Abstract
The purpose of the present study was to clarify the possible relationship between nitroglycerin (NTG)-induced headache and both vascular functional and organic atherosclerosis. The study included 96 patients with NTG-induced headache (group I: 54.7±9.5 years, 52 males) and 204 patients without headache (group II: 58.1±9.1 years, 127 males) who suffered from new-onset chest pain. Flow-mediated dilation and nitroglycerin-mediated dilation were significantly greater in group I than in group II (8.8±4.1% vs. 7.1±3.5%, p=0.001, and 23.1±7.3% vs. 17.1±11.8%, p<0.001, respectively). The carotid intima-media thickness was significantly smaller in group I than in group II (0.55±0.15 mm vs. 0.67±0.22 mm, p=0.001). Heart-carotid pulse wave velocity was significantly lower in group I than in group II (784.5±160.1 m/s vs. 979.1±215.6 m/s, p=0.003). In the multiple regression analysis, the absence of NTG-induced headache was a predictor of coronary artery disease (CAD) (odds ratio: 17.89, 95% confidence interval: 7.89-40.02, p<0.001). NTG-induced headache developed more frequently in patients with normal coronary arteries or minimal CAD than in patients with obstructive CAD. The presence of NTG-induced headache might be helpful and provide additional information in evaluating patients with chest pain syndrome.
Nitroglycerin (NTG)-induced headache is the most prominent side effect of nitrate therapy in patients with chest pain. Much work has been published regarding the role of increased nitric oxide (NO) in migraine subjects during acute migraine attacks.1-3 Intracranial arteries are dilated during migraine attack to increase intracranial flow, and when the migraine attack has subsided, intracranial flow returns to the baseline level.4-6 The capacity of blood vessels to respond to NO donors in the lumen confers the ability to self-regulate vascular tone and to adjust blood flow and distribution in response to changes in the local environment, indicating that NO may play a key role in migraine.
Therefore, we hypothesized that patients with NTG-induced headache have preserved vascular smooth muscle function and would show an increased response to NTG-induced dilation (NMD) in the brachial artery. However, there are few published data evaluating the association between NTG-induced headache, angiographic coronary artery disease (CAD), and noninvasive measurements of atherosclerosis in patients with chest pain. Therefore, the aim of this study was to clarify the possible relationship between NTG-induced headache and both vascular functional and organic atherosclerosis in patients with chest pain.
From September 9, 2007, to September 9, 2009, the study included 300 patients who were scheduled for coronary angiography at Chonnam National University Hospital because of new-onset chest pain. Patients were divided into two groups according to the presence or absence of NTG-induced headache: 96 patients with NTG-induced headache (group I: 54.7±9.5 years, 52 males) and 204 patients without NTG-induced headache (group II: 58.1±9.1 years, 127 males). Patients were excluded from this study if they had a history of chronic headache and migraine; use of nitrates for more than 3 months; previous myocardial infarction, heart failure, or other serious diseases; or former coronary angiography. Coronary angiography was performed within 1 month after NTG administration with the usual clinical indications.
After the sublingual administration of 0.6 mg NTG for NTG-mediated submaximal vasodilation, the presence of NTG-induced headache was determined according to the criteria proposed by the International Headache Society7: A. Headache with at least one of the following characteristics and fulfilling criteria C and D: 1) bilateral, 2) frontotemporal location, 3) pulsating quality, 4) aggravated by physical activity, B. Absorption of an NO donor, C. Headache develops within 10 minutes after absorption of NO donor, D. Headache resolves within 1 hour after release of NO has ended.7 Flow-mediated dilation (FMD), NMD, and inflammatory and coagulation markers were measured early in the morning after the patients had fasted overnight for more than 12 hours.
FMD of the brachial artery was measured as the noninvasive parameter of endothelial function according the guideline3 described previously. Vasoactive therapies were not prescribed for at least 24 hours before the study until the measurement was completed except for short-acting sublingual NTG, which was withheld for 1 hour before the study.
All studies were performed early in the morning (0600-0800 hours) before coronary angiography, by use of an 8 MHz high-resolution lineal vascular ultrasound transducer (Acuson Sequoia 512; Siemens Medical Solutions, USA), which was used to image the brachial artery longitudinally just above the antecubital fossa. A tourniquet for measuring blood pressure was placed on the lower arm to create shear stress induced by reactive hyperemia. After baseline measurements of the brachial artery diameter, the blood pressure cuff was inflated to at least 50 mmHg above systolic blood pressure to occlude arterial flow for 5 minutes. Subsequent deflation of the cuff induces a brief high-flow state through the brachial artery (reactive hyperemia) to accommodate the dilated resistance vessels. The resulting increase in shear stress causes the brachial artery to dilate. The brachial artery was imaged for the first 2 minutes of reactive hyperemia continuously. The flow-mediated dilatory response was used as a measure of endothelial-dependent dilation. After 10 minutes of rest to reestablish the baseline condition, 0.6 mg of NTG was administered sublingually. The brachial artery was imaged for 10 minutes continuously to measure peak diameter. NMD was used as a measure of endothelial-independent dilation. All patients were asked about NTG-induced headache after sublingual administration. In this studies, the intra- and inter-observer variability for the repeated measurements of resting arterial diameter were excellent (r=0.997, p< 0.001, and r=0.997, p<0.001).
The carotid intima-media thickness (IMT) was measured in the left and right common carotid arteries by use of high-resolution B-mode ultrasound (Acuson Sequoia 512; Siemens Medical Solutions, USA) with an electric linear transducer (mid frequency 8.0 MHz). Each IMT was determined for the far wall of both common carotid arteries. The common carotid artery was studied in the longitudinal plane from the level of the common carotid artery. The images were recorded from the approach showing the greatest distance between the lumen-intima interface and the media-adventitia interface. All scans were recorded on super-VHS videotape for subsequent analysis. The IMT was measured from the B-mode screen to within 10 mm proximal to the bifurcation and synchronized with the R-wave peak by one investigator who was blinded to the patient characteristics. The mean IMT was calculated as the mean of 10 measurements using electronic calipers. In the studies presented here, the intra- and inter-observer variability for the repeated measurement of IMT were 0.08±0.001 mm and 0.13±0.002 mm, respectively.
We used heart-carotid pulse wave velocity (PWV) and brachial-ankle PWV as the index for atherosclerosis. A medical technician measured the PWV and blood pressure of each subject twice by using a brachial-ankle PWV/ABI device (Nippon Colin, Aichi, Japan) while the subject was at rest in a supine position. This device, approved by the US Food and Drug Administration as VP-2000/1000, can monitor bilateral brachial and ankle pressure wave forms simultaneously by using the volume plethysmographic method, with two optional tonometry sensors for carotid and femoral arterial wave measurements. The medical technicians practiced PWV measurements beforehand and made arrangements for standardization.
No anti-anginal therapy was prescribed for at least 24 hours before catheterization, except for the unrestricted use of sublingual NTG. The coronary arteries were divided into segments according to the American Heart Association classification. Coronary angiograms were analyzed with a validated quantitative coronary angiography (QCA) system (Philips H5000 OR Allura DCI program; Philips Medical Systems, Eindhoven, The Netherlands). With the outer diameter of the contrast-filled catheter as the calibration standard, the minimal lumen diameter and reference diameter were measured in diastolic frames from orthogonal projections. Obstructive CAD was defined as significant if the mean lumen diameter reduction was ≥50% in any of the major coronary arteries.
Diabetes mellitus was defined as receiving oral hypoglycemic agents or insulin to lower blood glucose levels or known fasting blood glucose values of ≥126 mg/dL or postprandial 2-hour blood glucose values of ≥200 mg/dL. Hypertension was defined as receiving antihypertensive medications or known blood pressures of ≥140/90 mmHg. Dyslipidemia was defined as total cholesterol ≥220 mg/dL or low-density lipoprotein cholesterol ≥130 mg/dL. Smokers were defined as those who were smoking currently or had stopped smoking within 3 months of enrollment in the present study.
We measured the blood levels of white blood cell (WBC) counts, monocyte counts, high-sensitivity C-reactive protein (hs-CRP), and fibrinogen to examine the coagulation system. Blood samples were taken by venipuncture in the morning from patients after they had fasted for >12 hours before angiography. Hs-CRP was measured by immunoturbidimetric CRP-Latex (II) assay by using an Olympus AU 5400. Measurement of fibrinogen was performed by chromogenic assay (Sysmex, CA1500, Mundelein, IL, USA).
Data for the categorical variables are expressed as both the number and the percentage of patients. For continuous variables, data are expressed as the mean±SD. Independent sample t-test was used to compare variables between the two groups. Comparison between different groups was made by using the chi-square test for categorical variables. Multivariate logistic regression analysis was performed to identify independent predictors of CAD. A p value<0.05 was considered indicative of statistical significance. All statistical calculations were performed with a commercially available statistical software package (SPSS, version 15.0; SPSS Inc, Chicago, IL, USA).
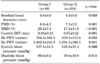
The clinical characteristics including the risk factors of the study population are shown in Table 1. Age was significantly greater in group II than in group I. However, there were no significant differences in gender, risk factors, blood pressure, or medications between the two groups.
Hs-CRP, fibrinogen, and homocysteine levels were not significantly different between the two groups. The level of triglyceride was significantly lower in group I than in group II.
The data on brachial diameter, FMD, and NMD are shown in Table 2. The mean brachial basal diameter was significantly smaller in group I than in group II. The mean FMD was significantly higher in group I than in group II. The mean NMD was significantly greater in group I than in group II.
The data on the mean carotid IMT, the mean heart-carotid PWV (hcPWV), and the mean brachial-ankle PWV (baPWV) are shown in Table 2. The mean carotid artery IMT was significantly smaller in group I than in group II. The mean hcPWV and the mean baPWV were significantly lower in group I than in group II (Table 2).
One hundred sixty-four patients had normal coronary arteries or minimal coronary artery disease. One hundred thirty-six patients had obstructive CAD with greater than 50% luminal diameter narrowing in one or more of the left or right coronary arteries or their major branches. In patients with normal coronary arteries or minimal CAD, 87.4% reported significant episodes of headaches after NTG use compared with only 12.6% of patients with obstructive CAD (p<0.001) (Table 1).
We performed multivariate analysis to determine independent predictors of coronary artery disease. The following variables were tested (all with p<0.2 in univariate analysis): age, hypertension, diabetes mellitus, smoking, HDL-cholesterol, triglyceride, NTG-induced headache, FMD, NMD, carotid IMT, and hcPWV. The absence of NTG-induced headache (odds ratio: 17.89, 95% confidence interval: 7.89-40.02, p<0.001) was the only independent predictor of CAD (Table 3).
The present study demonstrated that 1) patients with NTG-induced headache had greater NMD and FMD in the brachial artery, smaller carotid IMT, and lower PWV than did patients without NTG-induced headache; 2) NTG-induced headache developed more frequently in patients with normal coronary arteries or minimal CAD than in patients with obstructive CAD; 3) and the absence of NTG-induced headache was an independent predictor of CAD.
There are conflicting reports regarding the relationship between a history of migraine headaches and angina and between migraine headaches and cardiovascular events such as myocardial infarction and stroke. Although multiple population-based studies have found that patients with migraine headaches are more likely to have chest pain symptoms,8-11 the reported association between migraine headaches and major cardiovascular events has been inconsistent.
One large study observed a relationship between migraine headaches and cardiovascular events in a community-based of population of 3654 Australian men and women and noted that subjects with migraine headaches were twice as likely to have a self-reported history of myocardial infarction.12 Conversely, findings from the more recent prospective Nurses' and Physicians' Health Studies failed to show an association between migraine headaches and verified cardiovascular events, including angina and myocardial infarction.13 A possible explanation for these discrepant findings may include the reliance on self-reported cardiovascular events. Studies that used verified events data have consistently highlighted an absence of an association between migraine headaches and cardiovascular events.14
In the present study, NTG-induced headache developed more frequently in patients with normal coronary arteries or minimal CAD than in patients with obstructive CAD by coronary angiography. Nitrates can dilate epicardial coronary arteries and collateral vessels in patients with obstructive CAD.15,16 The prevalence of carotid atheromatous plaque was highly correlated with that of CAD, and carotid vascular elasticity to NTG use was decreased in patients with severe CAD.17 Therefore, NTG-induced headache might occur less frequently in patients with atherosclerosis.
The vascular endothelium has been reported to be a multifunctional component whose integrity is essential for normal vascular physiology. Loss of adequate endothelial cell function is most widely quantified by assessing FMD and NMD. Previously, we reported that decreased FMD and increased carotid IMT and PWV were associated with CAD.18 In particular, the dilatory response to NTG is used as a measure of endothelium-independent vasodilation. The vasodilator response to NTG is impaired in the brachial artery of patients with CAD, which illustrates functional abnormalities in smooth muscle dilation in adults with atherosclerosis.19,20 However, there is strong and growing evidence that abnormalities in endothelial function are present before the development of angiographically evident coronary atherosclerosis in patients with coronary risk factors.21-24 Previous studies suggested that the increasing arterial stiffness may relate to early endothelial dysfunction and overt atherosclerosis.19,20 The results of the present study, which showed that the absence of NTG-induced headache is an independent predictor of CAD, are consistent with the findings of these studies. To the best of our knowledge, this study is the first to assess the arterial stiffness of patients with chest pain by means of NTG-induced headache and to compare this method with other techniques used to evaluate coronary artery stenosis, endothelial dysfunction, and atherosclerosis, such as carotid IMT and PWV. The identification of NTG-induced headache is a simple and inexpensive way of assessing vascular function and may be used to screen patients for early detection of coronary artery disease.
There are several limitations to be mentioned. First, in order to evaluate endothelial function, organic atherosclerosis, and arterial stiffness, the data obtained from the study subjects must be compared with those from a control group. The major limitation of this study is the lack of control data for comparison. Second, the sample size was relatively modest. Therefore, further study is needed with a larger number of subjects. Further studies are also needed to establish the exact mechanisms of NTG-induced headache in patients with chest pain, to investigate other markers of endothelial dysfunction, and to examine the potential role of smooth muscle function as an aid to risk-stratifying patients with NTG-induced headache. Third, we did not measure how many patients with NTG-induced headache experienced aura. Patients with NTG-induced headache with aura have been shown to be a group at slightly increased risk for vascular events like ischemic stroke.25 Our study was unable to explore this association. Previously, several clinical and hemodynamic studies using nitrate were published in Korea.18,26-29 However, the clinical impact and mechanisms are not exactly known. Fourth, the origins of chest pain in our study patients have not been determined, although it is possible that the patients had coronary artery spasm. Previous studies7,8 showed that coronary vasospasm is closely related to atherosclerotic coronary artery disease. It is common for vasospasm to occur in lesions with angiographically normal or nearly normal coronary arteries. In the present study, provocative tests for coronary artery spasm using acetylcholine or ergonovine were not used. The number of patients who had coronary artery spasm remained unknown, and the possible relation between coronary artery spasm and NTG-induced headache was not determined. Further studies should be considered to ascertain the role of NTG-induced headache in patients with mild coronary artery stenosis and vasospasm.
In conclusion, the results of the present study show that NTG-induced headache is associated with increased NMD and FMD in patients with chest pain. NTG-induced headache developed more frequently in patients who had normal coronary arteries or minimal CAD than in patients with obstructive CAD. The presence of NTG-induced headache might be helpful and provide additional information in evaluating patients with chest pain syndrome.
Figures and Tables
ACKNOWLEDGMENT
This study was supported by grants of the Korea Healthcare Technology R&D project, Ministry for Health, Welfare & Family Affairs (A084869), and from the Fundamental R&D Program for Core Technology of Materials funded by the Ministry of Knowledge Economy (K00060-282), Korea.
References
1. Marsh N, Marsh A. A short history of nitroglycerine and nitric oxide in pharmacology and physiology. Clin Exp Pharmacol Physiol. 2000. 27:313–319.

2. Goadsby PJ, Lipton RB, Ferrari MD. Migraine--current understanding and treatment. N Engl J Med. 2002. 346:257–270.
3. Celermajer DS, Sorensen KE, Gooch VM, Spiegelhalter DJ, Miller OI, Sullivan ID, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992. 340:1111–1115.

4. Woods RP, Iacoboni M, Mazziotta JC. Brief report: bilateral spreading cerebral hypoperfusion during spontaneous migraine headache. N Engl J Med. 1994. 331:1689–1692.

5. Bednarczyk EM, Remler B, Weikart C, Nelson AD, Reed RC. Global cerebral blood flow, blood volume, and oxygen metabolism in patients with migraine headache. Neurology. 1998. 50:1736–1740.

6. Iversen HK, Nielsen TH, Olesen J, Tfelt-Hansen P. Arterial responses during migraine headache. Lancet. 1990. 336:837–839.

7. Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders. 2nd edition. Cephalalgia. 2004. 24:Suppl 1. 9–160.
8. Ahmed B, Bairey Merz CN, McClure C, Johnson BD, Reis SE, Bittner V, et al. Migraines, angiographic coronary artery disease and cardiovascular outcomes in women. Am J Med. 2006. 119:670–675.

9. Kurth T, Schürks M, Logroscino G, Gaziano JM, Buring JE. Migraine, vascular risk, and cardiovascular events in women: prospective cohort study. BMJ. 2008. 337:a636.

10. Kurth T, Gaziano JM, Cook NR, Logroscino G, Diener HC, Buring JE. Migraine and risk of cardiovascular disease in women. JAMA. 2006. 296:283–291.

11. Kurth T, Gaziano JM, Cook NR, Bubes V, Logroscino G, Diener HC, et al. Migraine and risk of cardiovascular disease in men. Arch Intern Med. 2007. 167:795–801.

12. Mitchell P, Wang JJ, Currie J, Cumming RG, Smith W. Prevalence and vascular associations with migraine in older Australians. Aust N Z J Med. 1998. 28:627–632.

13. Cook NR, Benseñor IM, Lotufo PA, Lee IM, Skerrett PJ, Chown MJ, et al. Migraine and coronary heart disease in women and men. Headache. 2002. 42:715–727.

14. Rose KM, Carson AP, Sanford CP, Stang PE, Brown CA, Folsom AR, et al. Migraine and other headaches: associations with Rose angina and coronary heart disease. Neurology. 2004. 63:2233–2239.

15. Dodge HT, Brown BG. The mechanism of action of nitroglycerin. Stenosis vasodilation as a major component of the drug response. Scand J Clin Lab Invest Suppl. 1984. 173:41–45.
16. Goldstein RE, Stinson EB, Scherer JL, Seningen RP, Grehl TM, Epstein SE. Intraoperative coronary collateral function in patients with coronary occlusive disease. Nitroglycerin responsiveness and angiographic correlations. Circulation. 1974. 49:298–308.

17. Lai CP, Koyanagi S, Shaw CK, Takeshita A. Evaluation of the early stage of carotid atherosclerosis using the vascular response to nitroglycerin and high-resolution ultrasonography. Jpn Circ J. 1998. 62:494–498.

18. Cho SH, Jeong MH, Park IH, Choi JS, Yoon HJ, Kim KH, et al. Endothelial dysfunction, increased carotid artery intima-media thickness and pulse wave velocity, and increased level of inflammatory markers are associated with variant angina. J Cardiol. 2009. 54:183–191.

19. Adams MR, Robinson J, McCredie R, Seale JP, Sorensen KE, Deanfield JE, et al. Smooth muscle dysfunction occurs independently of impaired endothelium-dependent dilation in adults at risk of atherosclerosis. J Am Coll Cardiol. 1998. 32:123–127.

20. Raitakari OT, Seale JP, Celermajer DS. Impaired vascular responses to nitroglycerin in subjects with coronary atherosclerosis. Am J Cardiol. 2001. 87:217–219.

21. Perrone-Filardi P, Cuocolo A, Brevetti G, Silvestro A, Storto G, Dellegrottaglie S, et al. Relation of brachial artery flow-mediated vasodilation to significant coronary artery disease in patients with peripheral arterial disease. Am J Cardiol. 2005. 96:1337–1341.

22. Benjamin EJ, Larson MG, Keyes MJ, Mitchell GF, Vasan RS, Keaney JF Jr, et al. Clinical correlates and heritability of flow-mediated dilation in the community: the Framingham Heart Study. Circulation. 2004. 109:613–619.

23. MacAlpin RN. Relation of coronary arterial spasm to sites of organic stenosis. Am J Cardiol. 1980. 46:143–153.

24. Miyao Y, Kugiyama K, Kawano H, Motoyama T, Ogawa H, Yoshimura M, et al. Diffuse intimal thickening of coronary arteries in patients with coronary spastic angina. J Am Coll Cardiol. 2000. 36:432–437.

25. Kurth T, Slomke MA, Kase CS, Cook NR, Lee IM, Gaziano JM, et al. Migraine, headache, and the risk of stroke in women: a prospective study. Neurology. 2005. 64:1020–1026.

26. Lim SY, Bae EH, Jeong MH, Kim HG, Lim JH, Park HW, et al. The clinical effect of intracoronary adenosine and nicorandil on no-reflow in acute myocardial infarction during percutaneous coronary intervention. Korean Circ J. 2004. 34:258–264.

27. Kim W, Jeong MH, Gill GC, Jeong WG, Hong YJ, Lee SH, et al. The changes of fractional flow reserve after intracoronary nitrate and nicorandil injection in coronary artery ectasia. Korean Circ J. 2003. 33:37–43.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download