This article has been corrected. See "Erratum to: Evaluation of sHLA-G levels in serum of patients with prostate cancer identify as a potential of tumor marker" in Volume 50 on page 162.
Abstract
Prostate cancer is the most common cancer type in men and is the second cause of death, due to cancer, in patients over 50, after lung cancer. Prostate specific antigen (PSA) is a widely used tumor marker for prostate cancer. Recently, PSA is discovered in non-prostatic cancer tissues in men and women raising doubts about its specificity for prostatic tissues. PSA exists in low serum level in healthy men and in higher levels in many prostate disorders, including prostatitis and prostate cancer. Thus, a supplementary tumor marker is needed to accurately diagnose the cancer and to observe the patient after treatment. Recently, soluble human leukocyte antigen-G (sHLA-G) has been introduced as a new tumor marker for different cancer types, including colorectal, breast, lung, and ovary. The present descriptive-experimental study was carried out including patients with malignant prostate tumor, patients with benign prostate tumor, and a group of health men as the control group, as judged by an oncologist as well as a pathologist. After sterile blood sampling, sHLA-G was measured by enzyme-linked immunosorbent assay in each group. The data was then analyzed using one-way ANOVA. P≤0.05 was considered as statistically significant. The results showed that the mean of sHLA-G level was high in patients. Also, it was found that there was a significant difference in sHLA serum level between the three groups. The data revealed that sHLA-G can be a novel supplementary tumor marker in addition to PSA to diagnose prostate cancer.
Prostate cancer is the most common cancer in middle-aged and elderly men after lung cancer with the prevalence of 25.3 per 10,000. The previous studies have shown that one man in six will suffer from this cancer during his lifetime. Genetic, hormonal, and environmental factors are known to be involved in the incidence of this cancer. It is most prevalent in the Northern Europe and Africa, and the least incidence is reported in the Asian population [12].
Screening, diagnosis, and treatment in the early stages of prostate cancer can improve the patients' life expectancy and quality of life and decrease morbidity and mortality [3]. Digital rectal examination and serum prostate specific antigen (PSA) measurement are the main diagnostic methods [4].
PSA is a proteolytic enzyme released by normal and neoplastic prostate cells. Any damage to prostate, including hyperplasia, adenocarcinoma, cystoscopy, prostatitis, and senility, has been reported to increase the serum level of this antigen; however, this antigen is widely used to diagnose prostate cancer [567].
This specific antigen is in a higher level in patients with prostate cancer although it does not necessarily indicate affliction to it as high level of PSA is also observed in many men with benign hyperplasia of prostate and urinary tract infections. To confidently diagnose prostate cancer, PSA measurement is followed by further tests including magnetic resonance imaging, computed tomography, ultrasound, and prostate biopsy. However, about 25% of prostate cancer is not diagnosed after first biopsy [8].
The previous studies have shown that despite the negative result of biopsy, PSA level increases, but in a few percentages of gland lesions, the level of PSA does not increase.
Therefore, considering the restriction and the low diagnostic accuracy of screening methods, finding a reliable method of diagnosis is significant [9]. Recently, human leukocyte antigen-G (HLA-G) has been introduced as a tumor marker for breast cancer, lung cancer, skin cancer, ovarian cancer, and gastrointestinal cancer [10]. It is shown that the evaluation of HLA-G level in serum or plasma can increase specificity of diagnosis [111213].
The present study is an attempt to evaluate the level of this tumor marker in comparison with the pathological findings in patients suffering from prostate cancer and to assess its efficiency as a new biomarker for screening purposes.
The present descriptive-experimental study was carried out in Nowshahr Medical Diagnostic Institute (Feb 2014–Jan 2015). First, among the patients who had referred to the laboratory, those with prostate cancer who met the inclusion criteria were selected and informed about the study. Prior to biopsy procedure, all the participants wrote and signed the consent form and their familial history was elicited.
Inclusion criteria were patients with benign or acute prostate cancer, approval of the cancer stage by an oncologist and a pathologist, and no history of other diseases. Patients whose cancer stage was unknown were excluded from the study.
Participants were divided into three groups: group 1 included 26 patients with acute prostate cancer; group 2 included 26 patients with benign prostate cancer; and group 3, comprised of 26 healthy participants. Two milliliters of blood was sampled from each participant. After separating serum in sterilized condition, the levels of biomarkers were measured in the three groups using Human AHLA-G ELISA Kit (Elabscience-Biotechnology, Wuhan, China). The data was analyzed by one-way analysis of variance (ANOVA) with significance set at P<0.05.
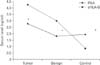
The statistical analyses revealed that the levels of PSA in malignant group, benign group, and control group were 3.45, 2.88, and 2.31, respectively, showing no statistically significant different between the groups (P<0.05) (Fig. 1). The highest level of PSA was found in the malignant group. The results of measuring HLA-G level were 1.68, 1.59, and 0.83 in malignant tumor group, benign tumor group, and control group, respectively, demonstrating a statically significant different between the three groups (P<0.05) (Fig. 2). The highest level of HLA-G was found in the group with malignancy. Also, when the mean of the serum level of PSA was compared with that of the serum level of HLA-G, no significant difference was observed between the three groups (P<0.05) (Fig. 3).
The aim of the present study was to evaluate serum level of HLA-G as an efficient tumor marker in screening and diagnosis of patients with prostate cancer and also to compare HLA-G and PSA in terms of their biomarker role. The serum level of PSA was abnormal in patients who suffered from prostate cancer, but no significant difference was observed between the malignant group and benign group with regard to the level of this biomarker. Moreover, the mean of the serum level of HLA-G was found to be high in the three groups. The results of the statistical analyses showed that there is a significant difference between the three groups of study concerning the serum level of HLA-G with the highest level belonging to the malignant tumor group and the least level to the control group; therefore, it can be stated that there is a positive correlation between the serum level of HLA-G and the stage of cancer. Evaluation of PSA level is routinely used in laboratories for screening prostate cancer where increase in the serum level of this antigen is interpreted as increase in the severity of the disease, yet according to our findings, there is no correlation between the disease, cancer stage, and the serum level of PSA.
HLA-G is one of the molecules of MHC I that plays the roles of immunosuppression and regulatory of natural killer cell and dendritic cell T-cell [10]. Previous studies have reported on the clinical linkage between an increase in expression of HLA-G in diseases such as cancer, viral infection, pregnancy, organ transplants, autoimmune disease, and inflammations. HLA-G expression were found, for the first time, in trophoblastic cell in chorion playing fundamental roles in protecting fetus against mother's immune system, survival of the fetus, and early stages of placenta angiogenesis [13]. Also, HLA-G has been detected in people receiving allograft and tumor progression in several cancers [14]. Similar to our findings, Wang et al. [15] has reported that there is positive a correlation between expression of HLA-G and size of glioma tumor. In another study, Guo et al. [16], after evaluation of the expression of HLA-E or HLA-G in patients with colorectal cancer, concluded that there is a direct relationship between HLA-G or HLA-E and metastasis rate and mortality.
In 2006, expression of HLA-G1, -G2, -G5, and -G6 were evaluated in normal prostate tissue, prostate hyperplasia, and prostate adenocarcinoma by Langat et al. [17]. They reported that HLA-G5 exists in prostate tissue and it increases in tissue secretion of prostate adenocarcinoma.
According to findings of the present study, the evaluation of serum level of HLA-G can be used as a novel and an easy method for screening, diagnosis, and staging of prostate cancer, as early diagnosis of prostate cancer can decrease morbidity and mortality and increase life expectancy in the patients.
Figures and Tables
Fig. 1
Mean and standard deviation of prostate specific antigen (PSA) level in malignant group, benign group, and control group (P<0.01).

References
1. Miyahira AK, Lang JM, Den RB, Garraway IP, Lotan TL, Ross AE, Stoyanova T, Cho SY, Simons JW, Pienta KJ, Soule HR. Multidisciplinary intervention of early, lethal metastatic prostate cancer: report from the 2015 Coffey-Holden Prostate Cancer Academy Meeting. Prostate. 2016; 76:125–139.
2. Roussel B, Ouellet GM, Mohile SG, Dale W. Prostate cancer in elderly men: screening, active surveillance, and definitive therapy. Clin Geriatr Med. 2015; 31:615–629.
3. Carter HB. American Urological Association (AUA) guideline on prostate cancer detection: process and rationale. BJU Int. 2013; 112:543–547.
4. Qaseem A, Barry MJ, Denberg TD, Owens DK, Shekelle P. Clinical Guidelines Committee of the American College of Physicians. Screening for prostate cancer: a guidance statement from the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med. 2013; 158:761–769.
5. Murthy V, Rishi A, Gupta S, Kannan S, Mahantshetty U, Tongaonkar H, Bakshi G, Prabhash K, Bhanushali P, Shinde B, Inamdar N, Shrivastava S. Clinical impact of prostate specific antigen (PSA) inter-assay variability on management of prostate cancer. Clin Biochem. 2016; 49:79–84.
6. Ammannagari N, Javvaji C, Danchaivijitr P, George S. Dramatic PSA increase with tumor shrinkage after initiating degarelix in advanced prostate cancer. Clin Genitourin Cancer. 2016; 14:e123–e125.
7. van Iersel MP, Witjes WP, Thomas CM, Segers MF, Oosterhof GO, Debruyne FM. Review on the simultaneous determination of total prostate-specific antigen and free prostate-specific antigen. Prostate Suppl. 1996; 7:48–57.
8. Bjurlin MA, Rosenkrantz AB, Beltran LS, Raad RA, Taneja SS. Imaging and evaluation of patients with high-risk prostate cancer. Nat Rev Urol. 2015; 12:617–628.
9. Zigeuner R, Schips L, Lipsky K, Auprich M, Salfellner M, Rehak P, Pummer K, Hubmer G. Detection of prostate cancer by TURP or open surgery in patients with previously negative transrectal prostate biopsies. Urology. 2003; 62:883–887.
10. Rouas-Freiss N, Moreau P, LeMaoult J, Carosella ED. The dual role of HLA-G in cancer. J Immunol Res. 2014; 2014:359748.
11. Zidi I, Ben Amor N. HLA-G regulators in cancer medicine: an outline of key requirements. Tumour Biol. 2011; 32:1071–1086.
12. Yie SM, Hu Z. Human leukocyte antigen-G (HLA-G) as a marker for diagnosis, prognosis and tumor immune escape in human malignancies. Histol Histopathol. 2011; 26:409–420.
13. Kovats S, Main EK, Librach C, Stubblebine M, Fisher SJ, DeMars R. A class I antigen, HLA-G, expressed in human trophoblasts. Science. 1990; 248:220–223.
14. LeMaoult J, Daouya M, Wu J, Loustau M, Horuzsko A, Carosella ED. Synthetic HLA-G proteins for therapeutic use in transplantation. FASEB J. 2013; 27:3643–3651.
15. Wang Y, Fan X, Li H, Lin Z, Bao H, Li S, Wang L, Jiang T, Fan Y, Jiang T. Tumor border sharpness correlates with HLA-G expression in low-grade gliomas. J Neuroimmunol. 2015; 282:1–6.
16. Guo ZY, Lv YG, Wang L, Shi SJ, Yang F, Zheng GX, Wen WH, Yang AG. Predictive value of HLA-G and HLA-E in the prognosis of colorectal cancer patients. Cell Immunol. 2015; 293:10–16.
17. Langat DK, Sue Platt J, Tawfik O, Fazleabas AT, Hunt JS. Differential expression of human leukocyte antigen-G (HLA-G) messenger RNAs and proteins in normal human prostate and prostatic adenocarcinoma. J Reprod Immunol. 2006; 71:75–86.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download