Abstract
Purpose
The aim of this study was to analyze of the risk factors for surgical procedure on ileo-colic intussusception without leading point in children.
Methods
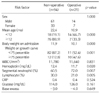
We retrospectively reviewed medical records of patient treated for ileo-colic intussusception between January 2003 and December 2014. We exclude the patients who had leading point. Because of the large difference on patient's numbers between non-operative group (cases of ileo-colic intussusceptions successfully reduced by air reduction) and operative group (cases underwent operation due to failed air reduction), we compared the data of operative group of patients without leading point between 2003 and 2014 with the data of non-operative group as control group from 2013 to 2014. Clinical features such as gender, age, body temperature, body weight in diagnosis, growth curves for age-gender-body weight, and laboratory data of blood test were compared.
Results
In non-operative group, total 94 patients who were treated successfully by the non-operative air reduction. In operative group, total 21 patients treated by surgical procedure. The age under 12 months, weight over upper 75 percentile group, increased segment neutrophil count, decreased hemoglobin level and lymphocyte count were significantly associated with a requirement for surgical procedure.
Conclusion
We conclude that younger age, higher weight percentile group, increased segment neutrophil, decreased hemoglobin and lymphocyte are the independent risk factors related to operative treatment for ileo-colic intussusception in children. If primary air reduction is failed in patients with such risk factors, operative treatment over ultrasonography or secondary reduction can prevent unnecessary effort and complications, thus emphasizing the consideration of operative treatment when selecting treatment methods.
Figures and Tables
References
1. Kim WS, Jeong JH, Lee JH, Park JK, Moon HJ, Shin HJ, et al. Clinical manifestations of childhood intussusception with ubiquitous ultrasonography: comparison with small bowel and ileocecal type. J Korean Assoc Pediatr Surg. 2011; 17:23–34.
2. Huppertz HI, Soriano-Gabarró M, Grimprel E, Franco E, Mezner Z, Desselberger U, et al. Intussusception among young children in Europe. Pediatr Infect Dis J. 2006; 25:1 Suppl. S22–S29.
3. Takeuchi M, Osamura T, Yasunaga H, Horiguchi H, Hashimoto H, Matsuda S. Intussusception among Japanese children: an epidemiologic study using an administrative database. BMC Pediatr. 2012; 12:36.
4. Ha H, Cho J, Park J. Risk factors associated with the need for operative treatment of intussusception in children. J Korean Assoc Pediatr Surg. 2014; 20:17–22.
5. Thurston DL, Holowach J, Mccoy EE. Acute intussusception; analysis of one hundred sixteen cases at St. Louis Children's Hospital. AMA Arch Surg. 1953; 67:68–79.
6. Peck DA, Lynn HB, Dushane JW. Intussusception in children. Surg Gynecol Obstet. 1963; 116:398–404.
7. Larsen E, Miller RC. Clinical aspects of intussusception. Am J Surg. 1972; 124:69–71.
8. Kim YJ, Kim CY. Factors related to the outcome of treatment of the intussusception in children. J Korean Pediatr Soc. 1993; 36:521–527.
9. Park BC, Kim SY, Jung SJ. A comparative analysis of clinical features and treatment outcomes of intussusception according to age distribution. Korean J Pediatr Gastroenterol Nutr. 2005; 8:150–156.
10. Son IT, Jung K, Park T, Kim HY, Park KW, Jung SE. Clinical features and factors affecting success rate of air reduction for pediatric intussusception. J Korean Assoc Pediatr Surg. 2010; 16:108–116.
11. Ramachandran P, Gupta A, Vincent P, Sridharan S. Air enema for intussusception: is predicting the outcome important? Pediatr Surg Int. 2008; 24:311–313.
12. Katz M, Phelan E, Carlin JB, Beasley SW. Gas enema for the reduction of intussusception: relationship between clinical signs and symptoms and outcome. AJR Am J Roentgenol. 1993; 160:363–366.
13. Lehnert T, Sorge I, Till H, Rolle U. Intussusception in children--clinical presentation, diagnosis and management. Int J Colorectal Dis. 2009; 24:1187–1192.
14. Fragoso AC, Campos M, Tavares C, Costa-Pereira A, Estevão-Costa J. Pneumatic reduction of childhood intussusception. Is prediction of failure important? J Pediatr Surg. 2007; 42:1504–1508.
15. Fike FB, Mortellaro VE, Holcomb GW 3rd, St Peter SD. Predictors of failed enema reduction in childhood intussusception. J Pediatr Surg. 2012; 47:925–927.
16. Tareen F, Ryan S, Avanzini S, Pena V, Mc Laughlin D, Puri P. Does the length of the history influence the outcome of pneumatic reduction of intussusception in children? Pediatr Surg Int. 2011; 27:587–589.
17. Reijnen JA, Festen C, van Roosmalen RP. Intussusception: factors related to treatment. Arch Dis Child. 1990; 65:871–873.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download