Introduction
Total or partial agenesis of the portal vein, abnormal branching pattern of the portal vein, arteriovenous malformations, and venous malposition are congenital variants of the portal vein. Anomalous branching pattern of the main portal vein (MPV) at the hepatic hilum are less frequent than those of the hepatic arteries, hepatic veins, and biliary ducts [1, 2]. Absence of portal vein bifurcation is an extremely rare anomaly and represents 0.03-2% of all the cases [3]. Presurgical awareness of portal vein anatomy is utmost important in liver transplantation, partial hepatectomy and portal vein embolization [4]. We are reporting a case of absence of portal vein bifurcation showing single intrahepatic portal vein (IHPV) with gradual decreasing caliber, coursing from right lobe to left lobe of liver and giving rise to segmental branches, in a young female patient on contrast-enhanced computed tomography (CT) study of abdomen.
Case Report
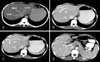
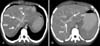
A 24-year-old-female patient reported to surgical outdoor with history of constipation, mild vague abdominal pain for 1 week. Menstrual cycle was regular. On examination, the vitals were stable. Central nervous system and cardiorespiratory system examination was normal. Abdomen was soft and non tender on palpation and revealed normal bowel sound on auscultation. Complete blood count and urine examination was normal. The patient had normal report of abdominal ultrasound study which was carried out two days back in private diagnostic center. Contrast-enhanced CT scan of abdomen was performed in our hospital after oral and intravenous contrast administration to the patient for further evaluation. Liver showed three hepatic veins such as right hepatic vein, middle hepatic vein and left hepatic vein draining to inferior venacava (Fig. 1A). The hepatic veins are of normal caliber. MPV revealed single IHPV without bifurcation (Fig. 1B-D) entering the right lobe of liver, coursing anteriorly in an arch like pattern with decreasing caliber to reach the left lobe of liver and giving rise to segmental branches to both lobes of liver. The MPV caliber was normal and measures about 9 mm in diameter. Thick maximum intensity projection axial and oblique images showed MPV behind pancreatic neck, absence of MPV bifurcation at porta hepatis, single IHPV entering right lobe of liver, giving rise to segmental braches to both lobes of liver (Fig. 2A, B). Both lobes of liver were of normal size. No intrahepatic biliary channel dilation was seen. Abdominal organs, bowel loops, and retroperitoneum were unremarkable in the abdominal CT study. The normal anatomical pattern of portal vein and hepatic veins in CT study of abdomen in another patient was shown in Fig. 3A and B for comparison.
Discussion
The MPV is formed by the union of splenic vein with superior mesenteric vein. It carries blood from digestive organs, spleen, pancreas and gall bladder to liver [3]. The MPV commonly enters the porta hepatis and divides into the right portal vein (RPV) and left portal vein (LPV). The RPV enters the right hepatic lobe and divides into two branches, supplying the anterior and posterior segments of the right lobe. The LPV gives off an initial horizontal segment in left hepatic lobe, turns anteriorly in a parasagittal plane at the level of the ligamentum teres to form its vertical segment. The medial and lateral segments of the left lobe are supplied by the vertical segment of LPV [4].
The adult portal vein is developed from vitelline and umbilical veins during 4th to 10th week of gestation. The proximal part right and left vitelline veins lie on both side of the developing duodenum and are interconnected by three anastomotic channels. The cranial and caudal anastomotic channels are located ventral to developing duodenum while the mid anastomotic channel runs dorsal to the duodenum. The superior mesenteric and splenic vein join to left vitelline vein a short distance caudal to dorsal anastomosis. Both umbilical veins initially lie on both side of developing liver bud. Distal portion of both umbilical veins and proximal portion of right umbilical vein gradually involute, leaving the left umbilical vein as the main channel between placenta and liver. The MPV is formed by the dorsal anastomotic channel, left vitelline vein between the entry of superior mesenteric and splenic vein and the dorsal anastomosis, part of right vitelline vein between dorsal and cranial ventral anastomosis. The right branch of portal vein develops from the part of right vitelline vein distal to cranial ventral anastomosis. The left branch of portal vein develops from the cranial ventral anastomosis and the part of left vitelline vein distal to cranial anastomosis. The remaining part of vitelline vein and caudal ventral anastomotic channel disappear. The ductus venosus is derived from the venous channel connecting the cranial portion of the right vitelline vein to the left umbilical vein (the future vertical segment of the LPV) and regressed to ligamentum venosum after birth. The horizontal part of LPV is derived from anastomotic venous channel between the caudal portion of the right vitelline vein with the left umbilical vein [4].
Absence of horizontal part of LPV or absence of portal bifurcation can be due to failure of the anastomosis between the caudal portion of the right vitelline vein and the left umbilical vein and appearance of new communicating venous channel between these two venous segments. [4, 5].
Some author opines that absence of portal bifurcation is due to failure of right branch of portal vein irrespective of its intrahepatic course from left to right or right to left due to the fact that the embryologic origin of the left branch of the portal vein is from multiple venous segments and the agenesis of the LPV is very unlikely to happen [6].
Major anatomic variants such as portal vein duplication, congenital absence of the portal vein, absence of branching of the portal vein, and preduodenal portal vein are rare [7]. The portal vein commonly divides at the porta hepatis into the RPV and the LPV. The RPV first gives off branches to the caudate lobe and then it divides into the anterior and posterior branches, which further subdivide into the superior and inferior segmental branches to supply the right lobe of the liver. The LPV first has a horizontal course to the left and then it turns medially towards the ligamentum teres, supplying the lateral segments (segments II and III) of the left lobe. It describes a wide and anteriorly concave curve and ends in the superior and inferior segmental branches of segment IV. Variation of normal branching pattern of portal vein has been reported since 1957 and occurs in approximately 20% of the population [8, 9]. The most common patterns are trifurcation of the MPV (7.8-10.8%), right posterior segmental branch arising from the MPV (4.7-5.8%) and right anterior segmental branch arising from the LPV (2.9-4.3%) [9]. Absence of portal vein bifurcation is seen in 1.5% to 1.9% of cases during hepatobiliary surgery and if it is unrecognized, it has serious implication for liver resection and split liver transplantation [10].
Detail assessment of vascular anatomy is very important for any surgery and percutaneous radiological intervention. However knowledge about portal vein and its variants is essential during liver resection split liver transplant, transhepatic portal vein embolization and transjugular intrahepatic portosystemic shunts. CT portography and biphasic magnetic resonance imaging of liver in arterial and portal vein phase with maximum intensity projection, multiplanar imaging and volume rendering imaging (3D) demonstrate the detail anatomical pattern of portal vein course and its branching pattern noninvasively [11]. Portal vein variants are usually asymptomatic. In our case the contrast-enhanced CT scan of abdomen was done in venous phase for evaluation of pain abdomen and the portal vein anomaly was detected incidentally. The patient responded well to laxative and conservative management.
In conclusion, knowledge of normal and abnormal anatomy of portal vein course and branching pattern is essential for correct vascular anatomy interpretation in imaging, for liver surgery and percutaneous radiological intervention. These variants can be better demonstrated in detail by multidetector contrast enhanced CT study of abdomen with three dimensional maximum intensity projection and reconstructions.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download