Abstract
Purpose
Spontaneous neonatal gastric perforation is a rare but fatal disease with unclear etiology. In this study, we reviewed its clinical manifestations, outcomes, and discussed the etiology and prognostic factors.
Methods
There were 12 neonates with gastric perforation in our hospital from 1989 to 2015. Their medical records were reviewed retrospectively including birth record, associated disease, site and size of perforation, type of surgical management, clinical outcome. Also, the prognostic factors were analyzed.
Results
The median gestational age and birth weight was 32 weeks (range, 26-43 weeks; preterm birth rate, 66.7%) and 1,883 g (range, 470-4,400 g), respectively. Five patients had associated gastrointestinal anomalies including esophageal atresia and tracheoesophageal fistula (two patients), midgut volvulus, non-rotation and microcolon, and meconium plug syndrome. The median age at surgery was six days after birth (range, 2-13 days), and the median weight at surgery was 1,620 g (range, 510-3,240 g). Upper third part of stomach was the most frequently involved location of perforation. The size of perforation varied from pin point to involving the whole greater curvature. Primary repairs were done in seven cases, and in five cases, resections of necrotic portion were needed. Mortality rate was 33.3% (n=4), morbidity (re-operation) rate was 16.7% (n=2). The causes of death were sepsis (n=3), and heart failure from Ebstein anomaly (n=1). The median hospital stay was 92.5 days (range, 1-176 days). The factors mentioned as prognostic factors in previous studies showed no significant relations to the mortality and morbidity in our study.
Conclusion
There were improvements of outcomes in patients with large size perforation. As previous studies, we assume these improvements were possible due to the improvements of critical care medicine. Given that rare incidence, a multi-center study can help us get a better understanding of this disease, and a better outcome.
Figures and Tables
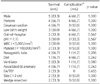
Table 1
Demographic Data of Neonate with Spontaneous Gastric Perforation

M, male (gender); F, female; GI, gastrointestinal; EA/TEF, esophageal atresia/tracheoesophageal fistula; VACTERL, vertebral anomalies, anal atresia, congenital heart disease, tracheoesophageal fistula or esophageal atresia, reno-urinary anomalies, and limb defect; U, upper stomach; M, middle stomach; L, lower stomach; GC, greater curvature; LC, lesser curvature; WR, wedge resection.
References
1. Duran R, Inan M, Vatansever U, Aladağ N, Acunaş B. Etiology of neonatal gastric perforations: review of 10 years' experience. Pediatr Int. 2007; 49:626–630.
2. Leone RJ Jr, Krasna IH. ‘Spontaneous’ neonatal gastric perforation: is it really spontaneous? J Pediatr Surg. 2000; 35:1066–1069.
3. Macgillivray PC, Stewart AM, MacFarlane A. Rupture of the stomach in the newborn due to congenital defects in the gastric musculature. Arch Dis Child. 1956; 31:56–58.
4. Campbell JR. Gastrointestinal perforations in the newborn. In : Welch KJ, Randolph JG, Ravitch MM, editors. Pediatric surgery. Chicago: Year Book Medical Publishers;1986. p. 824–826.
5. Cho YH, Kim HY, Kim SH, Byun SY, Park KH, Han YM. Gastric perforation in the neonatal period: differences between preterm and term infants. Neonatal Med. 2015; 22:150–155.
6. Yang CY, Lien R, Fu RH, Chu SM, Hsu JF, Lai JY, et al. Prognostic factors and concomitant anomalies in neonatal gastric perforation. J Pediatr Surg. 2015; 50:1278–1282.
7. Durham MM, Ricketts RR. Neonatal gastric perforation and necrosis with Hunt-Lawrence pouch reconstruction. J Pediatr Surg. 1999; 34:649–651.
8. Lin CM, Lee HC, Kao HA, Hung HY, Hsu CH, Yeung CY, et al. Neonatal gastric perforation: report of 15 cases and review of the literature. Pediatr Neonatol. 2008; 49:65–70.
9. Chung MT, Kuo CY, Wang JW, Hsieh WS, Huang CB, Lin JN. Gastric perforation in the neonate: clinical analysis of 12 cases. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. 1994; 35:460–465.
10. Rosser SB, Clark CH, Elechi EN. Spontaneous neonatal gastric perforation. J Pediatr Surg. 1982; 17:390–394.
11. Jactel SN, Abramowsky CR, Schniederjan M, Durham MM, Ricketts RR, Clifton MS, et al. Noniatrogenic neonatal gastric perforation: the role of interstitial cells of Cajal. Fetal Pediatr Pathol. 2013; 32:422–428.
12. Ohshiro K, Yamataka A, Kobayashi H, Hirai S, Miyahara K, Sueyoshi N, et al. Idiopathic gastric perforation in neonates and abnormal distribution of intestinal pacemaker cells. J Pediatr Surg. 2000; 35:673–676.
13. Dunham EC, Goldstein RM. Rupture of the stomach in newborn infants: report of two cases. J Pediatr. 1934; 4:44–50.
14. Hwang S, Park J, Chang S. Clinical review of spontaneous gastric perforation in the newborn. J Korean Assoc Pediatr Surg. 2003; 9:30–40.
15. Telle JT. Idiopathic neonatal gastric perforation: report of six cases. J Indiana State Med Assoc. 1968; 61:602–605.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download