Abstract
Vertebral osteophytes are a characteristic feature of intervertebral disc degeneration. In the lumbar spinal region, the two major structures in close proximity anterior to the spine are the inferior vena cava and the abdominal aorta, both of which have been reported to be affected by osteophytes. The purpose of this study was to determine the distribution, classification and lengths of osteophytes in the lumbar vertebrae. One hundred and eighty lumbar columns of 90 males and 90 females from Chiang Mai, Thailand, in the age range 15 to 96 years (mean age, 63 years) were collected. The measuring length of osteophytes was assessed on vertebral body and articular facet. Statistical analysis was performed by descriptive analysis, chi-square and Pearson Correlation. Lumbar osteophytes were presented in 175 specimens (97.2%), 88 males and 87 females. The highest frequency was at L4, most were on the superior, inferior surface of body and articular facet (39.7%, 38.4%, and 22%), respectively. The greatest mean length was 3.47±2.21 mm at L5, and the longest length of anterior superior surface of body was 28.56 mm. The osteophyte length was significantly correlated directly with age (P<0.01), and males were significantly greater than females (P<0.05). The highest prevalence of osteophytes was on the anterior side of superior surface of body (30.4%), and the classification was traction. It can be proposed that the abdominal aorta could be damaged, especially a risk of rupture of abdominal aortic aneurysm.
It is not well known that anterior and lateral lumbar osteophytes often cause injury to the abdominal aorta and inferior vena cava located to the front of them. Aortic perforation caused by a vertebral osteophyte in the absence of a major trauma has not previously been described. However, there have been some reports of abdominal aortic aneurysm (AAA) ruptures caused by anterior osteophytes.
There is a case report of a patient who was admitted with acute abdominal pain radiating to the back. Computed tomography examinations showed a needle-thin perforation of the aorta, opposite the origin of the superior mesenteric artery, with a pseudoaneurysm. A needle-sharp spinal osteophyte was located exactly opposite the perforation [1]. There is a significant association between increased anterior lumbar osteophytes and prevalence of abdominal aortic calcification (AAC) in both genders (P<0.001) [2]. The presence of calcified lesions in the abdominal aorta has been associated with cardiovascular morbidity and mortality [3, 4]. The purpose of this paper is to describe the distribution, lengths and classification of lumbar osteophytes, especially in the anterior and lateral sides of the lumbar vertebral body.
One hundred and eighty Thai specimens of dry lumbar vertebral columns between L1-L5 (90 males and 90 females) were recruited from the Department of Anatomy, Faculty of Medicine, Chiang Mai University. They consisted of five age groups: 15-35, 36-60, 61-75, 76-85, and >85 years old (6, 68, 72, 25, and 9 lumbar columns, respectively). The average age was 63 years old (range, 15-96 years old). The locations of osteophytes were observed from the edges of the superior, inferior surfaces of the body, and the articular facet of the lumbar vertebrae in the anterior, lateral, posterior and posterolateral areas. The three groups were classified according to Macnab [5] into traction (Fig. 1A), claw (Fig. 1B) and fusion types (Fig. 1C). Analysis was performed by percentile, mean and standard deviation, correlation of osteophytes with gender, and of age with osteophyte length by chi-square and Pearson correlation.
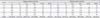
Of the 180 lumbar columns, osteophytes were found in 175 columns (97.2%), 88 out of 90 columns in males (97.8 %) and 87 out of 90 columns in females (96.7%), being not significant by gender (P>0.05). The prevalence of osteophytes was higher in the order of L4, L5, L1, L2, and L3 (Table 1). The osteophytes occurred at 100% in all groups, with the exception of the age group of 15-35 years (Table 2). The one column that presented osteophytes within the age group of 15-35 years was a 31-year-old female. The osteophytes were mostly found in the superior and inferior surfaces of the body and articular facet (39.7%, 38.4%, and 22%, respectively). A greatest prevalence of osteophytes on the superior surface of body, inferior surface of body and articular facet of lumbar vertebrae were 39.7%, 38.4%, and 22.0%, respectively. The greater prevalence of osteophytes was found on the anterior side of the superior surface of body (30.4%) and the lateral side of inferior surface (26.2%) (Table 3).
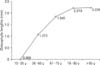
The osteophytes were classified into traction, claw and fusion types (78.5%, 17.5%, and 4.0%, respectively). The main traction osteophytes were present at the anterior, left lateral and right lateral sides, respectively (Table 4). The prevalence in traction type was higher than in claw and fusion types at all levels (Fig. 2).
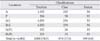
The average lengths of osteophytes were 3.47±2.21 mm at L5, 2.90±1.92 mm at L4, and 2.37±1.57 mm at L3. The longest lengths of osteophytes on anterior superior surface of body L5, L4, and L3 were 28.56, 23.18, and 17.72 mm, respectively. The osteophyte length was significantly correlated directly with age (P<0.01) (Fig. 3), and the osteophyte length of males was significantly greater than females (P<0.05) (Table 5).
The prevalence of osteophytes was very high in this study 97.2% (175 out of 180 columns). There was a similarity between male and female specimens. The present study showed the prevalence of 97.8% in male and 96.7% in female columns. Pye et al. [6] in a UK study analysed 585 lumbar lateral spinal radiographs, 286 males and 299 females. Their results showed osteophytes present in 73% specimens. In the study of O'Neill et al. [7], 681 female and 499 male patients were studied; 84% men and 74% women had at least one vertebra of a grade 1 or higher osteophyte.
In the United States, more than 80% of individuals older over 40 years of age have lumbar spondylosis [8]. The present study found osteophytes in all lumbar columns of those over 35 years old. The prevalence of osteophytes in this study was higher than in other reports [6, 7]. It is thought that the visual method used in the present study is more accurate than the radiological approach.
The primary cause of osteophytes is degeneration of the intervertebral disc; loss of disc height occurs with subsequent peripheral annular bulging. Proteoglycans and water escapes through fissures formed with the degeneration of annulus fibrosus, resulting in further thinning of disc space; vertebral sclerosis and osteophytic formation ultimately follow [9]. This study found more frequency of osteophytes at L4 and L5 for the reasons that could be consistent with the report of Panjabi et al. [10]. In the studies of intradiscal pressure and volume measurements in 84 fresh cadaveric lumbar spine disc spaces, the greater degeneration was found at lower levels of the lumbar spine as compared to the upper levels. Heuer et al. [11] investigated the annular fiber strains and disc bulging under simple and complex spinal loads. A novel laser scanner was used to image surfaces of six L2-3 segments. Loading was applied in the flexion, extension, lateral bending directions and combined directions. Two conditions were measured; intact and defect (vertebral body-disc-body units). The flexion produced 7.2% fiber associated strains and 1.63 mm bulge going up to 17.5% and 2.21 mm after the defect. Highest fiber associated strains were found for the combination of axial rotation plus lateral bending with 24.6% and with a maximal bulging of 1.14 mm. McGill [12] reported that the differences in range of motion between L4-L5 and L5-S1 in the three movements are more flexion in L4-L5, and more extension in L5-S1, more lateral bending in L4-L5, more rotation in L4-L5.
The most common cause of aortic aneurysms is arteriosclerosis. Arteriosclerosis can weaken the aortic wall and the pressure of the blood being pumped through the aorta causes expansion at the site of weakness. The exact cause is unknown, but risk factors for developing aortic aneurysm include: smoking, high blood pressure, high cholesterol, genetic factors and obesity. The stress occurring from osteophytes may render the overlying aortic wall ischemic and thus more vulnerable to infection by blood borne bacteria, because the osteophyte must have exerted pressure on the aortic wall before the perforation occurred [1].
The present study found anterior and lateral traction osteophytes in greater numbers than posterior and posterolateral traction osteophytes. These osteophytes can pressurize the abdominal aorta or inferior vena cava wall leading to ischemia or perforation. In the study of Karasik et al. [2], a significant association between increased anterior lumbar osteophytes and prevalent AAC was demonstrated. The statistic showed a male odds ratio (OR, 1.20), 95% confidence interval (95% CI, 1.1-1.3) per unit increased in osteophytes and that in women (OR, 1.25; 95% CI, 1.1-1.4).
The prevalence of AAAs has been reported to be higher in men than in women [13]. The majority of studies (AAA diagnosed by means of autopsies, ultrasound screening, and hospital discharge data) demonstrated the percentage of AAAs diagnosed in women to be 19% to 34% and the percentage diagnosed in men to be 66% to 81% [14, 15, 16, 17]. The margins of vertebral bodies are normally smooth. Growth of new bone projecting horizontally at these margins identifies osteophytes. Most osteophytes are anterior or lateral in projection. Posterior vertebral osteophytes when presented may contribute to lumbar stenosis which is increasingly diagnosed in Thais. Postero-lateral osteophytes can compress lumbar spinal nerve roots causing back and leg pain. A high prevalence of anterior and lateral osteophytes was found in this study. This may cause pressure on the abdominal aorta and inferior vena cava with serious health implications.
Figures and Tables
Fig. 1
The classification of osteophytes. (A) Traction type. (B) Claw type. (C) Fusion type (L4-L5).

Fig. 2
The percentage of traction, claw and fusion osteophytes on superior and inferior surfaces of body L1-L5.

Table 3
The number of osteophytes on superior surface of body and inferior surface of body at anterior (A), posterior (P), left lateral (Lt.L), right lateral (Rt.L), left posterolateral (Lt.PL), right posterolateral (Rt.PL) sides
References
1. Dregelid E, Jenssen G, Jonung T, Braaten A. Pseudoaneurysm of the abdominal aorta due to a needle-like osteophyte on the first lumbar vertebra. J Vasc Surg. 2007; 45:1059–1061.
2. Karasik D, Kiel DP, Kiely DK, Cupples LA, Wilson PW, O'Donnell CJ, Felson DT. Abdominal aortic calcification and exostoses at the hand and lumbar spine: the Framingham Study. Calcif Tissue Int. 2006; 78:1–8.
3. Witteman JC, Kok FJ, van Saase JL, Valkenburg HA. Aortic calcification as a predictor of cardiovascular mortality. Lancet. 1986; 2:1120–1122.
4. Iribarren C, Sidney S, Sternfeld B, Browner WS. Calcification of the aortic arch: risk factors and association with coronary heart disease, stroke, and peripheral vascular disease. JAMA. 2000; 283:2810–2815.
5. Macnab I. The traction spur. An indicator of segmental instability. J Bone Joint Surg Am. 1971; 53:663–670.
6. Pye SR, Reid DM, Lunt M, Adams JE, Silman AJ, O'Neill TW. Lumbar disc degeneration: association between osteophytes, end-plate sclerosis and disc space narrowing. Ann Rheum Dis. 2007; 66:330–333.
7. O'Neill TW, McCloskey EV, Kanis JA, Bhalla AK, Reeve J, Reid DM, Todd C, Woolf AD, Silman AJ. The distribution, determinants, and clinical correlates of vertebral osteophytosis: a population based survey. J Rheumatol. 1999; 26:842–848.
8. Rothschild BM. Lumbar spondylosis: epidemiology [Internet]. New York: Medscape;2011. cited 2012 Sep 14. Available from: http://emedicine.medscape.com/article/249036-overview#a0199.
9. Klaassen Z, Tubbs RS, Apaydin N, Hage R, Jordan R, Loukas M. Vertebral spinal osteophytes. Anat Sci Int. 2011; 86:1–9.
10. Panjabi M, Brown M, Lindahl S, Irstam L, Hermens M. Intrinsic disc pressure as a measure of integrity of the lumbar spine. Spine (Phila Pa 1976). 1988; 13:913–917.
11. Heuer F, Schmidt H, Wilke HJ. The relation between intervertebral disc bulging and annular fiber associated strains for simple and complex loading. J Biomech. 2008; 41:1086–1094.
12. McGill S. Low back disorders: evidence-based prevention and rehabilitation. 2nd ed. Champaign: Human Kinetics;2007. p. 73.
13. Harthun NL, Cheanvechai V, Graham LM, Freischlag JA, Gahtan V. Prevalence of abdominal aortic aneurysm and repair outcomes on the basis of patient sex: Should the timing of intervention be the same? J Thorac Cardiovasc Surg. 2004; 127:325–328.
14. Bridges PS. Vertebral arthritis and physical activities in the prehistoric southeastern United States. Am J Phys Anthropol. 1994; 93:83–93.
15. Yamada Y, Okuizumi H, Miyauchi A, Takagi Y, Ikeda K, Harada A. Association of transforming growth factor beta1 genotype with spinal osteophytosis in Japanese women. Arthritis Rheum. 2000; 43:452–460.
16. Kramer PA, Newell-Morris LL, Simkin PA. Spinal degenerative disk disease (DDD) in female macaque monkeys: epidemiology and comparison with women. J Orthop Res. 2002; 20:399–408.
17. Yoshimura N, Dennison E, Wilman C, Hashimoto T, Cooper C. Epidemiology of chronic disc degeneration and osteoarthritis of the lumbar spine in Britain and Japan: a comparative study. J Rheumatol. 2000; 27:429–433.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download