Abstract
The incidence and outcome of epilepsy in tuberous sclerosis (TS) patients have not yet been thoroughly investigated. The aim of this study was to evaluate the clinical features and prognosis of epileptic seizures associated with TS. The medical records of 29 patients who satisfied the diagnostic criteria for TS and were followed up for at least 2 years at the Department of Pediatrics, Chonnam National University Hospital (CNUH), between January 2000 and December 2010 were reviewed. Onset age of seizure, initial electroencephalography (EEG) findings, and efficacy of treatment were evaluated. Brain imaging studies were reanalyzed to determine the number of cortical tubers and subependymal nodules present. A total of 26 (89.6%) cases presented with seizures. In the seizure-controlled group (n=9, 34.6%), the mean number of cortical tubers was 4.5 (range, 0-16) and the mean number of subependymal nodules was 6.2 (range, 0-14). Initial EEG identified epileptiform discharges in 4 (44.5%) of these cases. In the seizure-sustained group (n=17, 58.6%), 10 patients had initial seizures before 1 year of age. In this group, the mean number of cortical tubers was 6.0 (range, 0-20) and the mean number of subependymal nodules was 6.0 (range, 1-11). A total of 15 (88.2%) had epileptiform discharges on their initial EEGs. In three patients who did not show any seizures during the observation period, the mean number of cortical tubers was 1.3 (range, 0-2), and the mean number of subependymal nodules was 4.6 (range, 0-13). Medical intractability of epilepsy in conjunction with TS did not correlate with age at onset of seizure, the number of cortical tubers, or subependymal nodules, but was associated with initial EEG findings.
Tuberous sclerosis (TS), which was first described by Bourneville in 1,880, is an autosomal dominant inherited neurocutaneous syndrome. The presence of TS genes on chromosomes 9 and 16 was recently revealed.1 The disease prevalence is 1 in 6,000, and the disease involves various organs forming hamartomas in the central nervous system (CNS), skin, eyes, heart, and lungs.2
In the case of CNS invasion, neurological symptoms such as epileptic seizures or mental retardation can be shown. Epileptic seizure, mental retardation, and facial angiofibroma are known as a clinical triad, but in two thirds of patients, these symptoms may not appear.3 Among those symptoms, epileptic seizure is a major factor determining quality of life in the affected children. Various types of epileptic seizure are reported in patients with TS, including infantile spasms;4,5 furthermore, the onset age or the severity of the seizures also varies in each patient. Even in cases with infantile spasms, the individual seizure outcomes vary and are strongly affected by the development of new antiepileptic agents, including vigabatrin. Several studies have been published about seizure or epilepsy outcomes in TS patients with infantile spasms after the introduction of new antiepileptic drugs.6,7 However, these studies were mainly focused on the seizures that developed during the infantile period. The epileptic seizures in children with TS have not been fully described.
In this study, we investigated initial clinical features including brain imaging studies and electroencephalograms in children with TS to determine possible prognostic predictors of epilepsy in TS.
Among 35 patients (20 male, 15 female) who were diagnosed as having TS by the criteria of Roach7 in the pediatric clinic of Chonnam National University Hospital (CNUH) from January 2000 to December 2010, 29 patients (16 male, 13 female) who were followed up for at least 2 years were the focus of this study. For each patient, age at diagnosis, presence of epileptic seizure, period of first seizure attack, initial electroencephalography (EEG), type of initial seizure, initial brain computed tomography (CT), initial brain magnetic resonance imaging (MRI), treatment, and prognosis were retrospectively reviewed. Initial EEG was analyzed as background activity, presence, and distribution of epileptiform discharge, whereas brain images were analyzed as the number of cortical tubers and subependymal nodules. In analyzing the data, we looked for correlations between the results and control of epileptic seizures. Types of epileptic seizures were sorted as infantile spasm, generalized tonic clonic type, tonic type, atonic type, and partial complex type. Also, anti-epileptic medication used to treat seizures during the follow-up period was reviewed. For patients whose epileptic seizures were controlled, onset of the seizure-controlled state was reviewed. The patients were classified into three groups by the presence and control of epileptic seizures as follows: the group without epileptic seizures, the seizure-controlled group, and the seizure-sustained group. SPSS software (version 18.0, SPSS Inc, Chicago, IL, USA) was used for the statistical analysis, and p-values less than 0.05 were considered to be significant.
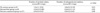
The mean follow-up period of the 29 patients who had been followed up for longer than 2 years was 99.6 months (range, 24-208 months). Among them, male patients were predominant; there were 16 (55%) males and 13 (45%) females, and the mean age at diagnosis was 51.6 months (range, 10 days to 168 months). Fifteen (51.7%) children were diagnosed before 1 year of age, the youngest one on 10 days after birth (Fig. 1). Three (10.3%) did not show any seizure during the follow-up period but mainly skin lesions; the mean age at diagnosis of this group was 114 months (range, 60-168 months). The mean follow-up period was 36 months (range, 24-48 months) (Table 1).
Twenty-six of 29 patients showed epileptic seizures during the follow-up period. Infantile spasm was the most common type of seizure, occurring in 12 (46%) cases, followed by generalized tonic clonic (n=8, 30.7%), tonic (n=3, 11.5%), complex partial (n=2, 7.6%), and atonic (n=1, 3.8%) seizure. Three patients showed epileptic seizure 40 days after being diagnosed as having TS, and 2 of them visited the hospital because of skin lesions and 1 for cardiac rhabdomyoma before 1 year of age. Two of them showed infantile spasms and 1 showed generalized tonic clonic seizure.
Among 26 patients, seizure was controlled in 9 (34.6%) cases and the mean duration before seizures were controlled was 64 months (range, 1-132 months). The mean duration of the seizure-free state was 61 months (range, 1-151 months) (Fig. 1, Table 1). In the other 17 (65.4%) cases, seizures were not controlled with multiple anti-epileptic medications during the follow-up period (mean, 97.41 months; duration, 24-204 months).
The first epileptic seizure was shown before 1 year of age in 15 cases, 10 (66.6%) of which were resistant to multiple anti-epileptic medications. Of 11 cases in which the first seizure was shown after 1 year of age, 7 (63.6%) were intractable. There was no definite correlation between the age of seizure onset and the outcome of seizure in TS (p=0.85).
In the analysis of first seizure type and prognosis of epileptic seizure in patients with TS, 3 (25.0%) of 12 patients with infantile spasms as their first seizure experienced control of seizures, whereas 6 (42.8%) of 14 patients with other seizure types showed improvement of seizures, which stood for a better prognosis (p=0.34) (Table 2).
Fifteen (75%) of 20 patients who showed epileptiform discharges in their initial EEGs had sustained seizure, whereas 4 (66.7%) of 6 who showed non-epileptiform abnormalities had a good outcome. Initial EEG finding and seizure outcome had a positive correlation (p=0.04) (Table 3).
Neuroimaging examinations were performed in all 29 patients (22 MRI, 7 CT). The counted mean number of cortical tubers was 4.9 (range, 0-20) and that of subependymal nodules was 5.6 (range, 0-14). The mean number of cortical tubers in patients without epilepsy (n=3) was 1.3±1.1 (range, 0-2), that in the seizure-controlled group (n=9) was 4.5±5.0 (range, 0-20), and that in the seizure-sustained group (n=17) was 6.0±5.9 (range, 0-2). No definite correlation between number of brain lesions and outcome of seizure was noted (p=0.9) (Table 4).
In 2 patients, astrocytoma was shown. In one, seizure was sustained and in the other it was controlled during the follow-up period. In the total 21 patients examined by MRI, 6 patients showed abnormal white matter; epileptic seizures in 3 of them were sustained and seizures in the other 3 patients were controlled.
Both MRI and CT were performed in 6 cases; one of them did not show cortical tubers in the CT image, whereas MRI revealed one cortical tuber. In the other 5 cases, there were no differences in brain lesions between the images.
The mean number of applied anti-epileptic medications was 3.1 (range, 1-6), including vigabatrin. In the seizure-controlled group (n=9), the mean number of drugs was 2 (range, 0-3), and all of the patients in this group took vigabatrin initially. Only 1 of them, however, improved with vigabatrin only. Four of them improved with topiramate, 2 with oxcarbazepine, and 1 with carbamazepine and lamotrigine (Table 1). In the seizure-sustained group (n=17), the mean number of applied drugs was 3.8 (range, 2-6). In the cases of infantile spasm (n=12), ACTH was applied in 3 (25.0%) and only 1 (33.3%) showed a seizure-control effect.
Because TS has been reported to have high frequency of neurological manifestations, such as epileptic seizure or mental retardation, evaluations and treatment of them are important. Epileptic seizure in children with TS is related to refractory seizure that is not responsive to multidrug treatment.5 Most TS patients (more than 90%) have seizure at least once, and 75% of them show their seizure before 1 year of age.7 In this study, a first seizure before 1 year of age was observed in 15 (57.6%) patients, which is relatively lower than in other reports.6 Infantile spasm was diagnosed in 12 cases (80.0%), which were the most frequent seizure type.5 Seizure was controlled in only 3 (25.0%) of the 12 patients, which was a lower ratio than that of the whole patient group (n=7/26, 34.0%). ACTH treatment was applied to 3 patients among them, and only one (33.3%) showed a seizure-control effect. Infantile spasms are a common symptom of TS that are present in one-third to two-thirds of cases.4 Features of infantile spasm are cluster seizure, which shows repeated spasms at short intervals and hypsarrhythmia on EEG.4 Pampigline reported that 20% of infantile spasms are caused by TS.8 Because infantile spasm itself is a risk factor for causing mental retardation, 4,9 prompt diagnosis and control of seizure is important. In this study of TS, the rate of infantile spasm was also high, and it tends to become refractory.
According to the report of Kim and Hwang,6 complex partial seizure is related to poor prognosis because it tends to remain refractory after childhood. But in this study, infantile spasm tended to be refractory, although it was not statistically significant. Only two cases of complex partial seizure were present in this study, one in the seizure-controlled group and the other in the sustained group.
Epileptic seizure in TS patients can occur at any time of life but is generally known to be exacerbated during puberty.8 In this study, 3 (patients 1, 2, and 8) of 9 patients whose seizures were controlled later showed seizure activities during the pubertal period; the other 6 showed activity at a preadolescent age (Fig. 2). Thus, continuous observation is needed.
Some studies have reported normal findings on neuroimaging examinations in patients with TS at an early age.1,10 In this study, MRI revealed many cortical tubers and subependymal nodules suitable for diagnosis of TS even in a 1-month-old infant with seizure at 10 days after birth.
Ninety percent of periventricular and subependymal hamartomas are accompanied by calcification and are easily observed by CT, and a positive correlation between degree of calcification in cortical tubers and severity of epileptic seizure has been reported.11-13 Epileptogenicity may also be related to the tuber itself because of a mass effect on surrounding tissue or vascular abnormalities.
Moreover, other studies have reported that the number and location of cortical tubers detected by MRI is closely related to the severity of epileptic seizure.14,15 In this study, more brain lesions were detected in the seizure-sustained group than in the seizure-controlled or seizure-free group, but the difference was not statistically significant (p=0.54). Although there was no strong positive correlation between the number of brain lesions and seizure outcomes, these results do not definitively indicate that there is no relation between the size or location of brain lesions and epileptogenicity itself, because there a case was reported in which surgical removal of cortical tubers improved seizure outcome.11
Even a subtle abnormal white matter lesion could be detected by MRI, and six or more abnormal findings in a patient are highly related to mental retardation.14 In this study of 6 cases, all of them were mentally retarded and had epilepsy; 3 (50%) of them were refractory.
In addition, previous studies reported that seizure-inducing cortical tubers could be differentiated by positron emission tomography (PET).16,17 However, PET was not performed in this study.
In the seizure-sustained group, the incidence of epileptiform discharges in the initial EEG recordings was higher (n=15/17, 88.2%) than in the seizure-controlled group (n=5/9, 55.5%). This result suggests that initial EEG abnormality may be related to incurableness.
The mean number of applications of anti-epileptic medications in TS patients was higher in the seizure-sustained group (3.8±1.2) than in the seizure-controlled group (2±0.9). However, a direct comparison was impossible because of a shortage of patients and various combinations of the drugs. Control of an epileptic seizure by additional topiramate, however, was observed in 4 of 9 cases, which suggested the efficacy of secondary medication other than vigabatrin in controlling epileptic seizures.18
To conclude, the correlation between the outcome of epilepsy and the initial clinical findings, including age of onset, first seizure type, and brain imaging findings, was not strong compared with that for initial EEG findings. Further extended study of the progression of epilepsy and other clinical features of TS might be required.
Figures and Tables
References
1. Devlin LA, Shepherd CH, Crawford H, Morrison PJ. Tuberous sclerosis complex: clinical features, diagnosis, and prevalence within Northern Ireland. Dev Med Child Neurol. 2006. 48:495–499.

2. Piao C, Yu A, Li K, Wang Y, Qin W, Xue S. Cerebral diffusion tensor imaging in tuberous sclerosis. Eur J Radiol. 2009. 71:249–252.

3. Hwang YS, Yoon YS. Clinical study of tuberous sclerosis - focused on neurologic manifestation and cardiac echo findings. J Korean Pediatr Soc. 1991. 34:992–998.
4. Staley BA, Vail EA, Thiele EA. Tuberous sclerosis complex: diagnostic challenges, presenting symptoms, and commonly missed signs. Pediatrics. 2011. 127:e117–e125.

5. Cho HR, Song SM, Yum MS, Lee EH, Jeong MH, Yoo HW, et al. Analysis of Overall Clinical Manifestations of Tuberous Sclerosis Complex Patients in the Childhood: Updated Diagnositic Criteria. J Korean Child Neurol Soc. 2009. 17:174–184.
6. Kim KJ, Hwang YS. Features and outcomes of epileptic seizure in tuberous sclerosis. J Korean Child Neurol Soc. 1995. 2:93–96.
7. Roach ES, Gomez MR, Northrup H. Tuberous sclerosis complex consensus conference: revised clinical diagnostic criteria. J Child Neurol. 1998. 13:624–628.

8. Pampiglione G, Moynahan EJ. The tuberous sclerosis syndrome: clinical and EEG studies in 100 children. J Neurol Neurosurg Psychiatry. 1976. 39:666–673.

9. Husain AM, Foley CM, Legido A, Chandler DA, Miles DK, Grover WD. West syndrome in tuberous sclerosis complex. Pediatr Neurol. 2000. 23:233–235.

10. Baron Y, Barkovich AJ. MR imaging of tuberous sclerosis in neonates and young infants. AJNR Am J Neuroradiol. 1999. 20:907–916.
11. Gallagher A, Madan N, Stemmer-Rachamimov A, Thiele EA. Progressive calcified tuber in a young male with tuberous sclerosis complex. Dev Med Child Neurol. 2010. 52:1062–1065.

12. Evans JC, Curtis J. The radiological appearances of tuberous sclerosis. Br J Radiol. 2000. 73:91–98.

13. Firat AK, Karakaş HM, Erdem G, Yakinci C, Biçak U. Diffusion weighted MR findings of brain involvement in tuberous sclerosis. Diagn Interv Radiol. 2006. 12:57–60.
14. Chou IJ, Lin KL, Wong AM, Wang HS, Chou ML, Hung PC, et al. Neuroimaging correlation with neurological severity in tuberous sclerosis complex. Eur J Paediatr Neurol. 2008. 12:108–112.

15. Arulrajah S, Ertan G, Jordan L, Tekes A, Khaykin E, Izbudak I, et al. Magnetic resonance imaging and diffusion-weighted imaging of normal-appearing white matter in children and young adults with tuberous sclerosis complex. Neuroradiology. 2009. 51:781–786.

16. Major P, Rakowski S, Simon MV, Cheng ML, Eskandar E, Baron J, et al. Are cortical tubers epileptogenic? Evidence from electrocorticography. Epilepsia. 2009. 50:147–154.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download