discharge showed RBC was 0-1/HPF, and the AST, ALP, CRP, and cTnI levels were reduced to normal.
Urinalysis at 1 month after discharge revealed RBC was 5-10/HPF, with persistent microscopic findings of hematuria. Other results included anti-MPO ELISA, 554 AAU; anti-TMA, 1046.2 U/mL; TSH, 0.03 uIU/mL; free T4, 5.3 ng/dL; and T3, 2.9 ng/mL. Upon the findings, levothyroxine was discontinued.
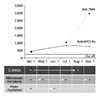
At 3 months after discharge, urine RBC was 3-5/HPF. ANCA IFA was negative, with an anti-MPO ELISA titer of 849 AAU. Urinalysis at 11 months showed RBC was 3-5/HPF, spot urine protein-to-creatinine ratio was 0.09, and anti-MPO ELISA was 639 AAU. Anti-TMA antibody was continuously elevated at 1236.3 U/mL (Fig. 1). Thyroid function was maintained normal with TSH of 4.3 uIU/mL, free T4 of 1.5 ng/dL, and T3 of 1.0 ng/mL. At 1 year after discharge, the patient has not shown any specific symptoms without drug treatment, and is still being closely monitored.
ANCA is an autoimmune antibody that reacts to the cytoplasmic antigens in the neutrophils and monocytes.7 Anti-MPO, a subtype of ANCA, is positive in patients with vasculitis (e.g., microscopic polyarteritis nodosa, Churg-Strauss syndrome)8 and has been used as a diagnostic marker of such disease. TPO is known as a major antigen of TMA, and anti-TMA is a main autoantibody involved in autoimmune thyroiditis. There is a case report of a patient who was both anti-MPO- and anti-TPO-positive and had both vasculitis and thyroid disease.6 The patient had Grave's disease and anti-MPO-positive glomerulonephritis.9 Whereas our patient in the present case was anti-TMA- and anti-MPO-positive and had hypothyroidism, she showed no symptoms leading to a clinical suspicion of vasculitis, despite the steadily elevated anti-MPO level. There were findings of hypothyroidism on the thyroid function test, and she was anti-TMA-positive. She also had positive results on the ANCA IFA and anti-MPO ELISA. The microscopic hematuria persisted, but without clinical symptoms of vasculitis. The anti-MPO ELISA continued to be positive. Later, negative seroconversion of ANCA IFA was observed, but the anti-MPO ELISA remained positive. Anti-MPO and anti-TMA were continuously positive throughout the outpatient monitoring over about 1 year, but no clinical findings conforming to vasculitis were found, except for the microscopic hematuria. Because renal biopsy was not performed initially when the microscopic hematuria and the positivity for ANCA and anti-MPO antibody was observed, we could not determine whether the microscopic hematuria was caused by a glomerular lesion accompanied by vascular changes. Nonetheless, normal renal function was maintained without proteinuria, and there were no findings to suggest vasculitis in other organs. Therefore, the possibility of vasculitis causing the hematuria appeared to be low. Furthermore, the initial ANCA IFA positivity was a C-ANCA pattern and might be unrelated to anti-MPO, which presents a perinuclear pattern (P-ANCA). TPO is known as the major antigen of TMA,3 and there are reports of peptide sequence similarities between TPO and MPO.4 In one study, anti-TPO and anti-MPO obtained from a patient with vasculitis and a patient with autoimmune thyroiditis, respectively, were put into reaction to the native TPO and MPO antigens. The anti-TPO reacted to the native TPO antigen but not to the native MPO antigen. Likewise, the anti-MPO reacted to the native MPO antigen but not to the native TPO antigen. Notably, the two antibodies showed cross-reactivity when the synthetic TPO and MPO antigens were used. The reported peptide sequence homology between TPO and MPO was up to 88%. During synthesis, the antibodies obtain a linear structure while the original peptide sequences are maintained. This configurational change exposes the cross-reactive epitopes.5 The absence of cross-reactivity to the native antigens is attributable to 1) the native spatial configuration of the antigens in which the cross-reactive epitopes are not well exposed and 2) the possibility of the native configuration working as an epitope itself. This was confirmed by another study in which anti-MPO reacted to native MPO but not to denaturated MPO.10 In ANCA IFA, patient serum is added to the neutrophils isolated from healthy donors. The fluorescent antigens are added, and the presence of ANCA is determined by using fluorescence microscopy. In other words, patient serum is added to native antigens. In ELISA, patient serum is added to the solid phase to which the MPO-specific antigens are attached. Then, the presence of ANCA is determined by absorbance and subsequently quantified. Here, unlike in the immunofluorescence, patient serum is added to synthetic antigens. Use of antigens that have epitopes common to both MPO and TPO in ELISA might cause cross-reaction of anti-TPO to synthetic MPO. In this case, anti-TPO positivity might result in anti-MPO positivity. In the present case, the patient was negative for the ANCA IFA but positive for the anti-MPO ELISA, which suggests the possibility of false anti-MPO positivity. Because we did not perform a renal biopsy, however, it remains uncertain whether a minor glomerular lesion was present.
In conclusion, when a patient is ANCA negative on IFA and is without clinical signs of vasculitis, but anti-MPO positive on ELISA, one should consider a possible cross-reactivity of MPO to thyroid autoantibody. In this case, it may be necessary to test thyroid function and autoantibody to investigate a possible false ELISA positivity.
Figures and Tables
References
1. Falk RJ, Jennette JC. Anti-neutrophil cytoplasmic autoantibodies with specificity for myeloperoxidase in patients with systemic vasculitis and idiopathic necrotizing and crescentic glomerulonephritis. N Engl J Med. 1988. 318:1651–1657.

2. Gaskin G, Ryan TJ, Rees AJ, Pusey CD. Antimyelo-peroxidase antibody in vasculitis: relationaship to. ANCA and clinical diagnosis. APMIS. 1990. 88:Suppl 19. 33.
3. Kotani T, Umeki K, Matsunaga S, Kato E, Ohtaki S. Detection of autoantibodies to thyroid peroxidase in autoimmune thyroid diseases by micro-ELISA and immunoblotting. J Clin Endocrinol Metab. 1986. 62:928–933.

4. Kimura S, Hong YS, Kotani T, Ohtaki S, Kikkawa F. Structure of the human thyroid peroxidase gene: comparison and relationship to the human myeloperoxidase gene. Biochemistry. 1989. 28:4481–4489.

5. Haapala AM, Hyöty H, Parkkonen P, Mustonen J, Soppi E. Antibody reactivity against thyroid peroxidase and myeloperoxidase in autoimmune thyroiditis and systemic vasculitis. Scand J Immunol. 1997. 46:78–85.

6. Lee SS, Lawton JWM. Co-existence of anti-myeloperoxidase and antithyroid peroxidase auto antibodies in two patients. J Hong kong Med Assoc. 1994. 46:138–141.
7. Radice A, Sinico RA. Antineutrophil cytoplasmic antibodies (ANCA). Autoimmunity. 2005. 38:93–103.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download