Abstract
During the strengthening and weakening procedures of intraocular muscles, distance of insertion from the sclerocorneal junction is an important determinant in the identification of muscles. During repositioning of the aponeurosis of the muscles, it is desired that the width should not change in order to avoid diversion of forces. Available anatomic studies on insertions of extraocular muscles are few, date back to early twentieth century and have been conducted on mostly white population. The present study is an attempt to document the insertions of recti and oblique muscles in Indian population. Forty eyeballs were removed from orbit. Insertion of recti and obliqui were cleaned and eyeballs were perfused with normal saline to regain the volume (hence shape and size) before recording observations. Insertion of recti and obliqui muscles were observed under various study parameters. The distance of insertion of recti from the limbus were found to be 7.3 mm, 8.06 mm, 8.71 mm, and 8.74 mm for medial, inferior, lateral, and superior rectus, respectively. The superior oblique was aponeurotic and found to be more variable in mode of insertion as compared to inferior oblique which had a fleshy and relatively constant insertion. The observations on insertion of recti and obliqui as obtained in present study differ from earlier studies to the tune of 1-1.5 mm. This may be attributed to adoption of method of reperfusion of eyeball before recording observations thus maintaining size close to in vivo. The observations are expected to be closer to actual.
Coordinated movements of eyeballs are important for binocular vision. These movements are brought by extraocular muscles. There are four recti muscles namely medial rectus, inferior rectus, lateral rectus, superior rectus, and two oblique muscles, i.e., inferior oblique, superior oblique [12]. An imaginary line joining the insertions of four recti forms a spiral pattern and is called spiral of Tillaxus. The precise location of insertions of these muscles is an important anatomical landmark while performing strabismus surgeries [3].
With advancement in diagnostic and treatment modalities, strabismus or squint surgeries have become more common. Apparent weakness or over action of any extraocular muscle on clinical examination is an indication of surgical intervention [4]. The aim of squint surgeries on extraocular muscles is to correct misalignment. Three types of surgical procedures are carried out in squint surgeries: (1) weakening-which decreases the pull of a muscle; (2) strengthening-which enhances the pull of a muscle; (3) procedures that changes the direction of muscle actions [3]. These procedures involve detachment and subsequent repositioning of insertion of muscles.
Forty eyeballs (20 right and 20 left) obtained from male adult embalmed cadavers from the collection of the Department of Anatomy were utilized for the study.
The cranial cavity was opened by cutting out the skull vault. After removal of brain the roof of the orbit was cut open to expose the contents. The neurovascular structures were cut near the apex of the orbit and the origins of extraocular muscles were also cut. Superior and inferior conjunctival fornices were incised to deliver the eyeball from the anterior aspect. The eyeballs were thoroughly cleaned and periocular connective tissue was removed. The insertions of the extraocular muscles were cleaned. Eyeballs were injected with the normal saline to maintain the integrity and shape of the eyeballs before taking the measurements (Fig. 1). This was required as it was observed that removal of eye balls from the orbit and cleaning of insertion involved handling of eyeball. Moreever cutting of vessels and nerves entering the eyeball left leakage points. The above two maneuvers resulted in leakage of fluid from within the eyeball causing distortion in shape and size and shrinkage. Following measurements were obtained:
- Distance of recti from limbus (sclerocorneal junction)
- Width of insertion of recti
- Length of aponeurosis of recti
- Distance between insertion of adjacent recti muscles
- Width of insertion of superior oblique and inferior oblique
- Minimum distance between insertions of superior oblique and inferior oblique
All the measurements were recorded by standard digital vernier caliper. The data obtained was tabulated and analyzed for descriptive statistics. Paired sample t test was applied to find the statistical difference between the right and left side. SPSS software (SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
Table 1 shows descriptive statistics of different study parameters of rectus muscles. It was observed that the distance of insertions from the limbus gradually increased from medial rectus to superior rectus and was quite variable (wide range).
The distance between the insertions also increased clock-wise from medial rectus to superior rectus. The aponeurosis of medial rectus was shortest and that of lateral rectus was longest.
Table 2 shows descriptive statistics of insertion of oblique muscles. The superior oblique aponeurosis fanned out to be inserted beneath the superior rectus muscle. Fig. 2 shows various modes of insertion of superior oblique muscle with respect to superior rectus. Insertion of inferior oblique muscle was always fleshy. The muscle mostly inserted deep to the lateral rectus muscle except in six cases (4 right and 2 left) where part of insertion projected above the superior border of lateral rectus.
Strabismus surgeries necessitate precise knowledge of insertions of extraocular muscles. Various surgical procedures like weakening or strengthening utilize the distance of insertion from the limbus as an important landmark.
The present study has documented the measurements of insertions of recti and oblique in Indian population.
Findings of the present study on distance from the limbus are higher to the tune of 1 to 1.5 mm as compared to earlier studies (Table 3). There are no comparable findings in Indian population. The outcomes of the present study on width of insertions were about 1 to 1.5 mm less than earlier studies (Table 3). The distances between the insertions of adjacent recti were slightly higher than the earlier studies (Table 4).
Following points are noteworthy in regards to difference of findings of present study as compared to others:
(1) Most of the studies have been performed on white population.
(2) Precise methodology followed for measurement has not been described except by Apt [5]. He utilized eyeballs obtained from autopsy specimen that were fixed in formalin for five days followed by treatment with alcohol. However volume changes are bound to occur in any postmortem tissue, moreover shrinkage of tissue is known to occur after fixation in formalin and dehydration in alcohol. There is no mention of methodology in other studies. Observations by Sevel [6] are not comparable as they were recorded on fetal eyeballs.
(3) Besides racial distinction, authors wish to attribute this difference to the methodological dissimilarity. Authors observed that cleaning of the insertions of recti and obliqui and removal of the periorbital connective tissue required lot of handling of the eyeball. This resulted in leakage of fluid from the cut ends of neurovascular entry points in the eyeballs. This aspect was taken care in present study by perfusion of fluid, after cleaning the eyeball, for achieving the volume (and hence the size) of the eye ball as in living condition. Sclera is an indistensible tissue [7] hence possibility of stretching because of over perfusion is ruled out.
The length of aponeurosis of the lateral rectus muscle was longest and almost double the length of aponeurosis of other recti. The knowledge of lengths of aponeurosis will be of surgical importance as these are relatively avascular. Longer aponeurosis of lateral rectus may be due to longer lateral rectus muscle. Because of the obliquity of the eyeball, the distance of the insertion of lateral rectus from the origin of recti is longer and hence, longer aponeurosis. This fact has not received any mention in the available literature.
In a histological study of the lateral and medial recti, Jaggi et al. [8] have observed that there are no aponeurosis in the recti muscles and the muscle fibers are directly inserted on to the sclera. A naked eye examination however clearly indicates the insertion to be predominantly aponeurotic.
The aponeurosis of superior oblique was very variable in its position and extent. The range of width of its insertion was wide [8]. During eye surgeries identification of superior oblique is a tricky task. The position of superior oblique muscle with respect to the superior rectus can be a good guide for identification.
The findings of the present study may aid ophthalmologist during strabismus surgeries. The study also indicates towards need to reevaluate the insertion in vivo.
Figures and Tables
Fig. 1
Showing insertions of rectus muscles and various study parameters. a1, a2, a3, and a4 represent distance of insertion from limbus of SR, MR, IR, and LR, respectively. b1, b2, b3, and b4 represents width of insertions of SR, MR, IR, and LR, respectively. c1, c2, c3, and c4 represent distance between adjacent recti, respectively. MR, medial rectus; IR, inferior rectus; LR, lateral rectus; SR, superior rectus.

Fig. 2
Shows different pattern of insertion of SO with respect to SR. SO, superior oblique; SR, superior rectus; L, lateral; M, medial.

Table 1
Descriptive statistics of various study parameters of the rectus muscles
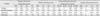
Table 2
Descriptive statistics of various study parameters of the oblique muscles

Table 3
The comparisons of various study parameters between present and other studies

| Variable | Distance of insertion of recti from limbus (mm) | Width of insertion of recti from limbus (mm) | ||||
|---|---|---|---|---|---|---|
| Apt (1980) [5] | Other studiesa) | Present study | Apt (1980) [5] | Other studiesb) | Present study | |
| MR | 3.3-6.4 | 5.05-5.7 | 6.21-10.85 | 9.6-13.3 | 10.30-10.76 | 7.32-11.41 |
| IR | 3.9-7.6 | 6.4-6.85 | 6.94-10.7 | 8.8-12.8 | 9.8-10.35 | 6.41-10.01 |
| LR | 4.8-7.9 | 6.6-7.4 | 6.94-10.7 | 8.8-12.5 | 9.2-9.65 | 6.8-11.6 |
| SR | 5.0-8.0 | 7.1-8.01 | 7.09-10.9 | 9.8-14.0 | 10.02-10.75 | 7.25-11.89 |
Table 4
The comparisons of distance (mm) between insertions of adjacent recti between present and Apt (1980) [5]

| Distance between adjacent recti | Present study | Apt (1980) [5] | Other studiesa) |
|---|---|---|---|
| MR-IR | 5.56-9.87 | 4.5-8.9 | 5.5 |
| IR-LR | 5.15-10.83 | 4.1-9.6 | 7.0-9.0 |
| LR-SR | 6.13-10.76 | 5.0-9.6 | 6.5-8.0 |
| SR-MR | 5.57-10.73 | 5.6-9.5 | 7.0-8.0 |
MR, medial rectus; IR, inferior rectus; LR, lateral rectus; SR, superior rectus. a)Duke-Elder and Wybar (1961) and Renard et al. (1965) as quoted by Apt (1980) [5].
References
1. Standring S, Ellis H, Healy JC, Johnson D, Williams A, Collins P, Wigley C. Gray's anatomy: the anatomical basis of clinical practice. 39th ed. London: Churchill Livingstone;2005. p. 91–694.
2. Last RJ. Anatomy, regional and applied. 7th ed. Edinburgh: Churchill Livingstone;1984. p. 432–440.
3. Kanski JJ. Clinical ophthalmology: a systematic approach. 6th ed. London: Elsevier Butterworth-Heinemann;2007. p. 780–782.
4. Roper-Hall G, Cruz OA, Chung SM. Results of extraocular muscle surgery in WEBINO bilateral internuclear ophthalmoplegia patients. J AAPOS. 2008; 12:277–281.
5. Apt L. An anatomical reevaluation of rectus muscle insertions. Trans Am Ophthalmol Soc. 1980; 78:365–375.
6. Sevel D. The origins and insertions of the extraocular muscles: development, histologic features, and clinical significance. Trans Am Ophthalmol Soc. 1986; 84:488–526.
7. Khurana AK. Comprehensive ophthalmology. 3rd ed. New Delhi: New Age International Publishers;2003. p. 127.
8. Jaggi GP, Laeng HR, Müntener M, Killer HE. The anatomy of the muscle insertion (scleromuscular junction) of the lateral and medial rectus muscle in humans. Invest Ophthalmol Vis Sci. 2005; 46:2258–2263.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download