INTRODUCTION
Percutaneous renal biopsy (PRB) is an essential tool in the diagnosis and treatment of patients with renal disease.1 Modification of the procedure by the addition of ultrasound (US) visualization has led to the widespread utilization of needle biopsy in the management of kidney disease.1 The use of real-time US guidance and automated needle biopsy has improved the rate of successful diagnosis in over 99% of cases.1 The safety of the percutaneous approach has also been maintained, with life-threatening complications occurring in less than 0.1% of biopsies.2 Nonetheless, complications related to PRB are reported to occur in 13% of biopsies and include hematuria, perirenal hemorrhage, arteriovenous fistula, and renal abscess. Moreover, 6.4% of complications are considered to be major complications, including urinoma following damage to the renal pelvis and inadvertent puncture of the spleen, mesenteric artery, and pancreas.2
Disruption of the urinary collecting system can produce internalized urine leaks that may result in continuous urine extravasation and form an encapsulated collection of urine, which is known as a urinoma.3 Although posttraumatic urine extravasation is common (2-18%), urinomas are extremely rare and only a few cases have been reported.4,5 Urinomas may initially be clinically occult and may manifest with delayed complications such as hydronephrosis, paralytic ileus, and electrolyte imbalances.6
Here we report a case in which a urinoma was caused by urine leakage after ultrasound-guided PRB and in which improvement occurred after the use of antibiotics and insertion of a double-J catheter.
CASE REPORT
A 20-year-old man presented to our hospital with a complaint of incidental microscopic hematuria according to an army physical exam performed in October 2005. In February and September 2006, repeated hematuria was observed. He was admitted to our hospital for a renal biopsy in December 2006.
In the physical examination, his vital signs were stable. Blood test results revealed the following values: white blood cells (WBC), 7,200/µl; segmented neutrophils, 61%; hemoglobin, 15.7 g/dl; platelets, 226,000/µl; ratio of aspartate aminotransferase to alanine aminotransferase (AST/ALT), 11/6 IU/L; ratio of blood urea nitrogen to creatinine (BUN/Cr), 13/0.8 mg/dl; and Na+/K+, 137/3.7 mg/dl. Urine test results revealed the following: negative protein; erythrocytes, 3+ erythrocytes/µl; red blood cells (RBC), many/HPF; WBC, 0-1/HPF; and dysmorphic RBC, 100%.
On the second day, ultrasound-guided percutaneous renal biopsy of the left kidney was performed twice, but no kidney tissue was found. Formation of a hematoma was observed on the left kidney by ultrasonography. On the third day, renal biopsy of the right kidney was performed again. Dark brown urine was removed, and the patient had sever pain in the left flank and left lower abdomen. The patient's vital signs after the renal biopsy were as follows: blood pressure, 120/80 mmHg; pulse rate, 76 per minute; respiratory rate, 20 per minute; and body temperature, 37℃. On the seventh day, the pain persisted and a heat sensation developed. The patient's vital signs were as follows: blood pressure, 130/80 mmHg; pulse rate, 88 per minute; respiratory rate, 20 per minute; and body temperature, 37.5℃.
A blood test on the seventh day showed the following values: WBC, 21,400/µl; blood pigment, 11.7 g/dl; platelets, 241,000/µl; BUN, 20 mg/dl; and Cr 1.7, mg/dl. Urine test results were as follows: leukocytes, 1+ leukocytes/µl; negative nitrites; urinary protein, 2+ mg/dl; urinary glucose, 1+ mg/dl; RBC, very many/HPF; and WBC, 11-15/HPF. Considering all results, we suspected an infection of the hematoma upon biopsy; computed tomography (CT) on the abdominal region was performed.
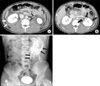
Contrast-enhanced abdominal CT and post-contrast plain abdominal radiography showed that contrast media had leaked around the left kidney and urinary tract (Fig. 1). The patient was diagnosed with urine leakage due to damage to the left urinary tract and kidney.
On the eighth day, a double-J catheter was inserted into the damaged left urinary tract, and cefoxitin and isepamicin sulfate were used because of pyrexia, which can be considered to be a complication of the urinoma (Fig. 2). On the 12th day, the urine became clear. Blood test results were as follows: WBC, 15,920/µl; blood pigment, 10.5 g/dl; platelets, 351,000/µl; AST/ALT, 31/67 IU/L; total bilirubin, increased to 1.3 mg/dl; BUN, 20 mg/dl; and Cr, 1.65 mg/dl. Because we believed that the drug eruption occurred because of the antibiotics, we changed the antibiotic regimen to ciprofloxacin. Subsequently, no further urine leakage occurred and the pain in the left flank and lower abdomen decreased. On the 16th day, blood test results showed that BUN had decreased to 11.3 mg/dl and that Cr had decreased to 1.26 mg/dl; the urine was clear. Urine test results were as follows: urinary glucose, 1+ mg/dl; erythrocytes, 3+ erythrocytes/µl; RBC, 31-35/HPF; and WBC, 3-5/HPF. As the situation became stabilized, on the on 18th day, the patient was discharged with a prescription for oral antibiotics while maintaining placement of the double-J stent.
DISCUSSION
In recent years, PRB has become a very useful tool in clinical nephrology and indispensable for diagnosis, therapy, and research. During that time, improvements in imaging techniques and biopsy needles have resulted in the ability to obtain adequate renal tissue for diagnosis in over 98% of renal biopsies.1
Indications for native renal biopsy include further evaluation of proteinuria, microscopic hematuria, rejection of a transplanted kidney, renal manifestations of systemic disease, and unexplained renal failure.1 Absolute contraindications to PRB include the presence of a bleeding diathesis, uncontrolled severe hypertension, an uncooperative patient, and a contracted and solitary native kidney. Severe azotemia, anatomic abnormalities of the kidney that may increase risk, drugs that alter hemostasis, pregnancy, and urinary tract infection are considered relative contraindications to PRB.1
With the introduction of automated biopsy guns and real-time US guidance, the risk of complications has been dramatically reduced. Despite the advances in security, simplicity, and handiness, however, this invasive procedure is not free from risks.7 The risk factors for complications of renal biopsy consist of poorly controlled hypertension, renal insufficiency (serum Cr>1.2 mg/dl), prolonged bleeding time, and frequent puncture.2
Although renal urine leakage generally results from blunt or penetrating renal trauma, obstruction in the genitourinary system, and iatrogenic injury during surgical procedures, PRB can cause renal urine leakage.8 Urine leaks and urinomas result from disruption of the urinary collecting system at any level from the calix to the urethra. Three major factors necessary for formation of a urinoma include a functioning kidney, a tear in the collecting system, and an element of ureteral obstruction.9 Extravasated urine over 2-5 days causes lipolysis of the perirenal fat. A fibroblastic reaction subsequently occurs, walling off the collection by a fibrous capsule without any lining epithelium.3
Urine leakage and urinomas have a variety of appearances and may be misdiagnosed as ordinary ascites, abdominal or pelvic abscesses or hematomas, cystic masses, or pancreatic pseudocysts.10 A diagnosis of urinoma should be considered in the case of an ill patient with an appropriate history and fluctuant mass in the flank. CT is the study of choice in the diagnosis of renal urine leakage and urinomas. Delayed-phase images are the key for demonstration of urine leakage because iodinated urine increases the attenuation of the urinoma over time.6
In most instances, small urinomas will reabsorb spontaneously, and drainage is not necessary. However, if a urinoma is larger or persists over several days, or if the patient develops fever or sepsis irrespective of urinoma size, image-guided drainage is clinically warranted.5,6,8 In the event of incomplete disruption of ureteral continuity, double-J stents may be satisfactorily used as the sole treatment. Placement of a nephrostomy catheter alone may not result in adequate diversion to allow a urine leak to be healed spontaneously. Therefore, in cases of persistent leakage from the collecting system, placement of a nephrostomy catheter, usually in combination with placement of a ureteral stent, is warranted.6
In our patient, the young age and the repeated renal biopsies could be considered risk factors. We assumed that the damage to the renal parenchyma and lower ureter occurred during a renal biopsy. Around the time of the diagnosis, a urinoma was found around the kidney and lower ureter, and complications occurred secondary to the closure, such as increased serum Cr (up to 1.7 mg/dl). Moreover, the patient had a low fever, leukocytosis, and an increase in WBC on the urine test. Considering all results, we determined that he had a urinoma and secondary urinary tract infection, and we prevented further urine leakage by using antibiotics and inserting a double-J catheter. Percutaneous nephrostomy was not performed because the urinoma was not large enough. The occurrence of urine leaks and urinoma after PRB is a very rare complication that may be improved by conservative treatment such as insertion of a double-J catheter and the use of antibiotics.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download