Abstract
The review article attempts to focus on the practice of human cadaveric dissection during its inception in ancient Greece in 3rd century BC, revival in medieval Italy at the beginning of 14th century and subsequent evolution in Europe and the United States of America over the centuries. The article highlights on the gradual change in attitude of religious authorities towards human dissection, the shift in the practice of human dissection being performed by barber surgeons to the anatomist himself dissecting the human body and the enactment of prominent legislations which proved to be crucial milestones during the course of the history of human cadaveric dissection. It particularly emphasizes on the different means of procuring human bodies which changed over the centuries in accordance with the increasing demand due to the rise in popularity of human dissection as a tool for teaching anatomy. Finally, it documents the rise of body donation programs as the source of human cadavers for anatomical dissection from the second half of the 20th century. Presently innovative measures are being introduced within the body donation programs by medical schools across the world to sensitize medical students such that they maintain a respectful, compassionate and empathetic attitude towards the human cadaver while dissecting the same. Human dissection is indispensable for a sound knowledge in anatomy which can ensure safe as well as efficient clinical practice and the human dissection lab could possibly be the ideal place to cultivate humanistic qualities among future physicians in the 21st century.
Human cadaveric dissection has been used as the core teaching tool in anatomy for centuries [1]. This review article attempts to focus on the significant events in the history of human cadaveric dissection. The article begins with the inception of human dissection in ancient Greece during the 3rd century BC, tries to underline the factors leading to its disappearance in the Middle Ages and subsequent revival in the early 14th century Italy. It traces the gradual change in attitude of religious authorities towards human dissection from being the primary dissuader to playing the role of mediator (when human dissection was strictly practiced within the boundaries of European universities) to accepting human dissection for teaching anatomy, which turned dissection sessions into public events. The article also emphasizes on the shift from the practice of dissection being performed by barber surgeons (prevalent from the time of Mondino de Liuzzi) to the anatomist himself dissecting the cadaver, a move triggered by Andreas Vesalius. Particularly the article focuses on the means of cadaver procurement which began with dissecting bodies of executed criminals (when human dissection was synonymous with capital punishment), then anatomists had to depend on illegal means such as grave robbing, body snatching and even murder for human bodies, which led to legalization of the use of unclaimed bodies, most of whom were poor people stationed in workhouses, to curb unethical practices (when dissection was perceived as a penalty for poverty) and eventually relying on the body donation programs as the primary source of human bodies for anatomical dissection in medical schools. Finally this review reflects on the relevance of human dissection in the 21st century, when researchers are coming up with findings affirming that human dissection contributes to the improvement of anatomic knowledge which could be the key to safe medical practice [23].
The introduction of systemic human cadaveric dissection is a remarkable moment in the history of science. For many centuries, physicians of ancient Greece gained considerable information about human body and health [4]. The development of Greek medicine culminated with the establishment of the school of Greek medicine in Alexandria during the 3rd century BC [5]. In Alexandria the practice of human cadaveric dissection was the dominant means of learning anatomy and it was here that Herophilus of Chalcedon and his younger contemporary Erasistratus of Ceos became the first ancient Greek physicians to perform systematic dissections of human cadavers in the first half of 3rd century BC [6]. Before these two legendary Greek physicians, relatively superficial surgical incisions and excisions prompted by pathological conditions constituted the limit of exploring human bodies. Available literature suggests that religious moral and esthetic taboos as well as their psychological concomitants inhibited ancient physicians from opening the human body for anatomical purposes [7]. The factors that could have encouraged Herophilus and Erasistratus to overcome the deeply entrenched beliefs and cultural habits included royal patronage whereby bodies of executed criminals were handed over to them for their scientific endeavour as the ambition of Greek rulers was to establish Alexandria as a glittering centre of literary and scientific learning. Moreover the environment in Alexandria which was mostly inhabited by cosmopolitan intelligentsia committed to literary and scientific frontiermanship could have contributed to their success [8]. However, after the death of Herophilus and Erasistratus, human dissection went into oblivion not only in Alexandria but from all of subsequent ancient Greek science [7]. This could possibly be attributed to the emergence of a new rival school of medical thought, probably founded by a renegade pupil of Herophilus, Filinos of Cos. His followers were referred to as "empiricists" and they considered that human dissection had no scientific utility in anatomy teaching and that desirable clinical results could be obtained by empirical collection of non-invasive, even random observations [6]. Moreover in the generations after Herophilus and Erasistratus, physicians in Alexandria turned increasingly to detailed clinical analyses of texts from past and to the collection and criticism of precursor's views while abandoning human dissection [7]. The flickering light of human dissection was completely snuffed out with the burning of Alexandria in 389 AD [4]. Following widespread introduction of Christianity in Europe during the Middle Ages, the development of rational thought and investigation was paralysed by the church authorities and physicians could only repeat the works of the eminent figures from past such as Aristotle or Galen, without questioning their scientific validity [9]. During this period, human dissection was considered to be blasphemous and so was prohibited [10]. For hundreds of years, the European world valued the sanctity of the church more than scientific quest and it was not until early 14th century that human dissection was revived as a tool for teaching anatomy in Bologna, Italy after a hiatus of over 1,700 years [11].
In Medieval Europe, considerable advances in the field of science could only be achieved during the 12th century and early 13th century, with the setting up of universities in Paris (1150), Bologna (1158), Oxford (1167), Montpellier (1181) and Padua (1222) [12]. From 12th century onwards, the church did not forbid human dissection in general; however, certain edicts were directed at specific practices [13]. One of the significant proscriptions that Pope Alexander III enunciated at the Council of Tours in 1163 was the prohibition of clerics to involve themselves in the studies of physical nature and the canon (directive) was named as "Ecclesia abhorret a sanguine" meaning "The church abhors blood." This was misinterpreted as a ban which prevented clerics from practising surgery or studying anatomy [14]. The Holy Roman emperor Frederick II (1194-1250) took significant measures towards the progress of science which reflected his free thinking outlook. In 1231, he issued a decree which mandated that a human body should be dissected at least once in every five years for anatomical studies and attendance was made compulsory for everyone who was to practice medicine or surgery [15]. This initiative was a giant step towards revival of human dissection in the domain of anatomical sciences and towards the later part of the thirteenth century, the realization that human anatomy could only be taught by the dissection of human body resulted in its legalisation in several European countries between 1283 and 1365 [16]. The new found enthusiasm in human dissection ceased for a short period from about 1299, when Pope Boniface VIII issued a Papal Bull entitled, "De sepolturis" which forbade manipulation of corpses and their reduction to bones. The Bull was aimed to stop the dismemberment of the cadavers and prohibit the trade that had developed involving bones from soldiers killed in Holy wars. It was not meant to impede human dissection and although it stopped the practice of dissection in some of the European countries, did not have any significant impact on the anatomical activities in Italy [17]. By the end of 13th century, the University of Bologna emerged as the most popular institution in Europe for learning medicine, attracting students from the whole of Italy and many other countries [18]. The status of Bologna was further bolstered when it was granted a Bull by Pope Nicolas II in 1292, whereby all students having graduated in medicine from the University were permitted to teach all over the world [19]. All these events ultimately culminated in the first officially sanctioned systemic human dissection since Herophilus and Erasistratus, being performed in full public display by Mondino de Liuzzi (1275-1326) in 1315 in Bologna [11]. The dissection was performed on an executed criminal, probably female and marked its return in the educational setting to study and teach anatomy [20]. The fact that an Italian university was the platform for the revival of human dissection after a prolonged hiatus in Europe, could be attributed to the efforts of emperor Frederick II and Pope Nicolas II. Although there is a possibility that human dissections may have been performed prior to De Liuzzi, most authors suggests that all those cases actually involved autopsies and post-mortems and the first such recorded case in Italy of a human body being opened for investigating the cause of death dates back to 1286 [1721]. During the early 14th century, the religious restraints imposed on dissection and autopsy relaxed significantly though the practice of dissection remained limited [22]. No longer was the church the primary dissuader of anatomical studies, instead public condemnation became the primary obstacle. However the mediating role of the church played a critical role in appeasing the people's social and religious consciences. Religious authorities gave permission as well as clearly delineated and articulated boundaries around the practice of human dissection-this consequently eased the public's anxiety and the procedures were allowed to continue with ever decreasing protests [23]. From De Liuzzi's time human dissections were conducted in the form of regular university sponsored anatomy teaching sessions comprising of four day exhibitions held once or twice a year and were performed on bodies of executed criminals, both male and female, provided to the medical school of Bologna by the local public authorities [9]. These public dissections were strictly standardized as they required the presence of the Lector (lecturer), who read from an authoritative text (usually the Lector was De Liuzzi who referred to Galen's text and later on other eminent anatomists who referred to De Liuzzi's text Anathomia Mondini), the Ostensor who pointed to the part of the body to be dissected and the Sector (surgeon/barber) who performed the dissection (Fig. 1). The whole exercise blindly followed the written text without any attempt to look into the real anatomy visible in the human cadaver which could be due to the fact that the anatomist (the Lector) did not have a close view of the dissected body [24]. However during this period unofficial dissections were also carried out in private houses, which involved informal anatomy teaching between a lecturer and his small group of students [12]. Procurement of cadavers for such private dissections was really difficult and may have led to some malpractice as in 1319 four students of Master Alberto, who was a lecturer at the University of Bologna, were prosecuted for robbing a grave and bringing the corpse to the house where Alberto lectured [17]. Over the course of the 14th century human cadaveric dissection became increasingly common, spreading rapidly to other northern Italian cities. During the middle of 14th century, Universities of Perugia, Padua and Florence made it mandatory to attend at least one dissection for candidates to receive the doctorate degree in medicine [25]. Such measures were also adopted by medical schools across Italy. This led to shortage of cadavers available for public dissection by the onset of 15th century as executions were few in number in Italian cities. Consequently the students attending the dissection in medical schools were required to pay for and also attend the subsequent funeral of the corpse after dissection to encourage local families to offer their dead for anatomical studies. Nevertheless the problem of supply did not appear critical as dissection as a medium of teaching/learning anatomy did not become overwhelmingly popular during the 15th century [26]. In those days dissections functioned like an extension of anatomical illustration and its goal was not to add to the existing body of knowledge concerning human anatomy but to help students and physicians remember the text in which the knowledge was enclosed [27]. However the situation changed dramatically towards the end of 15th century with a remarkable flowering of interest in anatomical studies particularly human dissection. The reasons for this new found enthusiasm in human dissection were the revival of antique art in renaissance Italy with its interest in naturalism, rise of humanist faith in classical scholarship leading to rediscovery of Galen's anatomical treatise and a consequent rise of interest among physicians and scholars in Galen's work and increased availability of printed and illustrated works of anatomy which enthused among general people an interest in medicine and the secrets of the natural world [28]. Accordingly the increasing popularity of anatomy was not confined to physicians or medical students but also involved contemporary artists and even the general population. Italian renaissance artists started to perform their own dissections and the great Florentine painter Antonio Pollainolo (1431/1432-1498) dissected many human bodies in order to investigate the muscles and understand the human body in a modern way. Later on Leonardo da Vinci (1452-1519), Michelangelo Buanorotti (1475-1564), and Baccio Bandinelli (1493-1560) were known to have undertaken detailed anatomical dissections at various points in their career and set new standards in their portrayals of the human figure [29]. Some artists also produced 'écorchés,' studies of the peeled away or ripped apart forms of muscles, to explore their potential for purely artistic expression. The majority of the artists however limited their investigations to the surface of the body-the appearances of its musculature, tendons and bones as observed through the skin. Italian renaissance artists started practising human cadaveric dissection by necessity as they attempted to produce a refined, more lifelike, sculptural portrayal of the human figure in their works [30]. On the academic front the size of the audience increased dramatically in formal university dissections, which now began to assume a truly public character. Initially these larger audiences were accommodated in temporary structures of seats and risers set up in the interiors of churches and later on during the 16th century in anatomical theatres [17]. The first permanent anatomical theatre designed for public anatomical dissections was built by Fabricius ab Aquapendente (1533-1619) in 1594 in the University of Padua. This was followed by the anatomical theatre in the University of Bologna built in 1595 and reconstructed in 1636. The trend spread in other European countries also and anatomical theatres were built in the University of Leiden (the Netherlands) in 1596 and in University of Paris in 1604 (Fig. 2) [31]. Meanwhile the ever growing popularity of human cadaveric dissection which had its roots in the later part of 15th century, attained enormous proportion during the 16th century. Consequently the demand for dissectable bodies quickly escalated beyond the meagre but regular trickle supplied by the local gallows and families swayed by the prospect of a free funeral [32]. Initially the physicians arranged bodies by increasingly recommending post-mortems to the patient's family even when the family itself was satisfied as to the cause of death [17]. However this was not an option for the artists who relied on local hospitals (mostly charitable hospitals) for the corpses of poor foreigners and bodies of those persons who were without their families to worry about their funerary rites [33]. Gradually even these sources proved inadequate to the task and the anatomists began to rely heavily on unofficial or extralegal sources of supply. Consequently, malpractices such as grave-robbing which existed even in 14th century but were rare in those times became increasingly common during the 16th century. The extent of the problem can be gauged by the reports of students attempting to remove corpses awaiting burial or assaulting funeral processions [34]. Even the great anatomist Andreas Vesalius (1514-1564) in his anatomical treatise De humani corporis fabrica, candidly admitted to have resorted to such malpractice in order to ensure an adequate supply of cadavers for the purpose of dissection [35]. In one instance his Paduan students stole a female corpse from her tomb and flayed the whole skin from the cadaver lest it be recognised by her relatives during public dissection [36]. Such unethical anatomical practices led to unsavoury stories being gradually collected around the names of famous anatomists with regards to serious criminal offences like vivisection [27]. Vesalius was accused to have performed dissection on a Spanish aristocrat when the heart was still beating. Gabriele Falloppio (1523-1562) faced an allegation that he had vivisected Spanish twin brothers with syphilis [37]. Although there is no strong evidence to support these particular allegations, nonetheless these were not completely preposterous either and actually reflected the dangerous and unseemly haste with which 16th century anatomists approached fresh cadavers for dissection. Whether or not the hunger for cadavers among the 16th century anatomists actually put the living at risk, it certainly exposed the unprecedented links between anatomists and administrators of criminal justice as they began to influence the time and mode of execution of criminals to suite their requirement of dissection [17]. By the middle of the 16th century, there were clear signs of persistent public concern regarding the anatomical practices in Italy. Initially their reservations were based on traditional issues like funerary ritual and family honour but eventually emerged as a fear of being buried alive and coming under the anatomist's knife [34]. However, such concerns in the public domain co-existed with the well documented popular enthusiasm for the spectacle of human cadaveric dissection [32].
Human cadaveric dissection was practiced in Italy from 13th century (mostly autopsies though), however in France it was officially conducted from middle of 14th century [38]. The Papal Bull issued by Pope Boniface VIII in 1299 was possibly responsible for this delay [17]. Henri de Mondeville (1260-1320), the French anatomist executed the first unauthorized human dissection in the University of Montpellier in 1315. Prior to this event Mondeville had taught anatomy at Montpellier from a series of full length anatomical illustrations [39]. Guy de Chauliac (1300-1368), the French surgeon after receiving his Master's degree in Medicine and Surgery from the University of Paris in 1325, went to the University of Bologna to study anatomy. Here he attended dissection sessions of his teacher Nicolla Bertuccio (?-1347) and took the style of teaching from dissected cadavers prevalent in Bologna on his return to France. His knowledge regarding cadaveric dissection was critical to the advancement of anatomical practices in France [40]. In 1340, human cadaveric dissections were made official in the University of Montpellier and in 1407 the first sanctioned dissection took place in the University of Paris [41]. By the beginning of 15th century, cadaveric dissection became a regular event for teaching and learning anatomy in French universities [6]. In 14th century France, the study of anatomy was mostly limited to the use of criminal bodies [42], however due to increased demand for cadavers by the turn of 15th century, anatomical dissections on bodies meant for post-mortem autopsy became common in French universities [41]. It may be mentioned here that during the middle of 14th century, the Papacy had sanctioned post-mortem examinations of human bodies [43]. Although France in 16th century was open minded about the use of human cadavers for scientific inquiry, however during the early part of the 16th century, as human dissection was still not sanctioned by the church (Pope Clement VII accepted the teaching of anatomy by dissection in 1537) hence it was practised only in the universities and the number of cadavers available were very few [3843]. It was under these circumstances that Andreas Vesalius arrived at the University of Paris in 1533, after completing his studies in the University of Louvain [44]. He stayed in Paris till 1536 and studied anatomy under Jean Guiter d'Andernach (1487-1574) and Jacques Dubois (1478-1555) before moving to Padua [4546]. His assertion was that in order to learn anatomy, one has to dissect human cadavers by himself. His efforts exposed the errors of Galen's theories which were based on animal dissections and eventually led to the most significant change in anatomical studies in general: blind faith on ancient authoritative books were replaced by learning anatomy from dissected human cadavers [47]. In that way Vesalius pioneered a paradigm shift from the concept prevalent till then that dissection being used as an extension of illustrations in anatomy to the acceptance of cadaveric dissection as the most significant tool from which students would learn anatomy. In those days, French anatomists like Jacques Dubois were completely influenced by the Galenic thoughts and Vesalius was very much disappointed at the fact that there was lack of any effort to rectify the mistakes of predecessors. The influence of Galen could be gauged by the fact that human cadavers were never seen in Dubois's anatomical theatre and he taught anatomy from the carcases of dogs and other animals [45]. Vesalius was also not satisfied with the traditional manner in which human dissections were carried out in those days, when the actual dissection was performed by the barber surgeons and the lecturer/anatomist orated from a text as they thought it was below their dignity to perform dissections on human cadavers by themselves. Hence he endeavoured to dissect human bodies by himself however opportunities were few and far between as he was still a student [44]. Nevertheless, his desire to gain knowledge through dissection of cadavers was so strong that he would raid the gallows of Paris for half decomposed bodies and skeletons to dissect. Sometimes he even found the courage to venture outside the walls of Paris, braving wild dogs and the stench of decomposed bodies, in order to steal cadavers from the mound of Monfaucon, where the bodies of executed criminals were hung until they disintegrated [4849]. Vesalius continued with his unethical practice to procure cadavers later on in Padua which have been mentioned before in this review. However his hunger for dissection during his stay in Paris may have contributed to his exceptional dissection skills which he displayed to the audience during only his second anatomical lecture in Padua, when he took the knife away from the barber-surgeon and began to dissect the cadaver himself (Fig. 3) [50]. His emphasis on the need for direct experience of dissection was instrumental in human cadaveric dissection achieving the central role in medical training and research in those days. During this period (early Renaissance) human dissection emerged as a popular domain for scholarly pursuits as physicians considered it an effective medium to communicate their discoveries of the natural world in objective form [51]. Hence, human dissection proved to be critical in dissemination of scientific knowledge in the field of medicine during this period of scientific revolution. Cadaveric dissection though was a messy business, requiring great physical strength and ability to withstand the smell of corpses as they decomposed. Due to natural decomposition, a cadaver was suitable for dissection in the first 3-4 days following death as after this the stench became too much for the dissector to bear. In warm or moist weather, the cadaver decomposed even faster, this is the reason that many medical schools preferred to dissect in winter months [49]. From 1537, after Pope Clement VII accepted human dissection for anatomical studies, popularity of dissection started to spread beyond the boundaries of the universities among the general population leading to public dissection sessions being attended by huge crowds and subsequent establishment of anatomical theatres (Fig. 4) [1743].
Human cadaveric dissection was prohibited in England until 16th century which could be due to the overwhelming influence of the Catholic Church on the monarchs as well as the general population and until this period anatomical knowledge in England was largely based on manuscripts from classical Greece and medieval Italy and dissection of animals [5253]. However during the early part of the 16th century, the Protestant Reformation started in England due to a major disagreement between King Henry VIII and Pope Clement VII [54]. Under such circumstances, in 1565, a selected group of physicians and surgeons from the Royal college of Physicians and Company of Barber Surgeons (founded in 1540) were given permission to dissect a very limited number of human cadavers [55]. John Caius (1510-1573), an English physician who graduated from Cambridge and a student of Vesalius in Padua, was the President of the Royal College of Physicians from 1555-1560 and again between 1562-1571. It is generally acknowledged that he was the first to popularize the study of practical anatomy by human dissection in England [56]. During the 16th century human dissections in England were performed on the corpses of hanged criminals and hardly any of the bodies required for dissection were voluntarily donated for this purpose [57]. However by the onset of 17th century, demand of human cadavers for conducting dissections rose sharply as printed books in anatomy from Italy and France (where significant advancement of anatomical knowledge had been achieved by this time through human dissections) became widely available [52]. It was from this period that anatomical studies in England started to come up with original contributions as the great English Physician, William Harvey (1578-1657) who graduated from Padua under the guidance of Fabricius and did his masters from Cambridge published his anatomical treatise De moto cordis et sanguinis (on the motion of the heart and blood) in 1628 in which he documented his theory on circulation of blood which were based on observations made in during the course of dissecting several bodies including those of his own father and sister [58]. Meanwhile the eligible hangings performed at that time proved insufficient to meet the demand of human cadavers and this led to royal charters which enabled prominent universities to procure bodies of hanged criminals even from places far off from the actual boundaries of respective cities [52]. Till the middle of the 18th century, the Royal College of Physicians and the Company of Barber Surgeons were the only two groups permitted to carry out dissections and had an annual quota of ten cadavers between them [49]. Interestingly in 1745, rift appeared between the barber surgeons and the licensed surgeons, with the later breaking away and forming the Company of Surgeons (which was later granted a Royal Charter in 1800 to become the Royal College of Surgeons) which was empowered as the sole authority to receive cadavers of executed criminals [59]. On receiving a cadaver, the authorities performed a 'proper examination' consisting of little more than a cut over the sternum and then the bodies were donated to different medical schools for anatomical studies [49]. During this period, due to pressure from anatomists in the rapidly growing medical schools in England, the Murder Act was passed in 1752 which legalized the dissection of the bodies of executed murderers to be dissected in various medical schools for anatomical research and education [60]. The Murder Act served dual purpose; it was aimed at preventing the horrid crime of murder as it was associated with the apprehension of being dissected after hanging and it also ensured a legal supply of fresh human cadavers for anatomical studies [61]. Moreover, to ensure adequate supply of human bodies, the government significantly increased the number of crimes punishable by hanging [52]. However all these measures proved insufficient due to considerable expansion in anatomical and medical training activities in 18th century England and consequently a sizeable percentage of the required cadavers were procured illegally by exhuming them from graveyards during the night by men referred to as 'resurrectionists' and were sold to the medical schools [1].
During the 17th and 18th centuries, when academic anatomical dissections were open to public in most cases, legislators throughout Europe tried to capitalize on the general perception that undergoing dissection was a matter of great dishonour for an individual as the corpse was rendered unrecognizable and denied a conventional funeral [62]. Thus, more and more legislations were passed throughout the continent legalising the use of bodies of executed criminals for anatomical dissection, to the extent that anatomical dissection became synonymous with capital punishment [63]. Such legislations served the dual purpose of increasing the supply of human bodies for medical schools (thus reducing unethical/illegal means of cadaver procurement to an extent) and act as a deterrent for the criminals [64]. However, by the middle of the 18th century it became evident that the body supply solely from executions was not sufficient to meet the ever increasing needs of medical schools which were growing in numbers as anatomy flourished in Europe [65]. Accordingly many European countries passed legislations allowing the use of the unclaimed bodies of 'paupers,' inmates of prisons as well as psychiatric and charitable hospitals for dissection in addition to the corpses of executed criminals [63]. As a result, by the end of 18th century, the availability of unclaimed bodies reduced the deficiency of the human cadavers for anatomical dissection in Europe [65]. However, the scenario was different in England as the use of unclaimed bodies was not yet legalised by the beginning of the 19th century [6163]. By this time, anatomy as a discipline had become a lynchpin of surgical training and an intimate understanding of anatomy and skill in dissection were considered to be important components of medical education as such [66]. Doctors in England and surgeons in particular in their quest to enhance scientific expertise greatly emphasized on anatomy and human dissection during medical training, resulting in a sharp increase in demand for cadavers which was worsened by the fact that the methods of preservation of human bodies were inadequate until late in the 19th century [61]. Such circumstances encouraged unethical practices like grave robbing, body snatching and even murder for dissection which became alarmingly frequent in 19th century England [67]. With reference to grave robbing, particularly at risk were the corpses of the poor people due to their obvious inability to pay for secure coffins, superior burial sites and well rewarded watchmen [66]. The general public were well aware about these ongoing misdeeds and the perpetrators were disgracefully referred to as "body-snatchers"; however, anatomists called them by the more dignified term "resurrectionists" [68]. The growing unrest among the people against the illegal trade involving human cadavers could be assessed by the fact that often fights and at times even riots broke out when the family members of the dead tried to resist the delivery of corpses from funeral processions/graveyards to the anatomists [69]. Throughout the early part of 19th century, the acts of grave robbing and body snatching continued to persist as lucrative trade involving national transportation of cadavers and occasionally people were even murdered for the value of their corpse [67]. In 1828, two Irishmen living in Edinburgh, William Burke and William Hare murdered and sold the bodies of at least 16 men and women to Robert Knox as dissection material for his anatomy classes. Burke and Hare crafted a method of murder, which became infamous as 'Burking' (smothering a victim after intoxicating him/her with alcohol) and went completely undetected by the doctors to whom they sold their prey. Ironically Burke himself was awarded capital punishment and his corpse was dissected [70]. This was not an isolated event as further rings of murderers were later unearthed in London, each of whom sold the bodies of their victims to doctors for anatomical studies. John Bishop and Thomas Williams formed a notorious gang of grave robbers in London and supplied bodies in prominent medical schools in London. In 1831, both were convicted for a murder using the same method as Burke and Hare and came to be known as "London Burkers." They were hanged on 5 December 1831 and subsequently their bodies were handed over for anatomical dissection [71]. In the same year, Elizabeth Ross was also executed for murdering Catherine Walsh and selling her body to surgeons [72]. In order to put an end to the ongoing malpractice and acknowledging the evident panic among the general population, the British government passed the Warburton Anatomy Act in 1832, which allowed for the unclaimed bodies of the poor to be removed from workhouses and charitable hospitals and dissected at recognized medical schools by licensed anatomists. The term "unclaimed" referred to bodies that remained within the workhouse 48 hours after death [73]. The anatomy Act of 1832 marked the onset of a paradigm shift in procurement of human cadavers for anatomical dissection, as in accordance with the human rights and dignity, it excluded the use of corpses of executed criminals for cadaveric dissection and instead allowed for body donations [61]. Hence the Anatomy Act of 1832 essentially differed from legislations adopted by other European countries in the 18th century in terms of bringing curtains on the practice of using bodies of executed criminals which had been prevalent for centuries. Moreover, it opened a new avenue for procurement of dead bodies for anatomical studies in the form of voluntary body donation. The Anatomy Act was pivotal in involving unclaimed bodies for anatomical dissection and was embraced in many parts of the world as countries belonging to the British Commonwealth soon followed with similar legislations [6373]. The Act provided for cheap legal cadavers to medical schools, thus reducing the price of illegally obtained corpses, eventually making unethical practices such as grave robbing neither profitable nor practically viable [66]. The Anatomy Act of 1832 was effective in curtailing the practice of grave robbing; however, it led to considerable differences in the attitude to the practice of dissection between the rich and the poor in the society. The wealthy and elite were in favour of anatomical dissections as they felt it was necessary for progress in scientific research. Same was not the case with the economically deprived section of the society as it was their corpses which eventually got dissected either voluntarily when the body was sold by desperately poor and grieving family members [74] or even against their wishes when death occurred in the workhouse or charitable hospital with the body being unclaimed [61]. The Act effectively made poverty the sole criterion for dissection in England. The social divide with regards to perception towards anatomical dissection worsened further with the introduction of the Poor Law Amendment Act (PLAA) in 1834, which aimed to reform the poverty relief system and curbed the cost of poor relief [66]. The PLAA abolished the 'outdoor relief' (relief provided outside a workhouse) system for the poor and emphasized more on the 'indoor relief' to the poor through workhouses. Moreover poor funding led to worsening of the conditions within workhouses thus leading to increase in the number of unclaimed bodies available in workhouses and those running the workhouses would sell corpses of their unclaimed inmates after death to recur the expenses of poor relief in their premises [74]. The Anatomy Act and PLAA can be considered as an indicator of hardening attitudes of the society towards the poor as the much feared penalty of dissection for the worst of crimes such as murder which was the norm prior to the Anatomy Act had now become a penalty for poverty [61]. Overall majority of the population still viewed human dissection negatively and the social unrest was evident by the hostility of the general public towards medical profession as such as demonstrated during the Cholera outbreak in England in 1848-1849 [66]. Hence, it may be opined that the Anatomy Act solved the problem of grave robbing but could do little to change the societal attitude towards dissection.
Recent studies provide penetrating and discomforting insights into the practices of anatomists in England and associated Commonwealth countries post the introduction of Anatomy Act in 1832 [4961]. What emerges all too clearly from these studies is that although the Anatomy Act mandated that unclaimed bodies would play the central role in anatomical dissection, it was repeatedly manipulated or ignored after 1832 [75]. Although grave robbing was curtailed however body snatching continued as bodies of the poor were diverted from the grave to the dissection table involving a host of unfair/illegal means adopted by the funeral directors and the owners of institutions housing the poor [76]. Such unethical means of procuring bodies for dissection continued through the 19th century and early part of the 20th century. Widespread use of unclaimed bodies during this period were mostly driven by the belief that by undergoing dissection these subjects are giving back something to the society which looked after them during their lifetime [75]. In the early years of the 20th century, the poor houses/workhouses began to close down in a number of countries leading to decrease in the availability of unclaimed corpses [77]. Such a transition led to widespread use of the unclaimed bodies of the mentally incapacitated who died in psychiatric asylums [78]. Possibly this was more unethical than using the corpses of poor as authors have highlighted the fact that in being both poor and mentally ill, these subjects whose corpses were now being used by anatomists were doubly disadvantaged on account of circumstances over which they had no control [75]. This was followed by exploitation of the marginalised sections of the society including the coloured people and impoverished immigrants [6468]. During this time slave owners used to sell the bodies of deceased slaves to medical schools as these slaves were considered to be property of the owners and they considered it right to dispose of this property without the consent of the family [79]. A close look at these historical episodes clearly points to the central place occupied by the dependence of anatomy on unclaimed bodies during the 19th and first half of 20th century for dissection related activities. The use of unclaimed bodies reached its moral nadir in Germany and its occupied territories during the National Socialist regime between 1933-1945. The corpses of those executed, mostly political prisoners, were made available to Anatomical Institutes for scientific use [8081]. A legislation passed in 1942 denied relatives of executed Poles and Jews the right to claim the bodies [75]. Subsequently large number of dead bodies was supplied from concentrations camps, prisons and even psychiatric institutions for anatomical dissections [6382]. Recent literature does suggest that during this period, anatomists in Germany utilised the prolific supply of human bodies, mostly victims of atrocities performed by the National Socialist regime, for both research and teaching [81]. It may not be an overstatement that the imbalance between scientific aspirations of anatomists on one hand and ethical considerations on the other, which is clearly evident throughout the history of human cadaveric dissection, reached monstrous proportions during the National Socialist regime in Nazi Germany. Historical incidents like these should serve as a reminder for present day anatomists that disregard of moral values cannot be justified by the quest for scientific glory. Rather being members of the medical profession we should premiere the cause of ethical considerations in the scientific activities that we undertake.
The history of human cadaveric dissection in the United States followed an almost identical course as the one in Europe. Until the 18th century the bodies of executed criminals served the sole source of cadavers for anatomists in United States. In 1790, a federal law was passed which permitted federal judges to add dissection to a death sentence for murder. At times the threat of dissection was used to discourage crimes such as duelling which was disruptive to the society [83]. However the demand for human cadavers was on the rise which was triggered by the beginning of the first formal course in anatomy at University of Pennsylvania in 1745 [84]. Such conditions encouraged the practice of robbing the graves of freshly buried person, which attained enormous proportions during the 18th and 19th centuries [83]. The perpetrators ranged from professional thieves to tavern owners to employees at the medical schools themselves. At times, even medical students or doctors themselves indulged in grave robbing [68]. Societal injustice was clearly evident as the bodies dissected were mostly those of African-Americans, prisoners and poor [85]. In response to the public outcry, New York passed legislation in 1789 to prevent the odious practice of grave robbing [64]. However, the law did little to curtail the illegal practice as it offered no suggestion as to how medical schools might legally obtain the requisite corpses [86]. Ultimately, Massachusetts became the first state to enact laws in 1830 and 1833 that allowed unclaimed bodies of people who died in public institutions, hospitals, asylums and prisons to be used for anatomical dissection. The Massachusetts law stipulated that the unclaimed bodies of soldiers would not be dissected as they had already served the state during their lifetime [86]. Over the course of next few decades, many other states followed the example and introduced similar legislations, which successfully curtailed the practicality of grave robbing [83]. Nevertheless, these legislations reaffirmed the association between dissection and destitution as both before and after these acts were introduced it was the poor sections of the society who were exploited the most [87]. The anatomy laws that were enacted during the middle of the 19th century lasted till the middle of the 20th century [83]. During the early part of the 20th century, prejudice against dissection remained high, and although few people defied convention by bequeathing their bodies, body donation were as such few and far between. Moreover, legislations like the Maine's Anatomy Act of 1869, which rested the final decision about disposition of the body of an individual with the relatives acted as a bottleneck towards anatomical schools acquiring the bodies of those who had wilfully donated their bodies prior to death [87]. The supply of human cadavers to the medical schools was further worsened by United States Welfare Legislation and better health care for the poor leading to a sharp decline in the availability of unclaimed bodies between 1930 and 1960 [86]. During the early 1960s, a confusing conglomeration of anatomy acts, common laws and state statutes made body donation a legally complicated matter. Finally the development of transplant surgery and consequent rise in demand for anatomical material led to the National Conference of the Commissioners on Uniform State Laws approve the Uniform Anatomical Gift Act (UAGA) in 1968 [88]. UAGA was a turning point in terms of body donation as it established the human body as a property such that a donor's wish now superseded those of next of kin in court [83]. Within the next four years majority of the states followed suit and enacted laws that were similar to UAGA [75]. A second act was signed in 1987, which served to clarify the donation process further. Together these two acts, often together referred to as the UAGA were instrumental in standardizing and streamlining the process of body donation in the United States [86].
During the later part of the 20th century, initiatives were undertaken in different parts of the world to promote body donation for the purpose of anatomical studies. UAGA's successful promotion of body donation led to stabilization of willed-body programs towards the end of 20th century and eventually satisfied the demands of most of the medical schools across the United States [86]. The rise in body donation could be attributed to changes in social beliefs and practices as well as changing cultural landscapes in the United States [61]. Moreover social awareness also played a crucial role in enhancing body donation programs as medical professionals frequently donated their bodies because they had learnt firsthand the value of cadavers. Further doctors in US have been actively involved in discussing body bequest with their patients thereby encouraging them to donate their bodies [86]. The UK government passed the Anatomy Act in 1984, which aimed to simplify the process of body donation and accordingly the criterion for accepting a bequest of a body was that if a person either in writing or orally in the presence of two or more witnesses expressed a request that his/her body be used after death for anatomical studies. However there was a provision for the surviving spouse or any other surviving relative of the deceased to object to the body being used for anatomical dissection [89]. Subsequently the Human Tissue Act was introduced in 2004, which formulated a hierarchy of qualifying relationships ranked with regard to provision of consent, so that the primacy of wishes can be determined [90]. Since the introduction of the Anatomy Act in 1984, most of the medical schools in the UK rely heavily on donated human cadavers for anatomical activities [89]. Body donation constitutes the chief source of human cadavers in the medical schools of most of the European countries and the European Federation for Experimental Morphology (EFEM) has recommended certain measures in 2005, to ensure good practice in the domain of body donation. It stresses the need for informed consent, with donors being given clear information upon which to base their decision and emphasize on the openness with donors and their relatives at every stage from the receipt of an initial enquiry to the final disposal of the remains. Further, it encourages medical schools/anatomy departments to hold services of thanksgiving or commemoration for those who have donated their bodies. Finally, it suggests special lectures in ethics related to the bequest of human remains should be offered to all students studying anatomy to encourage development of appropriate sensitivities in relation to the conduct and respect that is expected while handling human remains for anatomical education and research [91]. Memorial services at the end of anatomy courses began in UK in 1965 and in the United Sates in the 1970s to sensitize students towards their cadavers [92]. In Nanjing, China, an annual public memorial ceremony for those who have donated their bodies to medical education and research is held since 2002 and is attended by volunteer donors, deceased donors' families, anatomy teaching faculty and medical students [93]. Towards the end of the 20th century, transition of religious and social ethics in the Korean Peninsula led to a significant rise in the number of people donating their bodies to medical schools in South Korea. In order to boost the body donation programs, Korean medical schools have begun to hold funeral ceremonies to honour body donors. These ceremonies are considered as a mark of respect for the dead and useful to promote awareness about body donation programs [94]. Medical schools in Australia and New Zealand solely depend on body donation for anatomical teaching and research [9596]. Similarly, donation is the only means of obtaining cadavers for use in medical schools in Thailand, however traditional beliefs result in an insufficient number of donated cadavers [97]. Human cadaveric dissection has a long history in Japan, and like their western counterparts, medical schools in Japan in the mid Edo era (late 17th to early 19th century) relied on bodies of executed criminals for anatomical studies followed by a shift towards unclaimed bodies after the Meiji Restoration in 1868 [98]. It was difficult to acquire bodies through donation programs due to unique social culture and understanding surrounding the family of the deceased. However from mid 1970s the scenario started to change and the enactment of the Body Donation Law in 1983 ensured sufficient number of donated bodies for anatomical studies at the medical schools throughout Japan. The law ensured the cultural acceptance of the concept of body donation as it was verified by the government, facilitated the true wishes of the deceased and not that of the family members and resolved possible disputes between family members [99]. In India, although there is an increasing demand of human cadavers used in medical education, however there is an insufficient supply of donated cadavers available for dissection. This could be attributed to lack of awareness along with firm religious beliefs and customs, apprehensions concerning handling of donated bodies and lack of mindset to accept dissection of one's own body [100]. The fact that there is no uniform national body donation law till date has not helped either. In most of the states in India, anatomical activities are still regulated by the Anatomy Act of 1949 and its subsequent amendments [101]. However the very recently introduced Odisha Anatomy (Amendment) Bill (2012), which has been adopted by many other states in the country, has made body donation hassle free [102]. Voluntary donors now have to sign simple forms to pledge their bodies for use in medical education. Further relatives of a dead person can also donate the body for anatomy teaching without any problem. Body bequest programs have been in slow in African countries like Nigeria and Republic of South Africa, resulting in limited number of cadavers available for anatomical dissection and this could be attributed to the political climate and ocioeconomic status of the population [103104]. Traditional spiritual beliefs, psychological factors and prevailing social norms adversely affect body donation programs even in some European countries like Turkey and Greece [105106]. The success of body donation programs has not been uniform across the world. This is an area where the society as such can collectively contribute towards advancement of medical education. Persistent efforts needs to be undertaken to sensitize the medical community as well as the general population to promote voluntary donation of dead bodies, which is critical to the human anatomy training for health professionals.
Human cadaveric dissection has been the primary medium of teaching gross anatomy to medical students for centuries [1]. However, in recent times, teaching anatomy by dissection no longer commands the same number of class hours as it once did as more and more educational material is being inducted into medical school curricula over the past few decades [107]. Moreover, medical programs in some countries have replaced cadaver dissection with virtual dissection in cyberspace and some others are seriously considering such measures, possibly due to economical factors as well as ethical concerns [108109]. Nevertheless, recent literature suggests that the dissected cadaver remains the most powerful means of delivering fundamental regional, relational and topographical anatomical knowledge to medical students, which is indispensable to ensure safe and efficient clinical practice [110111]. Researchers have documented that decreased use of dissection as teaching tool is one of the factors that can have a negative influence on the anatomical knowledge of medical students [112]. Evidence suggests that learning anatomy by active exploration through cadaveric dissection actually contributes to improvement of anatomic knowledge [3]. Medical students have opined that cadaveric dissection deepens their understanding of anatomical structures, provides them with a three dimensional perspective of structures and helps them to recall what they learnt. It is noteworthy that the innovative modes of learning anatomy such as the interactive multimedia resources have not replaced student's perception about the importance of cadaveric dissection [113]. In some medical schools, newer radiological imaging techniques which permit in vivo visualization of anatomy structures have supplanted traditional cadaver dissection in teaching human anatomy. However, it has been observed that despite its important strengths, radiology cannot simply substitute cadaveric dissection, which provides students with deep insights into meaning of human embodiment and mortality and represents a profound rite of passage into the medical profession [114]. The current trend of a steady decline in the number of contact hours in relation to human dissection and consequent suboptimal anatomy knowledge is an area of concern not only for undergraduates but also at the post graduate level for specialities where surgical anatomy is essential [115]. In present times, when medicine is becoming more practical, technical, and specialized, physicians should be aware of the details related to the anatomy of the region they deal with as this will provide them with an intimate knowledge of their science [116]. Reports of patient misadventure due to inadequate anatomical knowledge have prompted researchers to come up with the idea of barrier assessment (halts further progress until satisfactorily completed) while teaching dissection based anatomy [107]. Authors have opined that long term consequence of this shortage of anatomical knowledge could have serious implications on patient safety and have suggested that medical schools should shift to dissection as the core method for teaching gross anatomy [2]. Apart from imparting essential anatomical knowledge, the human dissection room can serve as an ideal ground for cultivating humanistic values among medical students. Medical training essentially begins with the cadaveric dissection and nearly all clinicians remember the details of their first interaction with the human cadaver [110]. Hence, the dissection lab premises provide the educator with an immediate opportunity to teach and encourage humanistic qualities of respect, empathy and compassion among first semester medical students [117]. Moreover the students can be guided to use the experience of handling a human cadaver as a potential launching pad for them to mature into effective as well as empathetic clinicians [118]. Further, sensitizing the students to develop an emotional attachment with the cadaver can help him/her to understand the psychosocial factors contributing to a patient's illness [119]. Attention to concepts of humanistic care is a challenge in present day medical education curriculum when physicians and medical care as such are becoming mechanized by the day with increasing focus on procedures and technical aspects. The rise of the body donation programs has been instrumental in fostering social responsibilities among medical students. In some parts of the world, students get the opportunity to interact with the families of the deceased persons whom they are dissecting [118]. The University of Oklahoma College of Medicine have introduced the unique concept of "Donor Luncheon," whereby medical students meet the families of the donor prior to dissection in the anatomy course and findings suggest that such an opportunity enables the students to maintain humanistic attitudes at the beginning of their medical career [117]. Interaction with the donor family/possible donor and subsequent identification of the donor in the dissection room allows the student to gain perspective and reflect upon their emotions [110]. Also the students can possibly use the dissection lab experience pedagogically to better prepare themselves for the stress of the medical world, especially issues surrounding death and dying [109]. Human cadaveric dissection has survived the test of time and till date the importance of student-cadaver encounter remains paramount in medical education. The dissection room provides multifaceted education experiences while accomplishing the traditional objectives within the allotted time. In other words, in the dissection lab, medical students can learn to do their scheduled work without neglecting their emotions or developing an attitude of detached concern. Accordingly anatomists have presented arguments in favour of continuation of the use of cadaver material in anatomical sciences education which would be beneficial to future physicians and pivotal in strengthening a close and symbiotic association between anatomists and surgeons [107120].
The rise of ancient Greek medicine paved the way for the inception of human cadaveric dissection as a tool for teaching anatomy in 3rd century BC. Unfortunately the practice of human dissection was prohibited in Europe during the Middle Ages due to religious and popular beliefs. However from its revival at the beginning of 14th century, human dissection has been an integral part of anatomy teaching in medical schools. During the 14th century, religious authorities gave permission for human dissection only within the university premises and these were conducted once/twice annually on corpses of executed criminals. However by the beginning of 15th century, cadaveric dissection became a regular event in European universities and the supply of criminal bodies proved insufficient. Taking advantage of the Papal sanction of post-mortem examination to investigate the cause of death, anatomists started performing dissection on bodies meant for post-mortem autopsy. From the later part of the 15th century, human dissection became extremely popular as the wave of European Renaissance started to influence the domain of anatomical sciences and from the middle of 16th century, after Papal approval of human dissection for anatomical studies, formal university dissection sessions assumed a full blown public character being attended by large audiences, eventually leading to establishment of permanent anatomical theatres across Europe. Conventional sources of human cadavers proved inadequate to the task in the face of such unprecedented demand and consequently anatomists began to rely on extralegal sources which involved grave-robbing, body snatching and even murder for anatomical dissection. In response to the strong public outcry against these ongoing malpractices, many European countries passed legislations during the 18th and 19th centuries, legalising the procurement of unclaimed bodies of poor from workhouses and charitable hospitals for dissection in medical schools. The most prominent among these legislations was the Anatomy Act (1832) passed by the British government which not only allowed the use of unclaimed bodies but also prohibited the tradition of using corpses of executed criminals for anatomical dissection. Although the Anatomy Act (1832) was successful in curtailing the illegal practice of grave-robbing, it led to deep societal divide between the rich and poor with regards to the attitude towards practice of human dissection as in most cases it was the bodies of individuals from the economically backward sections of the society that underwent dissection. Moreover, even after the introduction of the Anatomy Act, unethical practices continued to plague the domain of human dissection involving bodies of poor/mentally ill/coloured people/impoverished immigrants. Incidentally, the National Socialist regime (1933-1945) in Germany set a disgraceful example of neglecting human rights and dignity by providing the bodies of victims of their atrocities to anatomists for research and education. Till the first part of the 20th century, instances of voluntary body donation was very low as socio-cultural prejudice against human dissection remained high. However, in the second half of 20th century, the approval of the UAGA in the United States of America in 1968 ensured a steady supply of human bodies to the medical schools through body bequest. Presently, body donation constitutes the sole source of human bodies for dissection in medical schools in most parts of the world. Even in those countries, where body donation programs have had limited success, measures are being undertaken to promote voluntary donation of dead bodies. Although the number of hours devoted to human dissection have been reduced in most of the medical schools over the past few decades, however research findings clearly emphasizes on the indispensability of dissection in anatomical sciences. Moreover the anatomy dissection lab in coherence with the body donation programs has the potential to cultivate humanistic values among medical students which could possibly contribute invaluably towards the making of empathetic physicians of tomorrow.
Figures and Tables
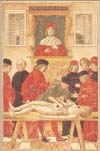 | Fig. 1A woodcut illustration from Fasciculus medicinae (1491) depicting human dissection in medieval Italy. The anatomist (Lector) over viewing the dissection, which is being performed by a barber surgeon (Sector) under directions from the Ostensor, who is pointing to the part of the body to be dissected. Fasciculus medicinae was edited by Johannes de Ketham, a German physician who practiced in medieval Italy. Image in public domain. |
 | Fig. 2An anonymous engraving of an anatomical dissection session being conducted in full public view in the anatomical theatre in University of Leiden (the Netherlands) which was built in 1596. The illustration is based on a drawing by J.C. vant Woudt in 1609. Image in public domain. |
 | Fig. 3Andreas Vesalius undertaking an anatomical lecture in Padua. A notable shift from the prevalent trend in medieval Italy as he is dissecting the human body himself. He is referring to Galen's text (prevalent textbook in anatomy in those days) which is open by the side of the cadaver. Vesalius is surrounded by his students in Padua and the general public viewing the dissection from the gallery. Image in public domain. |
 | Fig. 4The anatomy lesson of Dr. Nicolaes Tulp, official city anatomist of the Amsterdam Guild of Surgeons, drawn by Rembrandt in 1632. Anatomical dissection sessions were social events in those days being attended by students as well as the general public on payment of an entrance fee. All the spectators were properly dressed for a solemn social occasion. Image in public domain. |
References
1. Magee R. Art macabre: resurrectionists and anatomists. ANZ J Surg. 2001; 71:377–380.
2. Yammine K. The current status of anatomy knowledge: where are we now? Where do we need to go and how do we get there? Teach Learn Med. 2014; 26:184–188.
3. Nwachukwu C, Lachman N, Pawlina W. Evaluating dissection in the gross anatomy course: correlation between quality of laboratory dissection and students outcomes. Anat Sci Educ. 2015; 8:45–52.
4. Sallam HN. The ancient Alexandria school of medicine. Gynecol Obstet Fertil. 2002; 30:3–10.
5. Serageldin I. Ancient Alexandria and the dawn of medical science. Glob Cardiol Sci Pract. 2013; 2013:395–404.
6. Elizondo-Omaña RE, Guzmán-López S, García-Rodríguez Mde L. Dissection as a teaching tool: past, present, and future. Anat Rec B New Anat. 2005; 285:11–15.
7. von Staden H. The discovery of the body: human dissection and its cultural contexts in ancient Greece. Yale J Biol Med. 1992; 65:223–241.
8. Fraser PM. Ptolemaic Alexandria. Oxford: Clarendon Press;1972.
9. Mavrodi A, Paraskevas G. Mondino de Luzzi: a luminous figure in the darkness of the Middle Ages. Croat Med J. 2014; 55:50–53.
10. Gregory SR, Cole TR. MSJAMA. The changing role of dissection in medical education. JAMA. 2002; 287:1180–1181.
11. Rengachary SS, Colen C, Dass K, Guthikonda M. Development of anatomic science in the late middle ages: the roles played by Mondino de Liuzzi and Guido da Vigevano. Neurosurgery. 2009; 65:787–793.
12. Siraisi NG. Medieval and early Renaissance medicine: an introduction to knowledge and practice. Chicago, IL: The University of Chicago Press;1990.
13. Aufderheide AC. The scientific study of mummies. Cambridge: Cambridge University Press;2003.
14. Somerville R. Pope Alexander III and the Council of Tours (1163): a study of ecclesiastical politics and institutions in the twelfth century. Berkeley, CA: The University of California Press;1977.
15. Persaud TV. Early history of human anatomy: from antiquity to the beginning of the modern era. Springfield, IL: Charles C. Thomas;1984.
16. Prioreschi P. Determinants of the revival of dissection of the human body in the Middle Ages. Med Hypotheses. 2001; 56:229–234.
17. Park K. The criminal and the saintly body: autopsy and dissection in Renaissance Italy. Renaiss Q. 1994; 47:1–33.
18. Pilcher LS. The Mondino myth. Med Library Hist J. 1906; 4:311–331.
19. Walsh JJ. The popes and the history of anatomy. Med Library Hist J. 1904; 2:10–28.
20. Infusino MH, Win D, O'Neill YV. Mondino's book and the human body. Vesalius. 1995; 1:71–76.
21. Ferrari G. Public anatomy lessons and the carnival: the anatomy theatre of Bologna. Past Present. 1987; (117):50–106.
22. Joffe SN. Andreas Vesalius: the making, the madman, and the myth. Osborne Park: Persona Publishing;2009.
23. Park K. That the medieval church prohibited human dissection. In : Numbers RL, editor. Galileo Goes to Jail: And Other Myths about Science and Religion. Cambridge, MA: Harvard University Press;2009. p. 43–49.
24. Joutsivuo T. Vesalius and De humani corporis fabrica: Galen's errors and the change of anatomy in the sixteenth century. Hippokrates (Helsinki). 1997; 98–112.
25. Premuda L. Storia dell'iconografia anatomica: con un'appendice di Gaetano Ottaviani. Milano: Aldo Martello Editore;1957.
26. Park K. The life of the corpse: division and dissection in late medieval Europe. J Hist Med Allied Sci. 1995; 50:111–132.
27. French R. Dissection and vivisection in the European Renaissance. Aldershot: Ashgate;1999.
28. Huff TE. The rise of early modern science: Islam, China and the West. Cambridge: Cambridge University Press;2003.
29. Sellmer R. Anatomy during the Italian Renaissance: a brief history of how artists influenced its development. In : Whitelaw WA, editor. The Proceedings of the 10th Annual History of Medicine Days. Calgary: Alberta Faculty of Medicine, The University of Calgary;2001. p. 341.
30. Cazort M, Kornell M, Roberts KB. The ingenious machine of nature: four centuries of art and anatomy. Ottawa: National Gallery of Canada;1996.
31. O'Malley CD. History of medical education: an international symposium held February 5-9, 1968. 673. Berkeley, CA: The University of California Press;1996.
32. Frati P, Frati A, Salvati M, Marinozzi S, Frati R, Angeletti LR, Piccirilli M, Gaudio E, Delfini R. Neuroanatomy and cadaver dissection in Italy: History, medicolegal issues, and neurosurgical perspectives. J Neurosurg. 2006; 105:789–796.
33. Mavrodi A, Paraskevas G, Kitsoulis P. The history and the art of anatomy: a source of inspiration even nowadays. Ital J Anat Embryol. 2013; 118:267–276.
34. Grendler PF. The universities of the Italian Renaissance. Baltimore, MD: Johns Hopkins University Press;2002. p. 616.
35. Vesalius A. De Humani Corporis Fabrica Libri Septem. Basilea: Officina Ioannis Oporini;1543.
36. Ball P. The devil's doctor: Paracelsus and the world of Renaissance magic and science. New York: Random House Publishing;2014. p. 67.
37. Shotwell RA. The revival of vivisection in the sixteenth century. J Hist Biol. 2012; 46:171–197.
38. Daynes-Diallo S. A touch of France: theory and practice: European Renaissance medicine. Medicographia. 2011; 33:334–343.
39. Pilcher JE. Guy de Chauliac and Henri de Mondeville,-A Surgical Retrospect. Ann Surg. 1895; 21:84–102.
40. Thevenet A. Guy de Chauliac (1300-1370): the "father of surgery". Ann Vasc Surg. 1993; 7:208–212.
41. McArdle WD, Katch FI, Katch VL. Exercise physiology: nutrition, energy, and human performance. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins;2010.
42. Brim OG Jr, Freeman HE, Levine S, Scotch NA. The dying patient. Piscataway, NJ: Transaction Publishers;1980.
43. Singh AK. Modern world system and Indian proto-industrialization: Bengal 1650-1800. Vol. 1. New Delhi: Northern Book Centre;2006. p. 296.
44. Holomanova A, Ivanova A, Brucknerova I, Benuska J. Andreas Vesalius: the reformer of anatomy. Bratisl Lek Listy. 2001; 102:48–54.
45. Tubbs RS, Linganna S, Loukas M. Jacobus Sylvius (1478-1555): physician, teacher, and anatomist. Clin Anat. 2007; 20:868–870.
46. Drizenko A. The Anatomy Institutions of Jean Guinter d'Andernach (1487-1574), and Andre Vesale (1514-1564). Hist Sci Med. 2011; 45:321–328.
47. Aziz MA, McKenzie JC, Wilson JS, Cowie RJ, Ayeni SA, Dunn BK. The human cadaver in the age of biomedical informatics. Anat Rec. 2002; 269:20–32.
48. Adler RE. Medical firsts: from Hippocrates to the human genome. Hoboken, NJ: John Wiley & Sons;2004.
49. MacDonald H. Human remains: dissection and its histories. London: Yale University;2005.
50. Goodrich JT. Andreas Vesalius and anatomy: a re-evaluation of his efforts. Hist Sci Med. 1982; 17:13–16.
51. Ghosh SK. Evolution of illustrations in anatomy: a study from the classical period in Europe to modern times. Anat Sci Educ. 2015; 8:175–188.
52. Mitchell PD, Boston C, Chamberlain AT, Chaplin S, Chauhan V, Evans J, Fowler L, Powers N, Walker D, Webb H, Witkin A. The study of anatomy in England from 1700 to the early 20th century. J Anat. 2011; 219:91–99.
53. Mitchell PD. Anatomical dissection in Enlightenment Britain and beyond: autopsy, pathology and display. Surrey: Ashgate Publishing Ltd.;2012.
54. Ferm V. Pictorial History of Protestantism. New York: Philosophical Library;1957.
55. Robinson JO. The barber-surgeons of London. Arch Surg. 1984; 119:1171–1175.
56. Alberti F. Anatomy in London. Anatomic teaching in London and John CAIUS, student of the Padua School before Harvey. Minerva Med. 1961; 52:Varia 1893–1896.
57. Payne L. "With much nausea, loathing, and foetor": William Harvey, dissection, and dispassion in early modern medicine. Vesalius. 2002; 8:45–52.
58. Gregory A. Harvey's hear: the discovery of blood circulation. Cambridge: Icon Books;2001.
59. Sanders MA. William Cheselden: anatomist, surgeon, and medical illustrator. Spine (Phila Pa 1976). 1999; 24:2282–2289.
60. Fielding S. The executioner's bible: the story of every British hangman of the twentieth century. London: John Blake Publishing;2008.
61. Richardson R. Death, dissection and the destitute. London and New York: Routledge and Kegan Paul;1987.
62. Park K. Secrets of women: gender, generation, and the origins of human dissection. New York: Zone Books;2006. p. 15.
63. Hildebrandt S. Capital punishment and anatomy: history and ethics of an ongoing association. Clin Anat. 2008; 21:5–14.
64. Sappol M. A traffic of dead bodies: anatomy and embodied social identity in nineteenth-century America. Princeton, NJ: Princeton University Press;2002. p. 102.
65. Stukenbrock K. Unter dem Primat der Okonomie? Soziale und wirtschaftliche Randbedingungen der Leichenbeschaffung fuer die Anatomie. In : Helm J, Stukenbrock K, editors. Anatomie: Sektionen einer Medizinischen Wissenschaft im 18. Jahrhundert. Stuttgart: Franz Steiner Verlag;2003. p. 227–239.
66. Hutton F. The study of anatomy in Britain, 1700-1900: the body, gender and culture. London: Pickering & Chatto Ltd.;2013.
67. Humphries E. Murder, mortsafes and Moir: a medical student looks at anatomy teaching in Aberdeen. J R Coll Physicians Edinb. 2014; 44:67–71.
68. Halperin EC. The poor, the Black, and the marginalized as the source of cadavers in United States anatomical education. Clin Anat. 2007; 20:489–495.
69. Linebaugh P. The Tyburn riot against the surgeons. In : Hay D, Linebaugh P, Rule JG, Thompson EP, Winstow C, editors. Albion's Fatal Tree: Crime and Society in Eighteenth Century England. London: Penguin;1975. p. 65–117.
70. Rosner L. The anatomy murders: being the true and spectacular history of Edinburgh's notorious Burke and Hare and of the man of science who abetted them in the commission of their most heinous crimes. Philadelphia, PA: University of Pennsylvania Press;2011.
71. Wise S. The Italian boy: a tale of murder and body snatching in 1830s London. New York: Metropolitan Books;2004.
72. Moore W. The knife man: blood, body snatching, and the birth of modern surgery. Portland, OR: Broadway Books;2006. p. 354.
73. Persaud TV. A history of anatomy: The Post-Vesalian Era. Springfield, IL: Charles C. Thomas;1997.
74. Hurren ET. Protesting about Pauperism: poverty, politics and poor relief in Late Victorian England 1870-1900. Woodbridge: Boydell Press;2007.
75. Jones DG, Whitaker MI. Speaking for the dead: the human body in biology and medicine. 2nd ed. Farnham: Ashgate;2009.
76. MacDonald HP. Possessing the dead: the artful science of anatomy. Carlton: Melbourne University Press;2010.
77. Jones DG, Fennell S. Bequests, cadavers and dissections: sketches from New Zealand history. N Z Med J. 1991; 104:210–212.
78. Jones DG. The anatomy museum and mental illness: the centrality of informed consent. In : Coleborne C, MacKinnon D, editors. Exhibiting Madness in Museums: Remembering Psychiatry through Collection and Display. New York: Routledge;2011. p. 161–177.
79. Savitt TL. Medicine and slavery: the diseases and health care of blacks in Antebellum Virginia. Champaign, IL: University of Illinois Press;1978.
80. Hildebrandt S. First symposium on "Anatomie im National-sozialismus" ("Anatomy in National Socialism"), Wurzburg, Germany, September 29, 2010. Clin Anat. 2011; 24:97–100.
81. Kaiser S. Tradition or change? Sources of body procurement for the Anatomical Institute of the University of Cologne in the Third Reich. J Anat. 2013; 223:410–418.
82. Redies C, Viebig M, Zimmermann S, Fröber R. Origin of corpses received by the anatomical institute at the University of Jena during the Nazi regime. Anat Rec B New Anat. 2005; 285:6–10.
83. Hulkower R. From sacrilege to privilege: the tale of body procurement for anatomical dissection in the United States. Einstein J Biol Med. 2011; 27:23–26.
84. Tward AD, Patterson HA. MSJAMA. From grave robbing to gifting: cadaver supply in the United States. JAMA. 2002; 287:1183.
85. Humphrey DC. Dissection and discrimination: the social origins of cadavers in America, 1760-1915. Bull N Y Acad Med. 1973; 49:819–827.
86. Garment A, Lederer S, Rogers N, Boult L. Let the dead teach the living: the rise of body bequeathal in 20th-century America. Acad Med. 2007; 82:1000–1005.
87. Weinmann GH. A survey of the law concerning dead human bodies. Bulletin No. 73. Washington, DC: National Research Council of the National Academy of Sciences;1929. p. 68–72.
88. Dalley AF, Driscoll RE, Settles HE. The Uniform Anatomical Gift Act: what every clinical anatomist should know. Clin Anat. 1993; 6:247–254.
89. Greene JR. Effects of detailed information about dissection on intentions to bequeath bodies for use in teaching and research. J Anat. 2003; 202:475–477.
90. Taylor SJ, Wilson DJ. The Human Tissue Act (2004), anatomical examination and the importance of body donation in Northern Ireland. Ulster Med J. 2007; 76:124–126.
91. McHanwell S, Brenner E, Chirculescu AR, Drukker J, van Mameren H, Mazzotti G, Pais D, Paulsen F, Plaisant O, Caillaud MM, Laforet E, Riedere BM, Sanudo JR, Bueno-Lopez JL, Donate-Oliver F, Sprumont P, Teofilovski-Parapid G, Moxham BJ. The legal and ethical framework governing body donation in Europe: a review of current practice and recommendations for good practice. Eur J Anat. 2008; 12:1–24.
92. Warner JH, Rizzolo LJ. Anatomical instruction and training for professionalism from the 19th to the 21st centuries. Clin Anat. 2006; 19:403–414.
93. Zhang L, Xiao M, Gu M, Zhang Y, Jin J, Ding J. An overview of the roles and responsibilities of Chinese medical colleges in body donation programs. Anat Sci Educ. 2014; 7:312–320.
94. Park JT, Jang Y, Park MS, Pae C, Park J, Hu KS, Park JS, Han SH, Koh KS, Kim HJ. The trend of body donation for education based on Korean social and religious culture. Anat Sci Educ. 2011; 4:33–38.
95. McClea K, Stringer MD. The profile of body donors at the Otago School of Medical Sciences: has it changed? N Z Med J. 2010; 123:9–17.
96. Alexander M, Marten M, Stewart E, Serafin S, Štrkalj G. Attitudes of Australian chiropractic students toward whole body donation: a cross-sectional study. Anat Sci Educ. 2014; 7:117–123.
97. Agthong S, Wiwanitkit V. Cadaver donation: a retrospective review at the King Chulalongkorn Memorial Hospital, Bangkok. Southeast Asian J Trop Med Public Health. 2002; 33:Suppl 3. 166–167.
98. Kozai T. History of collecting cadavers in Japan. Kaibogaku Zasshi. 2007; 82:33–36.
99. Sato T. Process of development of body donation law in Japan. Kaibogaku Zasshi. 2007; 82:63–71.
100. Rokade SA, Gaikawad AP. Body donation in India: social awareness, willingness, and associated factors. Anat Sci Educ. 2012; 5:83–89.
101. Ajita R, Singh I. Body donation and its relevance in anatomy learning: a review. J Anat Soc India. 2007; 56:44–47.
102. Appaji AC, Kulkarni R. A survey on the role and the status of cadavers in medical education: an Indian scenario. J Clin Diagn Res. 2012; 6:1132–1136.
103. Anyanwu EG, Obikili EN. Dissecting the dissectors: knowledge, attitude, and practice of body bequests by Nigerian anatomists. Anat Sci Educ. 2012; 5:347–353.
104. Kramer B, Hutchinson EF. Transformation of a cadaver population: Analysis of a South African cadaver program, 1921-2013. Anat Sci Educ. 2015; 8:445–451.
105. Sehirli US, Saka E, Sarikaya O. Attitudes of Turkish anatomists toward cadaver donation. Clin Anat. 2004; 17:677–681.
106. Halou H, Chalkias A, Mystrioti D, Iacovidou N, Vasileiou PV, Xanthos T. Evaluation of the willingness for cadaveric donation in Greece: a population-based study. Anat Sci Educ. 2013; 6:48–55.
107. Ramsey-Stewart G, Burgess AW, Hill DA. Back to the future: teaching anatomy by whole-body dissection. Med J Aust. 2010; 193:668–671.
108. Lempp HK. Perceptions of dissection by students in one medical school: beyond learning about anatomy. A qualitative study. Med Educ. 2005; 39:318–325.
109. Robbins BD, Tomaka A, Innus C, Patterson J, Styn G. Lessons from the dead: the experiences of undergraduates working with cadavers. Omega (Westport). 2008; 58:177–192.
110. Rizzolo LJ. Human dissection: an approach to interweaving the traditional and humanistic goals of medical education. Anat Rec. 2002; 269:242–248.
111. Bergman EM, de Bruin AB, Herrler A, Verheijen IW, Scherpbier AJ, van der Vleuten CP. Students' perceptions of anatomy across the undergraduate problem-based learning medical curriculum: a phenomenographical study. BMC Med Educ. 2013; 13:152.
112. Bergman EM, Verheijen IW, Scherpbier AJ, Van der Vleuten CP, De Bruin AB. Influences on anatomical knowledge: The complete arguments. Clin Anat. 2014; 27:296–303.
113. Azer SA, Eizenberg N. Do we need dissection in an integrated problem-based learning medical course? Perceptions of first- and second-year students. Surg Radiol Anat. 2007; 29:173–180.
114. Gunderman RB, Wilson PK. Viewpoint: exploring the human interior: the roles of cadaver dissection and radiologic imaging in teaching anatomy. Acad Med. 2005; 80:745–749.
115. Older J. Anatomy: a must for teaching the next generation. Surgeon. 2004; 2:79–90.
116. Mavrodi A, Paraskevas G. Evolution of the paranasal sinuses' anatomy through the ages. Anat Cell Biol. 2013; 46:235–238.
117. Crow SM, O'Donoghue D, Vannatta JB, Thompson BM. Meeting the family: promoting humanism in gross anatomy. Teach Learn Med. 2012; 24:49–54.
118. Talarico EF Jr. A change in paradigm: giving back identity to donors in the anatomy laboratory. Clin Anat. 2013; 26:161–172.
119. Halpern J. From detached concern to empathy: humanizing medical practice. New York: Oxford University Press;2001.
120. Korf HW, Wicht H, Snipes RL, Timmermans JP, Paulsen F, Rune G, Baumgart-Vogt E. The dissection course: necessary and indispensable for teaching anatomy to medical students. Ann Anat. 2008; 190:16–22.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download