Abstract
The Thrombolysis in Myocardial Infarction (TIMI) risk score (TRS) has proven value in predicting prognosis in unstable angina/non ST-elevation myocardial infarction (NSTEMI) as well as in ST-elevation myocardial infarction. The TRS system has little implication, however, in the extent of myocardial damage in high-risk patients with NSTEMI. A total of 1621 patients (63.6±12.2 years; 1043 males) with NSTEMI were enrolled in the Korea Acute Myocardial Infarction Registry (KAMIR). We analyzed the risk for major adverse cardiac events (MACE) during a 6-month follow-up period. The TRS system showed good correlation with MACE for patients in the low and intermediate groups but had poor correlation when the high-risk group was included (p=0.128). The MACE rate was 3.8% for TRS 1, 9.4% for TRS 2, 10.7% for TRS 3, and 12.3% for TRS 4 (HR=1.29, p=0.026). Among the biomarkers and clinical risk factors, elevated N-terminal pro-brain natriuretic peptide (NT-proBNP) (HR=2.61, p=0.001) and Killip class above III showed good correlation with MACE (HR=0.302, p<0.001). Therefore, we revised an alternative clinical scoring system by including these two variables that reflect left ventricular dysfunction: age > 65 years, history of ischemic heart disease, Killip class above III, and elevated pro-BNP levels above the 75th percentile. This modified scoring system, when tested for validity, showed good predictive value for MACE (HR=1.64, p<0.001). Compared with the traditional TRS, the novel alternative scoring system based on age, history of ischemic heart disease, Killip class, and NT-proBNP showed a better predictive value for 6-month MACE in high-risk patients with NSTEMI.
In patients with non-ST-elevation acute coronary syndrome (ACS), early risk stratification is of critical importance, because the benefit of newer and more aggressive treatment strategies seems to be proportional to the risk of adverse clinical events.1-3 Different scores capable of early risk stratification have been developed on the basis of initial clinical history, electrocardiogram, and laboratory tests. Among others, the Thrombolysis in Myocardial Infarction (TIMI) risk score (TRS) is the most validated and the most extensively used in patients with non-ST-elevation ACS.4 However, this score does not utilize N-terminal pro-brain natriuretic peptide (NT-proBNP) or Killip class from the candidate variables. The baseline measure of NT-proBNP has been identified as a powerful long-term determinant of cardiac events,5-8 and Killip class at presentation has invariably been a component of previous scores,9-12 emphasizing the importance of the clinical examination for signs of heart failure at the time of initial presentation.
Accordingly, we hypothesized that incorporating NT-proBNP and Killip class into the TRS would enhance this score's ability to predict events. The aims of the present study were therefore to analyze the prognostic value of the TRS in patients with non-ST-elevation myocardial infarction (NSTEMI) and to construct, if possible, a new predictive model based on the TRS by including Killip class (≥ III) and NT-proBNP to increase prognostic efficacy for patients at high risk of adverse cardiac outcomes.
To this end, data from the Korea Acute Myocardial Infarction Registry (KAMIR), the largest multicenter registry in Korea of AMI to date, were utilized for score derivation. The KAMIR is a population-based, multicenter data collection registry evaluating treatment practice and outcomes that was launched in November 2005. The registry includes 50 community and teaching hospitals that enroll more than 5000 patients annually. As of August 2007, the registry contained data on 12,634 patients. The KAMIR is supported by a research grant from the Korean Circulation Society in commemoration of its 50th Anniversary and aims to improve patient care by providing a greater understanding of patient management and outcomes in the rapidly evolving field of AMI treatment.
The study population consisted of 1261 consecutive patients with NSTEMI registered in the KAMIR database between January 2006 and December 2007. Patients of any age with NSTEMI were enrolled. The inclusion criteria were a history of chest pain at rest or other symptoms suggestive of an acute coronary syndrome, with the most recent episode occurring within 24 hours of admission. This could be associated with elevated levels of biomarkers of myocardial damage with or without ST or T wave changes on the electrocardiogram suggestive of myocardial ischemia. The biomarkers used were cardiac troponin I or T with a threshold for positivity of ≥99th percentile of the upper reference limit. After clinical evaluation, the patients underwent determination of NT-proBNP at the emergency department (with at least one blood sample more than 6 hours after the onset of pain).
The TRS was calculated from the initial clinical history, electrocardiogram, and laboratory values collected on admission. A retrospective calculation of the TRS was made for each patient. This yielded between 0 and 7 possible points according to the simple mathematical sum of each of the following characteristics: age of 65 years, existence of 3 or more classical risk factors (hypertension, hypercholesterolemia, diabetes mellitus, smoking, or family history of ischemic heart disease), previous significant coronary artery disease (stenosis of ≥50%), aspirin consumption in the previous 7 days, at least 2 episodes of angina in the previous 24 hours, elevation of cardiac necrosis markers, and ST deviations of at least 0.5 mm.4
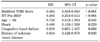
The Modified TIMI Risk Score (MTRS) was constructed to include markers of heart failure such as Killip class and NT-proBNP. This novel score was therefore made up of 4 simpler variables, with a scoring system as follows:
The total score was still a simple mathematical sum but now ranged from 0 to 4. Based on the total risk score, patients were classified into risk categories of low risk (MTRS=0-1), intermediate risk (MTRS=2-3), and high risk (MTRS=4).
Clinical follow-up was done 6 months after discharge by personal interview or telephone to record data relating to the control of risk factors, adherence to treatment, functional class, and appearance of symptoms or complications. The incidence of the combined event of cardiovascular death, infarction, and need for revascularization was recorded during the follow-up period.
The log-rank test was performed for the Kaplan-Meier probability estimates. The relationship between NT-proBNP (either continuous or dichotomous) and the outcome was adjusted for the effects of Killip classes and TRS (either continuous or dichotomous) with the use of stepwise multivariate logistic regression.
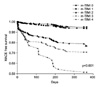
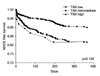
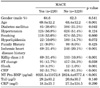
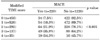
The baseline clinical and laboratory characteristics of the MACE and no MACE groups are summarized in Table 1. Patients with MACE were older and were more likely to have diabetes, a history of ischemic heart disease, a Killip class ≥3, ST-segment change, cardiogenic shock, heart failure, and higher NT-ProBNP levels. Among the biomarkers, elevated NT-proBNP levels above the 75th percentile had the best predictive value for MACE (HR=2.61, p=0.001) independently of other risk factors. Among the clinical risk factors, Killip class above III and the presence of heart failure or cardiogenic shock showed good correlation with MACE (p<0.001, p<0.001, p=0.001, respectively). The TRS system had good correlation with MACE for patients in the low and intermediate groups (Table 2, Fig. 1). The MTRS, which included Killip class ≥3 and NT-ProBNP levels, showed good predictive values for MACE (p<0.001) (Table 3, Fig. 2). Also, the MTRS showed excellent discriminative properties among other risk factors and laboratory indices except for troponin-I and hs-CRP levels (Table 4). Multivariate analysis for predictions of MACE revealed NT-proBNP as the best prognostic indicator (HR=0.394, p<0.001) (Table 5).
The principal findings of the present study, in which a powerful new cardiac risk score was created and validated, are as follows. First, in patients with acute NSTEMI, 6-month cardiac events can be accurately predicted by using four clinical and laboratory variables readily available at the time of presentation. Second, baseline NT-proBNP and Killip class are powerful predictive variables of mortality and should be incorporated into risk models. Third, with the use of this prognostic score, three levels of risk stratification can be created that identify patients with NSTEMI. Finally, the current risk score, when validated against the original TRS, provides more discriminatory accuracy for 6-month clinical outcome, especially in a high-risk population. Accordingly, use of this alternative risk scoring system enables identification of patients with a poor long-term prognosis in whom close monitoring and intensive therapy may be beneficial.
Previous risk scoring systems have been proposed for estimating in-hospital risk after admission for ACS,4,10,16 including risk models developed from large clinical trials or registry data by the TIMI clinical trials group.4,10 All these scores were developed for short-term prognosis: events at 14 days for the TRS and at 30 days for the PURSUIT risk score. However, a significant proportion of adverse events in patients with non-ST-elevation ACS occur after the first 30 days, and it is not known whether these risk scores can also predict the development of MACE. On the other hand, it has been shown that an early invasive strategy has a prognostic benefit in long-term clinical follow-up.17
The TRS is a scoring system with 7 risk variables in patients with unstable angina or NSTEMI.4 This scale was created by retrospectively applying multivariate statistic models to the populations of two large clinical trials with heparins: TIMI 11B2 and Efficacy and Safety of Subcutaneous Enoxaparin in Unstable Angina and Non-Q-wave Myocardial Infarction (ESSENCE).18 It has since been validated in various studies such as CURE, PRISM-PLUS, and TACTICS-TIMI 18,3,19 in which it has proved to be capable of predicting both the prognosis and the response to new therapies in both short- and long-term clinical follow-up. Nevertheless, there is little information on its applicability to daily clinical practice beyond the trials in which it was developed in selected populations.13 Because of the low incidence of signs of heart failure on admission in the population of the TIMI 11B trial used for the development of the TRS, variables such as Killip class or NT-proBNP were not included in the model. This is an important limitation, however, especially because the occurrence of heart failure is much more frequent in the real world than in selected patients from clinical trials, and its prognostic value is well established.16,20,21 The GRACE score, which was based on a large registry of patients across the entire spectrum of acute coronary syndromes, shares many variables with previous mortality models.22,23 However, heart failure at presentation, expressed as Killip class, constituted a greater proportion of the predictive information in this model than in previous clinical trial models. This may be partially explained by the fact that these patients were not excluded from the GRACE database. The other reason for the findings presented above may come from the fact that in contrast with other well-established factors included in TRS, NT-proBNP has an advantage in detecting long-term consequences of myocardial infarction such as left ventricular dysfunction or dilatation in addition to estimation of the amount of infarct size.24 Previous studies demonstrated that NT-proBNP levels obtained in the first days after the onset of symptoms are predictive of short- and long-term mortality in patients with ACS.6-8,25 Recently, Bazzino et al26 and Grabowski et al27 reported a highly significant additive value of baseline NT-proBNP concentrations for 6-month mortality assessed with common risk scales for non-ST-elevation ACS: TRS and the American College of Cardiology/American Heart Association classification. Our results are consistent with those of Bazzino's group, who showed that baseline NT-proBNP added prognostic information to risk scores for non-ST-elevation ACS.26,27
Systematic risk assessment for each patient provides decisions regarding therapeutic interventions, triage to additional hospital care, and allocation of clinical resources. In this observational study, the MTRS was confirmed as an important long-term prognostic predictor in patients with NSTEMI; it establishes a risk curve ranging from a low to intermediate probability of cardiac events. Furthermore, we have obtained a new modified scale that, with the addition of presence of Killip class and NT-pro BNP to the other variables, increases prognostic capacity at no expense to the simplicity of the model. Our results also demonstrated that the long-term benefit of myocardial revascularization performed during initial hospital admission was only clearly observed in high-risk patients. These results agree with those of the FRISC II and TACTICS-TIMI 18 studies, which established the benefit of an early invasive strategy, but only for high-risk patients.1,28,29 This, in part, could be explained by the constitution of the patient population in our study, most of whom already had a few risk factors of TRS at presentation, i.e., electrocardiogram changes and positive troponins. In this study, the diagnosis between unstable angina pectoris and acute myocardial infarction was usually made by the increased levels of serum troponins. Accordingly, the proportion of patients with intermediate to high-risk features may have been a lot higher compared with the patients included in the original TIMI 11B trial.
The present study confirms the capacity of the TRS for discriminating the probability of events in patients with NSTEMI. In fact, the 6-month MACE ranged from 12.4% for a score of 0 to 2 to 23.1% for high-risk patients (score of 5 or above). However, in our analysis, the prognostic value was less pronounced in high-risk patients, with 21.5% of events at 6 months for the intermediate TRS and 23.1% for the highest. The inclusion of Killip class and NT-proBNP as variables in the scale improved prognostic capacity. The excellent result of integrating these 2 variables may lie in the fact that they predict different complications. The TRS was developed to evaluate the risk of ischemic episodes (including myocardial infarction and the need for revascularization in the combined event), whereas the factors predicting mortality are usually related to left ventricular dysfunction (worse Killip class, NT-proBNP, etc). The MTRS may well be closer to real-world practice than previous studies limited to clinical trial populations or single-region registries. As such, we believe that clinicians will find greater confidence in its applicability in their practices. The KAMIR is the largest national registry study in Korea to include the entire spectrum of patients with AMI. It is designed to be representative of regional communities and uses standardized criteria for defining AMI and hospital outcomes and quality control and audit measures.
In conclusion, the MTRS, 6-month post-discharge prediction model, is a simple, robust tool for predicting death in patients with NSTEMI and has very good discriminative capacity. This risk assessment tool is likely to be clinically useful in the triage and management of patients eligible for early invasive therapy and may also serve as a valuable aid in clinical research for patients with NSTEMI.
A limitation of our study was the relatively small number of participants. Due to the low mortality rate in patients with TRS <4, incremental information offered by BNP measurement was practically limited to patients with high TRS. Another reason limiting the statistical analysis was the absence of ejection fraction in the multivariate model. However, our aim was to investigate the influence of Killip class and NT-proBNP on prognostic information obtained from clinical variables available on admission. Third, there may be unmeasured variables that would have provided further prognostic and longer-term information. The aim of this model, however, was to provide insight into factors associated with increased risk for 6-month clinical outcomes. The goal of achieving simplicity and ease of use must be balanced against completeness and accuracy. Finally, it must be remembered that this was an observational, registry study, and the results should be extrapolated carefully to other environments with different populations and clinical management schemes. Further studies would be warranted for verification of this new score system.
Figures and Tables
FIG. 2
Major adverse cardiac event (MACE)-free survival according to the Modified TIMI Risk Score system.
ACKNOWLEDGEMENTS
This study was performed with the support of the Korean Circulation Society (KCS) in commemoration of its 50th Anniversary and the Korea Healthcare technology R&D project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A084869).
References
1. Cannon CP, Weintraub WS, Demopoulos LA, Vicari R, Frey MJ, Lakkis N, et al. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med. 2001. 344:1879–1887.

2. Antman EM, Cohen M, McCabe C, Goodman SG, Murphy SA, Braunwald E. TIMI 11B and ESSENCE Investigators. Enoxaparin is superior to unfractionated heparin for preventing clinical events at 1-year follow-up of TIMI 11B and ESSENCE. Eur Heart J. 2002. 23:308–314.

3. Morrow DA, Antman EM, Snapinn SM, McCabe CH, Theroux P, Braunwald E. An integrated clinical approach to predicting the benefit of tirofiban in non-ST elevation acute coronary syndromes. Application of the TIMI risk score for UA/NSTEMI in PRISM-PLUS. Eur Heart J. 2002. 23:223–229.

4. Antman EM, Cohen M, Bernink PJ, McCabe CH, Horacek T, Papuchis G, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000. 284:835–842.

5. Omland T, Persson A, Ng L, O'Brien R, Karlsson T, Herlitz J, et al. N-terminal pro-B-type natriuretic peptide and long-term mortality in acute coronary syndromes. Circulation. 2002. 106:2913–2918.

6. Morrow DA, de Lemos JA, Sabatine MS, Murphy SA, Demopoulos LA, DiBattiste PM, et al. Evaluation of B-type natriuretic peptide for risk assessment in unstable angina/non-ST-elevation myocardial infarction: B-type natriuretic peptide and prognosis in TACTICS-TIMI 18. J Am Coll Cardiol. 2003. 41:1264–1272.

7. de Lemos JA, Morrow DA, Bentley JH, Omland T, Sabatine MS, McCabe CH, et al. The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N Engl J Med. 2001. 345:1014–1021.

8. Galvani M, Ottani F, Oltrona L, Ardissino D, Gensini GF, Maggioni AP, et al. N-terminal pro-brain natriuretic peptide on admission has prognostic value across the whole spectrum of acute coronary syndromes. Circulation. 2004. 110:128–134.

9. Lee KL, Woodlief LH, Topol EJ, Weaver WD, Betriu A, Col J, et al. Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction. Results from an international trial of 41,021 patients. GUSTO-I Investigators. Circulation. 1995. 91:1659–1668.

10. Morrow DA, Antman EM, Charlesworth A, Cairns R, Murphy SA, de Lemos JA, et al. TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation: an intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation. 2000. 102:2031–2037.

11. Addala S, Grines CL, Dixon SR, Stone GW, Boura JA, Ochoa AB, et al. Predicting mortality in patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention (PAMI risk score). Am J Cardiol. 2004. 93:629–632.

12. De Luca G, Suryapranata H, van't Hof AW, de Boer MJ, Hoorntje JC, Dambrink JH, et al. Prognostic assessment of patients with acute myocardial infarction treated with primary angioplasty: implications for early discharge. Circulation. 2004. 109:2737–2743.

13. Scirica BM, Cannon CP, Antman EM, Murphy SA, Morrow DA, Sabatine MS, et al. Validation of the thrombolysis in myocardial infarction (TIMI) risk score for unstable angina pectoris and non-ST-elevation myocardial infarction in the TIMI III registry. Am J Cardiol. 2002. 90:303–305.

14. Peters RJ, Mehta SR, Fox KA, Zhao F, Lewis BS, Kopecky SL, et al. Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: observations from the Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) study. Circulation. 2003. 108:1682–1687.

15. Ohman EM, Granger CB, Harrington RA, Lee KL. Risk stratification and therapeutic decision making in acute coronary syndromes. JAMA. 2000. 284:876–878.

16. Boersma E, Pieper KS, Steyerberg EW, Wilcox RG, Chang WC, Lee KL, et al. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation Results from an international trial of 9461 patients. The PURSUIT Investigators. Circulation. 2000. 101:2557–2567.

17. Invasive compared with non-invasive treatment in unstable coronary-artery disease: FRISC II prospective randomised multicentre study. FRagmin and Fast Revascularisation during InStability in Coronary artery disease Investigators. Lancet. 1999. 354:708–715.
18. Cohen M, Demers C, Gurfinkel EP, Turpie AG, Fromell GJ, Goodman S, et al. Low-molecular-weight heparins in non-ST-segment elevation ischemia: the ESSENCE trial. Efficacy and Safety of Subcutaneous Enoxaparin versus intravenous unfractionated heparin, in non-Q-wave Coronary Events. Am J Cardiol. 1998. 82:19L–24L.
19. Budaj A, Yusuf S, Mehta SR, Fox KA, Tognoni G, Zhao F, et al. Benefit of clopidogrel in patients with acute coronary syndromes without ST-segment elevation in various risk groups. Circulation. 2002. 106:1622–1626.

20. Malmberg K, Yusuf S, Gerstein HC, Brown J, Zhao F, Hunt D, et al. Impact of diabetes on long-term prognosis in patients with unstable angina and non-Q-wave myocardial infarction: results of the OASIS (Organization to Assess Strategies for Ischemic Syndromes) Registry. Circulation. 2000. 102:1014–1019.

21. McGuire DK, Emanuelsson H, Granger CB, Magnus Ohman E, Moliterno DJ, White HD, et al. Influence of diabetes mellitus on clinical outcomes across the spectrum of acute coronary syndromes. Findings from the GUSTO-IIb study. GUSTO IIb Investigators. Eur Heart J. 2000. 21:1750–1758.

22. Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003. 163:2345–2353.

23. Eagle KA, Lim MJ, Dabbous OH, Pieper KS, Goldberg RJ, Van de Werf F, et al. A validated prediction model for all forms of acute coronary syndrome: estimating the risk of 6-month postdischarge death in an international registry. JAMA. 2004. 291:2727–2733.

24. Wiviott SD, de Lemos JA, Morrow DA. Pathophysiology, prognostic significance and clinical utility of B-type natriuretic peptide in acute coronary syndromes. Clin Chim Acta. 2004. 346:119–128.

25. Omland T, Persson A, Ng L, O'Brien R, Karlsson T, Herlitz J, et al. N-terminal pro-B-type natriuretic peptide and long-term mortality in acute coronary syndromes. Circulation. 2002. 106:2913–2918.

26. Bazzino O, Fuselli JJ, Botto F, Perez De Arenaza D, Bahit C, Dadone J. PACS group of investigators. Relative value of N-terminal probrain natriuretic peptide, TIMI risk score, ACC/AHA prognostic classification and other risk markers in patients with non-ST-elevation acute coronary syndromes. Eur Heart J. 2004. 25:859–866.

27. Grabowski M, Filipiak KJ, Malek LA, Karpinski G, Huczek Z, Stolarz P, et al. Admission B-type natriuretic peptide assessment improves early risk stratification by Killip classes and TIMI risk score in patients with acute ST elevation myocardial infarction treated with primary angioplasty. Int J Cardiol. 2007. 115:386–390.

28. Cannon CP, Weintraub WS, Demopoulos LA, Vicari R, Frey MJ, Lakkis N, et al. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med. 2001. 344:1879–1887.

29. Diderholm E, Andrén B, Frostfeldt G, Genberg M, Jernberg T, Lagerqvist B, et al. The prognostic and therapeutic implications of increased troponin T levels and ST depression in unstable coronary artery disease: the FRISC II invasive troponin T electrocardiogram substudy. Am Heart J. 2002. 143:760–767.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download