Abstract
Nerve root anomalies are frequently underrecognized regardless of the advances in imaging studies; they are also underappreciated and underreported when encountered surgically. The classification of conjoined nerve roots is based on whether the nerve root emerges at an abnormal level or from an anastomotic branch. In the present report, we describe case with a conjoined nerve root that emerged at a more caudal level than that normally observed that was an undiagnosed on preoperative imaging studies. We also discuss the atypical imaging features obtained through preoperative imaging studies. As observed in the present case, preoperative recognition and diagnosis of such anomalies offer the best opportunity of performing a successful procedure and preventing inadvertent damage to nerve roots intraoperatively.
In general, the spinal nerve root exiting the spinal cord is surrounded by a root sleeve extension of dura mater [1]. It runs from the medial to lateral direction along the inferior surface of the corresponding pedicle, exiting through the intervertebral foramen. A conjoined nerve root is defined as two adjacent nerve roots that share a common dural envelope at some point during their course from the thecal sac [2]. The prevalence of lumbosacral nerve root anomalies in autopsies is 8.5-30%, which is considerably greater than the values (1.9-4%) reported in previous imaging studies [3]. When present, conjoined nerve roots emerge most commonly from L5-S1 [4]. One study reported that dorsal roots are more frequently affected by this anomaly than ventral roots, although the cause is not clear [5]. Bifurcation of conjoined nerve roots occurs close to the intervening pedicle, after which they emerge through their respective foramina [6]. Abnormal root anastomosis may result from the connection of a band of nerve fibers or a complete distal union in a common sheath [7]. The classification of conjoined nerve roots is based on whether the nerve root emerges at an abnormal cranial level or from an anastomotic branch.
Conjoined nerve roots are frequently undiagnosed prior to an operation and may cause considerable difficulty during spinal procedures during nerve root mobilization [1]. Accordingly, several imaging and physical examination techniques have been proposed to diagnose and address anomalous roots [4]. Although there is some controversy concerning the reliability of these signs, recent findings suggest that magnetic resonance imaging (MRI) can accurately identify the presence of conjoined nerve roots [8, 9]. Here, we present the case of a man with acute low back pain radiating down the right leg, which was undiagnosed on preoperative imaging studies.
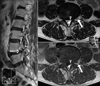
A 71-year-old man presented with acute low back pain and radiating pain in the right leg, with a positive straight-leg raising sign at 30°. He had a history of minor trauma suggestive of a lumbar sprain. His symptoms had gradually worsened, and he was unable to walk due to aggravation of pain in the back and leg upon standing or walking. On manual muscle testing, muscle weakness was not detected in the extremities. His patellar tendon reflexes were normal. On neurological examination, L5 nerve root compression was identified. On plain lumbar spine radiographs, spinal abnormalities, except for spondylolisthesis, were difficult to detect. Slight disc space narrowing at L4-5 was noted in lateral view (Fig. 1). Computed tomography showed no definite bone abnormalities. MRI revealed disc herniation at both root exits at the L4-5 intervertebral disc level (Fig. 2). Based on these observations, we diagnosed the patient with spondylolisthesis and lumbar disc herniation at L4-5.
Intraoperatively, disc sequestration was noted, and the herniated disc was found to be incarcerated to the adjacent conjoined L5 nerve roots. Upon further investigation, we discovered that the L5 nerve root originated from the caudal level of the L5 pedicle and was conjoined with the S1 nerve root (Fig. 3). The disc herniation at L4-5 migrated bilaterally and was found beneath the abnormal conjoined nerve roots. After removal of the disc herniation and unroofing of the nerve root, we did not observe any obvious mobility of the conjoined nerve root. After surgery, the patient's leg pain immediately disappeared and no muscle weakness was recorded. Upon retrograde imaging review, we observed several signs of conjugated nerve roots on routine MRI images (Fig. 4): the "sagittal shoulder sign," a vertical structure connecting two consecutive nerve roots and the overlying herniated disc on the parasagittal MRI which represents a combination of a protruded or extruded disc adjacent to a conjoined nerve root; "corner sign," asymmetric structure of the anterolateral corner of the dural sac with one side being angulated compared with the other; "fat crescent sign," the presence of extradural fat between the conjoined nerve root and the asymmetric dural sac; and "parallel sign," an unusual course of the entire nerve root at the disc level, running parallel to the disc plane.
A conjoined nerve root is defined as two adjacent nerve roots that share a common dural envelope at some point during their course from the thecal sac [2]. General information about conjoined nerve root is summarized in Table 1. Several authors have proposed classifications for conjoined nerve roots, but the classification proposed by Postacchini et al. [3] is most commonly used. According to this classification, type I refers to one or more roots that emerge at an abnormal cranial level; type II refers to one root that emerges at a more caudal level than normal; type III refers to two or more nerve roots that emerge through closely adjacent openings of the dura; type IV refers to two nerve roots that emerge from the dural sac in a common nerve trunk; and type V refers to an anastomotic branch that connects two nerve roots in their extrathecal course. These anomalous roots may or may not leave the vertebral canal through their correct intervertebral foramina [1]. Type II is the most common type [3] and corresponds to the type illustrated by the present case-The L5 nerve root originated from the caudal level of the L5 pedicle and conjoined with the S1 nerve root.
MRI is the gold standard for differentiating conjoined nerve root anomalies from other space-occupying processes. Although a T2-weighted coronal MRI is the best method for tracking the course of a conjoined nerve root, such imaging studies are not usually conducted. This sequence displays images of the course of the roots under their corresponding pedicles and their sleeves, similar to a myelogram [8]. Kang et al. [9] reported that the "sagittal shoulder sign" occurred in 90.9% of surgically documented cases of conjoined lumbosacral nerve roots compromised by herniated discs. This sign was detected on both T1- and T2-weighted MRI sequences and is defined as "a vertical structure connecting two consecutive nerve roots and the overlying herniated disc on the parasagittal MRI, which represents the combination of a protruded or extruded disc adjacent to a conjoined nerve root" [9]. We also observed this sign described by Kang et al. [9] in the present case (Fig. 4).
Additionally, Song et al. [10] described three radiological signs on standard axial MRI at the level of the disc, all of which are more easily detected on T1-weighted images. The "corner sign" is described as an asymmetric structure of the anterolateral corner of the dural sac, with one side being angulated compared to the other. This sign may also be observed in other conditions such as epidural lipomatosis and spinal stenosis. The "fat crescent sign" refers to the presence of extradural fat between the conjoined nerve root and the asymmetric dural sac. A ''parallel sign'' denotes an unusual course of the entire nerve root at the disc level, running parallel to the disc plane. Such observations suggest that T1-weighted MRI axial images can be routinely reviewed to assess nerve root anomalies, owing to a more intense contrast between the dural sac and intervening dural fat. All the above signs described by Song et al. [10] were identified in the present case. Despite the established description of these typical signs of conjoined nerve roots, MRI diagnosis is subject to several limitations. Imaging in the most useful planes is not routinely conducted in many studies, and false-positive findings are also possible with this method. However, preoperative diagnosis of a conjoined nerve root, or even a high index of suspicion of an anomaly, may greatly aid the spinal surgeon and decrease the chances of operative complications [1].
Conjoined nerve roots are frequently undiagnosed prior to an operation and may cause considerable difficulty during spinal procedures involving nerve root mobilization. Medical history and physical findings often vary and mostly resemble those of a herniated disc with symptoms not necessarily presenting in a dermatome distribution. Moreover, there are no pathognomonic signs associated with lumbar conjoined nerve roots. Conjoined nerve roots are generally fixed, and are consequently difficult to retract during spinal surgeries. The roots could be irritated and inflamed during forceful retraction, which may increase tension on the nerve roots and cause postoperative neurologic deficit and neuropathic pain. A nerve root anomaly could be mistaken for a portion of protruding or herniated disc and incised inadvertently, resulting in iatrogenic neural injury. Thus, great care should be taken before surgery to minimize perioperative complications in cases with conjoined nerve roots. Several radiographic signs of conjoined lumbar nerve roots have been described using standard MRI techniques. Coronal MRI, with T1- and T2-weighted images, should be performed if a conjoined nerve root anomaly is suspected.
Figures and Tables
Fig. 3
Images of conjoined nerve roots at the left L5 root classified as Type 1a, according to Neider and MacNab's classification.

Acknowledgements
This study was supported by the Teun Teun Research Foundation and no external funding was received.
References
1. Trimba R, Spivak JM, Bendo JA. Conjoined nerve roots of the lumbar spine. Spine J. 2012; 12:515–524.
2. Scuderi GJ, Vaccaro AR, Brusovanik GV, Kwon BK, Berta SC. Conjoined lumbar nerve roots: a frequently underappreciated congenital abnormality. J Spinal Disord Tech. 2004; 17:86–93.
3. Postacchini F, Urso S, Ferro L. Lumbosacral nerve-root anomalies. J Bone Joint Surg Am. 1982; 64:721–729.
4. Lotan R, Al-Rashdi A, Yee A, Finkelstein J. Clinical features of conjoined lumbosacral nerve roots versus lumbar intervertebral disc herniations. Eur Spine J. 2010; 19:1094–1098.
5. White JG 3rd, Strait TA, Binkley JR, Hunter SE. Surgical treatment of 63 cases of conjoined nerve roots. J Neurosurg. 1982; 56:114–117.
6. Phillips LH 2nd, Park TS. The frequency of intradural conjoined lumbosacral dorsal nerve roots found during selective dorsal rhizotomy. Neurosurgery. 1993; 33:88–90.
7. Artico M, Carloia S, Piacentini M, Ferretti G, Dazzi M, Franchitto S, Bronzetti E. Conjoined lumbosacral nerve roots: observations on three cases and review of the literature. Neurocirugia (Astur). 2006; 17:54–59.
8. Gomez JG, Dickey JW, Bachow TB. Conjoined lumbosacral nerve roots. Acta Neurochir (Wien). 1993; 120:155–158.
9. Kang CH, Shin MJ, Kim SM, Lee SH, Kim HK, Ryu JA, Lee CS, Kim SS. Conjoined lumbosacral nerve roots compromised by disk herniation: sagittal shoulder sign for the preoperative diagnosis. Skeletal Radiol. 2008; 37:225–231.
10. Song SJ, Lee JW, Choi JY, Hong SH, Kim NR, Kim KJ, Chung SK, Kim HJ, Kang HS. Imaging features suggestive of a conjoined nerve root on routine axial MRI. Skeletal Radiol. 2008; 37:133–138.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download