Abstract
Purpose
Laparoscopic appendectomy (LA) has become a gold standard for children even in complicated appendicitis. The purpose of this study was to compare the postoperative surgical site infection rates between laparoscopic and open appendectomy (OA) group in pediatric complicated appendicitis.
Methods
A total of 1,158 pediatric patients (age ≤15 years) underwent operation for appendicitis over a period of 8 years. Among these patients, 274 patients (23.7%) were diagnosed with complicated appendicitis by radiologic, operative and pathologic findings, and their clinical outcomes were retrospectively analyzed.
Results
Of the 274 patients with complicated appendicitis, 108 patients underwent LA and 166 patients underwent OA. Patients in the LA group returned to oral intake earlier (1.9 days vs. 2.7 days; p<0.01) and had a shorter hospital stay (5.0 days vs. 6.3 days; p<0.01). However, rate of postoperative intra-abdominal infection (organ/space surgical site infection) was higher in the LA group (LA 15/108 [13.9%] vs. OA 12/166 [7.2%]; p<0.01). Readmission rate was also higher in the LA group (LA 9/108 [8.3%] vs. OA 3/166 [1.8%]; p<0.01).
Conclusion
The minimally invasive laparoscopic technique has more advantages compared to the open procedure in terms of hospital stay and early recovery. However, intra-abdominal infection and readmission rates were higher in the laparoscopy group. Further studies should be performed to evaluate high rate of organ/space surgical infection rate of laparoscopic procedure in pediatric complicated appendicitis.
Laparoscopic appendectomy (LA) appears to be a safe alternative to open appendectomy (OA) for simple, non-perforated appendicitis, and even for complicated appendicitis, in adults [1,2]. LA for children retains the many advantages that other minimal access procedures offer, such as minimizing scarring, reducing pain and duration of hospital stay, as well as better diagnostic efficacy over an open technique.
However, some authors have reported an increased risk of intra-abdominal abscess (IAA) if LA is performed in pediatric complicated appendicitis [3,4,5]. Complicated appendicitis involves a larger proportion of pediatric appendicitis cases relative to adult cases. The postoperative morbidity rate is also higher for pediatric than adult patients due to distinct characteristics such as difficulty in diagnosing children, and the rapid progress of infectious processes within a smaller abdominal cavity [6]. Therefore, adequate judgment related to the appropriate management of pediatric complicated appendicitis is a substantial issue.
The hypothesis of this study was that a LA in a pediatric complicated appendicitis can increase the intra-abdominal infection rate (organ/space surgical site infection [SSI] rate). Therefore, we evaluated the operative variables, postoperative complications focused on the SSI, and readmission rates in cases of pediatric complicated appendicitis, and compared the results of laparoscopic versus OA.
All pediatric patient clinical records containing diagnosis of acute appendicitis, which occurred between January 2002 and January 2010 at Korea University Anam, Guro, and Ansan Hospitals, were retrieved from our institutional database under the certification of an institutional review board. For the purpose of this study, complicated appendicitis was defined as operative findings of a gangrenous or perforated appendix, with or without abscess formation, and confirmed by pathologic finding. Patients with generalized peritonitis were included. The exclusion criteria for complicated appendicitis were as follows. Patients with other co-morbidity or congenital disease and any other infectious disease, and patients with history of previous surgery were excluded in this study. A total of 1,158 pediatric patients (age ≤15 years) underwent operation for appendicitis over the of 8 year period. Among these patients, 274 patients (23.7%) were diagnosed with complicated appendicitis, and the outcomes of these cases were retrospectively analyzed.
All open and laparoscopic appendectomies were performed by surgeons with at least 5 years of surgical training and more than 2 years of laparoscopic training. The decision to perform either OA or LA was determined by the surgeon's preference. Under the general anesthesia, open surgery was performed through a Rocky-Davis or McBurney incision. Dissection, vessel ligation, resection of appendix and pus drainage was performed by conventional methods. The laparoscopic approach was performed with three-trocar approach (two 5 mm, one 11 mm), using monopolar dissectors and forceps. Pre-tied suture loops were used for stump closure, and pus drainage was performed by using suction-irrigation device. A closed suction drainage catheter was used in cases where generalized peritonitis, or remained abscess cavity after the adequate suction of the pus. All patients were given antibiotics (ampicillin/sulbactam or 3rd generation cephalosporin plus gentamycin or metronidazole or clindamycin) preoperatively and subsequently for 5-7 days after the operation. Antibiotics were given at the time of diagnosis and within 1 hour preoperatively. Then the antibiotics were postoperatively continued until clinical infection signs (abdominal tenderness, fever, and increased CRP) was discontinued. Readmission was defined as patient readmission within 30 days after initial surgery for abdominal complications related to the previous operation.
Statistical analysis was performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). The two groups are compared by unpaired t-test for continuous variables, or Fisher's exact test or chi-square test for discrete variables. A p-value <0.05 was considered significant.
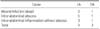
Of the 274 patients, 108 patients underwent LA, and 166 patients underwent OA. Their mean age was 9.7±3.4 years (LA 9.5±3.2 years vs. OA 10.2±3.5 years; p=0.92). There was no significant differences observed related to gender, body weight, initial leucocyte count and body temperature between the two groups (Table 1).
The operation time (LA 53.8±15.4 minutes vs. OA 48.8±11.4 minutes; p<0.01) was significantly longer in the LA group. Patients in the LA group returned to oral intake earlier (1.9±1.2 days vs. 2.7±1.3 days; p<0.01) and had a shorter hospital stay (5.0±2.1 days vs. 6.3±1.9 days; p<0.01) (Table 2).
The postoperative SSI rates between the two groups were not significantly different. However, the organ/space SSI rate was higher in the LA group (LA 15/108 [13.9%] vs. OA 12/166 [7.2%]; p<0.01) (Table 3). Readmission rate was also higher in the LA group (LA 9/108 [8.3%] vs. OA 3/166 [1.8%]; p<0.01) (Table 2).
The causes of readmission were IAA (n=6) and intra-abdominal inflammation (n=3) in the LA group. Most patients improved after treatment of intravenous antibiotics (tazobactam or 3rd generation of cephalosporin plus metronidazole). One patient needed percutaneous abscess drainage for the treatment of IAA (Table 4).
The advent of minimal access surgery, more and more pediatric surgeons have no scruples in adopting laparoscopic techniques for performance of various pediatric surgical procedures. The indisputable merits of laparoscopy over open techniques are reduced postoperative pain, reduced scarring, and earlier return of daily activity. Yet based on our results, laparoscopy also seems to have demerits including increased intra-abdominal inflammatory complications. This higher intra-abdominal inflammatory rate has also been observed in other studies [5,7,8].
The most intriguing result of our study was the higher rate of readmission of the LA group. Many previous reports comparing LA and OA did not analyze readmission rates [9,10,11]. The hospital stay of LA was 5 days in our study and less than 7 days in most other studies [10,11,12]. Taking account of the fact that IAA usually develops 7 to 10 days after surgery, late development of IAA can be missed if readmission is not analyzed during the data review period, especially in a retrospective study. In our study, most of the causes of readmission were intra-abdominal inflammation, with or without abscess formation. After laparoscopic surgery, surgeons tend to discharge the patient from the hospital earlier than for cases of open surgery. These results suggest that implementation of the LA procedure accompanies greater risk in producing early and late postoperative inflammatory complications than OA.
Postoperative abscess formation may occur anywhere in the peritoneal cavity, but the usual sites are the periappendicular, paracecal and pelvic collection. In the LA group in our study, atypical abscess formations in the splenic hilum and lesser sac were observed. These were likely due to spillage or spread of inflammation caused by the changing of patient positions that sometimes required during use of the LA procedure (Trendelenburg and right-up positions) for visualization, and also due to the effects of CO2 gas insufflation. However, considering the observation of frequent disturbance during LA caused by a distended bowel loop, where ileus is closely associated with complicated appendicitis, the position change during the laparoscopic procedure is sometimes required if completing LA without conversion to an open technique is desired. Therefore, after the laparoscopic diagnosis of complicated appendicitis, the surgeon should prudently determine whether to continue by the LA method, or not. Once the surgeon selects laparoscopic surgery, care should be performed in order to not necessitate position change, and surgery should be accompanied by copious four quadrants irrigation.
The increased intra-abdominal complications associated with LA may have resulted from the following reasons. First, the change of position during performance of LA and the insufflations of CO2 gas for the quadrant may be causes. In support of this reason, a recent animal study suggested that CO2 insufflation may promote the growth of intra-abdominal anaerobic bacteria and lead to IAA formation, or cause localized peritonitis to develop into generalized peritonitis [13].
The second possible reason for increased intra-abdominal complications associated with LA is the difficulty in effective irrigation of the abdomen, laparoscopically. We suspect the increased IAA rate has more to do with the difficulties associated with proper lavage than anything else. For small children, effective laparoscopic irrigation is difficult due to their small abdominal cavity, the low gas insufflation pressure, low gas flow rate, and distended small bowel which often occurs in complicated appendicitis. In small children, due to the small working space and relatively low abdominal gas pressure the suction during laparoscopy frequently collapses the abdominal cavity, leading to nonvisualization of the abdominal cavity. Some authors suggested copious irrigation of four quadrants and interloop areas with at least 3 L of sterile saline, leaving 300 to 500 mL of saline inside the peritoneal cavity at the end of the procedure, and also the application of a drain [14]. On the other hand, Wang et al. [10] has recommended irrigation using copious amounts of fluid containing metronidazole. However, recent studies compared irrigation versus suction alone in perforated appendicitis in children suggested that irrigation of peritoneal cavity has no advantage [15,16]. The effectiveness of peritoneal irrigation for complicated appendicitis and the adequate technical tips for laparoscopy should be fully evaluated and standardized through further studies.
The last reason for increased intra-abdominal complications associated with LA, is that the small abdominal cavity size associated with pediatric patients enables any infected contents contained within the cavity to spread more easily than in adults, possibly increasing the rate of the intra-abdominal inflammation. Therefore, more careful handling of the infected appendix should be conducted when intra-corporeal manipulation and resection of the appendix are performed for these small patients.
This study has several limitations. First, this is retrospective analysis and LA was determined by surgeon's preference. Another limitation is the use of postoperative antibiotics. All the patients received postoperative antibiotics; however, the type and duration of antibiotics were different according to the patient's condition. But our study differs from others, in evaluating the readmission rate as well as IAA rates to compare LA and OA. Postoperative inflammatory complications such as SSI can lead to readmission and increase the cost of treatment. If we want to pursue advanced laparoscopic techniques, we should work to strengthen the merits of the procedure and simultaneously compensate for the weaknesses. A well-designed analysis, focused on intra-abdominal complications should be performed to verify these results.
In conclusion, the minimally invasive laparoscopic technique has several advantages compared to an open procedure. However, organ/space SSI rate and readmission rate were higher in the laparoscopy group. Further study should be performed to clarify this result.
Figures and Tables
References
1. Sauerland S, Jaschinski T, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2010; (10):CD001546.
2. Park HC, Yang DH, Lee BH. The laparoscopic approach for perforated appendicitis, including cases complicated by abscess formation. J Laparoendosc Adv Surg Tech A. 2009; 19:727–730.
3. Langer JC, Albanese CT. Pediartric minimal access surgery. Boca Raton: Taylor & Francis;2005.
4. Simon P, Burkhardt U, Sack U, Kaisers UX, Muensterer OJ. Inflammatory response is no different in children randomized to laparoscopic or open appendectomy. J Laparoendosc Adv Surg Tech A. 2009; 19:Suppl 1. S71–S76.
5. Markar SR, Blackburn S, Cobb R, Karthikesalingam A, Evans J, Kinross J, et al. Laparoscopic versus open appendectomy for complicated and uncomplicated appendicitis in children. J Gastrointest Surg. 2012; 16:1993–2004.
6. Morrow SE, Newman KD. Current management of appendicitis. Semin Pediatr Surg. 2007; 16:34–40.
7. Sauerland S, Lefering R, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2002; (1):CD001546.
8. Aziz O, Athanasiou T, Tekkis PP, Purkayastha S, Haddow J, Malinovski V, et al. Laparoscopic versus open appendectomy in children: a meta-analysis. Ann Surg. 2006; 243:17–27.
9. Menezes M, Das L, Alagtal M, Haroun J, Puri P. Laparoscopic appendectomy is recommended for the treatment of complicated appendicitis in children. Pediatr Surg Int. 2008; 24:303–305.
10. Wang X, Zhang W, Yang X, Shao J, Zhou X, Yuan J. Complicated appendicitis in children: is laparoscopic appendectomy appropriate? A comparative study with the open appendectomy--our experience. J Pediatr Surg. 2009; 44:1924–1927.
11. Pham VA, Pham HN, Ho TH. Laparoscopic appendectomy: an efficacious alternative for complicated appendicitis in children. Eur J Pediatr Surg. 2009; 19:157–159.
12. Yau KK, Siu WT, Tang CN, Yang GP, Li MK. Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg. 2007; 205:60–65.
13. Sare M, Demirkiran AE, Tastekin N, Durmaz B. Effects of laparoscopic models on anaerobic bacterial growth with bacteroides fragilis in experimentally induced peritonitis. J Laparoendosc Adv Surg Tech A. 2003; 13:175–179.
14. Hussain A, Mahmood H, Nicholls J, El-Hasani S. Prevention of intra-abdominal abscess following laparoscopic appendicectomy for perforated appendicitis: a prospective study. Int J Surg. 2008; 6:374–377.
15. St Peter SD, Adibe OO, Iqbal CW, Fike FB, Sharp SW, Juang D, et al. Irrigation versus suction alone during laparoscopic appendectomy for perforated appendicitis: a prospective randomized trial. Ann Surg. 2012; 256:581–585.
16. Moore CB, Smith RS, Herbertson R, Toevs C. Does use of intraoperative irrigation with open or laparoscopic appendectomy reduce post-operative intra-abdominal abscess? Am Surg. 2011; 77:78–80.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download