Abstract
Purpose
The use of CT as a diagnostic tool in pediatric acute appendicitis is increasing because of its high sensitivity and specificity. However, due to both the serious concerns about radiation of CT and the convenience and reasonable cost of ultrasound (US) examination, US has value on the initial diagnosis of acute appendicitis despite of the lower sensitivity in children. The purpose of this study was to examine the factors that affect the rate of false negative diagnosis of the ultrasound from the patients who received laparoscopic appendectomy.
Methods
The pediatric appendectomy cases from 2002 to 2013 in Yeouido St. Mary's Hospital have been reviewed through the medical records. We included patients who underwent an initial screening by ultrasound examination.
Results
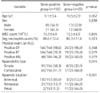
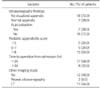
Among 181 patients, 156 patients were the sono-positive group and 25 patients were sono-negative group. There is no significant difference in ages, genders, physical examination findings and white blood cell count between the two groups. But, the degree of inflammation of appendicitis (simple, 58.3% vs. 32.0%; complicated, 41.7% vs. 68.0%) and the appendix position (antececal, 85.0% vs. 12.0%; retrocecal, 13.7% vs. 44.0%; pelvic, 1.3% vs. 44.0%) were significantly different between the two groups (sono-positive group vs. sono-negative group; p<0.05).
Figures and Tables
References
1. Mostbeck G, Adam EJ, Nielsen MB, Claudon M, Clevert D, Nicolau C, et al. How to diagnose acute appendicitis: ultrasound first. Insights Imaging. 2016; 7:255–263.

2. van den Bogaard VA, Euser SM, van der Ploeg T, de Korte N, Sanders DG, de Winter D, et al. Diagnosing perforated appendicitis in pediatric patients: a new model. J Pediatr Surg. 2016; 51:444–448.

3. Galai T, Beloosesky OZ, Scolnik D, Rimon A, Glatstein M. Misdiagnosis of acute appendicitis in children attending the emergency department: the experience of a large, tertiary care pediatric hospital. Eur J Pediatr Surg. 2016; 01. 08. [Epub]. DOI: 10.1055/s-0035-1570757.

4. Reynolds SL. Missed appendicitis in a pediatric emergency department. Pediatr Emerg Care. 1993; 9:1–3.

5. Rothrock SG, Skeoch G, Rush JJ, Johnson NE. Clinical features of misdiagnosed appendicitis in children. Ann Emerg Med. 1991; 20:45–50.

6. Puylaert JB. Acute appendicitis: US evaluation using graded compression. Radiology. 1986; 158:355–360.

7. Craig S, Dalton S. Diagnosing appendicitis: what works, what does not and where to from here? J Pediatr Child Health. 2016; 52:168–173.
8. Duke E, Kalb B, Arif-Tiwari H, Daye ZJ, Gilbertson-Dahdal D, Keim SM, et al. A systematic review and meta-analysis of diagnostic performance of MRI for evaluation of acute appendicitis. AJR Am J Roentgenol. 2016; 206:508–517.

9. Cohen B, Bowling J, Midulla P, Shlasko E, Lester N, Rosenberg H, et al. The non-diagnostic ultrasound in appendicitis: is a non-visualized appendix the same as a negative study? J Pediatr Surg. 2015; 50:923–927.

11. Chung JB, Jeon SY, Song YT. A clinical score and ultrasonography for the diagnosis of childhood acute appendicits. J Korean Assoc Pediatr Surg. 2004; 10:117–122.

12. Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. Am J Roentgenol. 2001; 176:289–296.

13. Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012; 380:499–505.

14. Partain KN, Patel A, Travers C, McCracken CE, Loewen J, Braithwaite K, et al. Secondary signs may improve the diagnostic accuracy of equivocal ultrasounds for suspected appendicitis in children. J Pediatr Surg. 2016; 51:1655–1660.

15. Butler M, Servaes S, Srinivasan A, Edgar JC, Del Pozo G, Darge K. US depiction of the appendix: role of abdominal wall thickness and appendiceal location. Emerg Radiol. 2011; 18:525–531.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download