Abstract
We report a case of thymic carcinoma that was initially detected by echocardiography in an 80-year-old male who visited the emergency room for chest pain and had a history of myocardial infarction and percutaneous coronary intervention. Transthoracic echocardiography showed a huge extracardiac mass that was located in the anterior mediastinum and was diagnosed as a thymic carcinoma by biopsy.
Thymic carcinoma is an aggressive anterior mediastinal malignancy that can cause severe chest pain, although its incidence is rare. Echocardiography is useful for assessing chest pain in the emergency room, but the diagnosis of an extracardiac mass can be missed. The purpose of this report is to describe the validation of echocardiography for accessing an extracardiac mass that presented with chest pain.
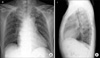
An 80-year-old male visited the emergency room for sharp chest pain that had lasted for 1 month. He had a history of inferior wall myocardial infarction and percutaneous coronary intervention on the proximal-middle right coronary artery 2 years ago. On the physical examination, his temperature was 36.6℃, his blood pressure was 100/60 mmHg, and his pulse was 81 beats/min. Laboratory examinations showed that the levels of CK-MB, troponin-I, and brain natriuretic peptide were not significantly elevated (2.8 ng/ml, 0.05 ng/ml, and 143 ng/ml, respectively). Electrocardiography revealed atrial fibrillation with Q-waves in lead II, III, and aVF. Chest radiography showed mild cardiomegaly and mediastinal widening (Fig. 1). Emergent coronary angiography was performed because of his history of previous myocardial infarction, but mild in-stent restenosis of the proximal right coronary artery and no new lesions of significant coronary artery stenosis for chest pain were shown.
Two-dimensional transthoracic echocardiography showed akinesia of the basal inferior wall, but no newly detected regional wall motion abnormality. However, a huge echogenic mass in the extracardiac area was found (Fig. 2A, B). This extracardiac mass was located in the upper anterior mediastinal area and showed vascularity by color Doppler imaging (Fig. 2C). The right ventricle was slightly compressed by this mass, but there was no detectable pericardial effusion. The previous echocardiography 1 year ago had shown no echogenic mass in the extracardiac area (Fig. 3).
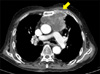
Chest computed tomography (CT) showed neither significant aortic dilation nor dissection. A huge anterior mediastinal mass was enhanced heterogeneously and directly invaded the sternal cartilage, costal cartilage, aortic arch, and pulmonary artery (Fig. 4). These CT findings were suggestive of a thymic carcinoma, and the severe chest pain of this patient was due to the huge anterior mediastinal mass with bone invasion.
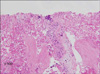
Histological findings by sonography-guided fine-needle aspiration demonstrated that the great majority of cells had tumoral necrosis and a very small number of cells had a high nucleus to cytoplasm ratio with hyperchromatin. These findings represented malignancy of the thymus; however, it was impossible to classify the subtype of tumor because of severe necrosis (Fig. 5). The patient was referred to an oncologist for further management of the left anterior mediastinal mass. Ptosis and muscle weakness for myasthenia gravis were suspected by neurologic physical examination. However, further specific tests were refused. According to the clinical presentation, the anterior mediastinal mass with invasiveness, and ptosis and muscle weakness, thymic carcinoma was clinically diagnosed and palliative radiotherapy was performed. However, palliative radiotherapy was discontinued because the patient complained of significant anorexia and weakness.
Only 15% to 20% of patients with acute chest pain actually have acute coronary syndrome.1,2 To discriminate patients with acute coronary syndrome from patients with non-cardiac chest pain is an immediate challenge to the primary clinician, especially in patients with a history of myocardial infarction and percutaneous coronary intervention. The accuracy and efficiency of the differential diagnosis of acute chest pain can be improved by combining various approaches based on vigilant history taking, electrocardiography, biochemical markers, and imaging modalities such as echocardiography, coronary computerized tomography, and coronary angiography. Because transthoracic echocardiography is widely available, with bedside utility and high sensitivity and negative predictive value in patients with acute chest pain for ischemia, it is very useful for evaluation in emergency circumstances. Therefore, after ruling out life-threatening conditions, it is necessary to consider other possible causes. Especially when chest pain is sharp and lasts for hours, it is frequently suspicious that the chest pain originates from a musculoskeletal cause. When a mediastinal mass such as a thymic carcinoma invades the chest wall, pleura, or heart, patients frequently present with chest pain.3
Our case illustrates several considerations in the initial evaluation of chest pain. First, chest CT was needed more than emergent coronary angiography because of the characteristics of the chest pain, which was sharp and had lasted for a month. Second, echocardiography could detect the extracardiac mass, which showed echogenic material.
Although a few cases of thymic cyst and malignancy have been documented,4-7 there has been no report that echocardiography detected an extracardiac mediastinal mass in the course of evaluating chest pain.
Thymic carcinoma is a heterogeneous group of aggressive and epithelial malignancies, and its incidence is rare. Most patients present with cough, dyspnea, or chest pain. While these symptoms are being evaluated, the malignancy is often incidentally detected by chest radiographs or CT scan.3 When an anterior mediastinal mass shows the presence of an irregular contour, necrotic or cystic component, heterogeneous enhancement, lymphadenopathy, and great vessel invasion on a CT scan, the mass is likely to be a thymic carcinoma.8 Mediastinal tumors, including thymoma, thymic carcinoma, and seminoma have been incidentally detected by Thallium-201 (Tl 201) imaging.9
Considering that the mediastinal mass is adjacent to the cardiac chamber, echocardiography can evaluate a mediastinal mass like a CT scan or Tl 201 uptake. The mediastinal mass can distort or partially displace one or more cardiac chambers, and an anterior mediastinal mass can compress the right heart chamber, which can be shown by echocardiography.5 It has been reported that thymic cancer was detected by echocardiography presenting as cardiac tamponade or supra vena cava (SVC) syndrome.6,7 However, cardiac tamponade as an initial manifestation of thymic cancer is rare.
Echocardiography is useful for the evaluation of chest pain in emergency circumstances and can detect a mediastinal mass because mediastinal masses are just adjacent to the heart; however, the diagnosis of an extracardiac mass can be missed. Therefore, it is important to look outside the heart in addition to the heart itself in the assessment of chest pain.
Figures and Tables
FIG. 2
Hypoechogenic mass (arrow) was shown in the parasternal long axis view (A) and short-axis view at the level of the aortic valve (B).The vascularity of the mass was documented in color flow imaging in the zoom view (C). M: mass, RV: right ventricle, LV: left ventricle, LA: left atrium, AV: aortic valve, PA: pulmonary artery.

FIG. 3
Echocardiography in the parasternal long axis view (A) and short axis view at the level of the aortic valve (B) 1 year previously showed no echogenic material in the retrosternal area.

References
1. Pope JH, Aufderheide TP, Ruthazer R, Woolard RH, Feldman JA, Beshansky JR, et al. Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med. 2000. 342:1163–1170.

2. Swinburn JM, Stubbs P, Soman P, Collinson P, Lahiri A, Senior R. Independent value of tissue harmonic echocardiography for risk stratification in patients with non-ST-segment elevation acute chest pain. J Am Soc Echocardiogr. 2002. 15:1031–1037.

4. Ozer N, Can I, Aytemir K, Atalar E, Erman M, Ovünç K, et al. Malignant thymoma invading the right atrium: a rare echocardiographic finding. Echocardiography. 2002. 19:61–62.

5. D'Cruz IA, Feghali N, Gross CM. Echocardiographic manifestations of mediastinal masses compressing or encroaching on the heart. Echocardiography. 1994. 11:523–533.
6. Canedo MI, Otken L, Stefadouros MA. Echocardiographic features of cardiac compression by a thymoma simulating cardiac tamponade and obstruction of the superior vena cava. Br Heart J. 1977. 39:1038–1042.

7. Woldow A, Kotler M, Goldstein S, Milcu M. Thymoma with pericardial tamponade. Clin Cardiol. 1995. 18:484–485.

8. Sadohara J, Fujimoto K, Müller NL, Kato S, Takamori S, Ohkuma K, et al. Thymic epithelial tumors: comparison of CT and MR imaging findings of low-risk thymomas, high-risk thymomas, and thymic carcinomas. Eur J Radiol. 2006. 60:70–79.

9. Seto H, Kageyama M, Shimizu M, Wu YW, Kamei T, Kakishita M. Assessment of residual tumor viability in thymic carcinoma by sequential thallium-201 SPECT: comparison with CT and biopsy findings. J Nucl Med. 1994. 35:1659–1661.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download