Abstract
The palmaris longus (PL) is a slender, spindle-shaped weak flexor of the wrist. Congenital absence of the PL is estimated to occur in 15% among individuals worldwide. However, the frequency of its absence varies considerably among different population groups and with different detection techniques. In the present study, the presence of the PL tendon was examined in a Korean population (n=269) using three clinical tests, namely the Traditional Test, Mishra's Test II, and the Gangata Test. We classified subjects into six types based on whether inspection or palpation was required to determine the presence of the PL and flexor carpi radialis. The most reliable test was determined using Kendall's coefficient of concordance. Our results showed that the PL tendon was absent in 4.1% of the subjects in our study, and bilateral and unilateral absences were 2.2% and 1.8%, respectively. Statistical analysis revealed that these tests had similar reliability for assessing the PL tendon, and the Traditional Test showed the highest effectiveness, at 93%. Therefore the Traditional Test was found to be the most effective for revealing the PL in this Korean population.
The palmaris longus (PL) is a slender, spindle shaped weak flexor of the wrist and it is located medial to the flexor carpi radialis (FCR). The PL muscle is extremely variable in both number and form [1]. As for its clinical significance, many clinicians have focused on the PL for its use in tendon grafts. Previous studies have suggested that the muscle is more commonly absent in women, and that it has a tendency to occur bilaterally, a finding that is independent of its interethnic variations [2, 3]. The rate of congenital absence of the PL is estimated to be 15% among individuals worldwide and its incidence is population-dependent - from 0.6% (in the Korean population) to 63.9% (in the Turkish population) [4-7].
To determine the best technique to assess the absence of the PL, various methods have been used [8, 9]. In the detection tests, differing results were obtained because each test varied in their method and effectiveness for detecting muscles that were in close relation to the PL. In particular, the PL and FCR muscles were frequently mistaken for each other due to their close relationship [10]. Therefore, palpation is needed to detect the presence of the tendon in question when it is difficult to visually identify the tendons. To investigate the effectiveness and consistency of various tests revealing the PL, Ndou et al. [11] studied the patterns of the PL and FCR tendons using three different methods.
One of the aims of this study was to examine the frequency of absence of the PL. In addition, we compared the effectiveness and consistency of various tests revealing the PL in a Korean population. The results obtained may have clinical significance for the detection of the PL and FCR in a racially homogenous group.
For the purpose of this study, 269 subjects who were students in the colleges of medicine and nursing at Keimyung University, were examined. Of the 269 subjects, 149 were male and 120 were female, with an age range between 18 and 30 years (mean age, 26.3 years). Individuals with a history of injury, disease or other abnormality of the upper extremity that would preclude examination for the presence of the PL tendon were excluded from the study. Only one examiner performed this study; this was to reduce the error by plural examiners. The absence of the PL and the type of the PL and FCR were investigated as previous described [11]. The following tests were used:
1) Traditional Test: The thumb opposes the fifth finger with slight wrist flexion [3].
2) Gangata Test: Thumb abduction is resisted as well as wrist flexion [8].
3) Mishra's Test II: The thumb is abducted against resistance with the wrist in slight flexion [9].
A positive result in the Type I and II means that the PL is present and absent, respectively. If the PL is present, then the type of the PL was classified according to the degree of prominence of the two tendons as in the following (Fig. 1).
1) Type Ia: Both the tendons of the PL and FCR are visible and no palpation is required.
2) Type Ib: Only the tendon of the PL is visible whereas the tendon of the FCR can be located by palpation. The arrow indicates the position of the FCR.
3) Type Ic: Only the tendon of the FCR is visible, whereas the tendon of the PL can be located by palpation. The arrow indicates position of the PL.
4) Type Id: Neither the tendon of the PL nor that of the FCR are visible but both tendons may be located by palpation.
If the PL is absent, then the type of the PL was classified according to the degree of prominence of the two tendons as in the following.
1) Type IIa: The tendon of the FCR is visible, whereas the tendon of the PL is neither visible nor palpable.
2) Type IIb: The FCR is not visibly present and it can only be located by palpation, whereas the PL is not visible and it is not palpable.
We tested the effectiveness of each testing method as previously described [11]. The effectiveness of each test was assessed against the majority outcome. The majority outcome was defined as the result that was consistent in at least two of the tests.
All the statistical analyses were carried out using SPSS (version 18, SPSS Inc., Chicago, IL, USA). The prevalence of the absence of the PL (unilateral or bilateral) was presented with a 95% confidence interval. The association between an absent PL and the body side and gender was assessed using chi-square tests or Fisher's exact tests. Statistical significance was set at P<0.05. Kendall's coefficient of concordance was used to test for agreement of the results obtained by the three different tests used in the study. This was done to determine the most effective clinical test for assessing the PL.
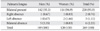
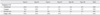
The overall prevalence of the absence of the PL tendon (unilateral or bilateral) was 4.1% (11 subjects), and the frequency of absence in the males and females were 4.7% and 3.3%, respectively. The PL tendon was absent unilaterally in 5 subjects (1.8%) and the frequency of unilateral absence in the males and females were 1.3% and 2.5%, respectively. The PL tendon was absent bilaterally in 6 subjects (2.2%), and the frequency of bilateral absence in the males and females were 3.3% and 0.8%, respectively (Table 1). Laterality and gender have no statistical significance in the absence of the PL. If the PL tendon was present, then Type Ia and Ib were the dominant types. Without the PL tendon, the dominant form was Type IIa, and the tendon of the FCR was visible in all three tests. The highest consistency of the kappa values for the three tests was found for Types Ia, Ib, IIa, and IIb (0.55, 0.52, 1, and 1, respectively). The three tests that were used exhibited inconsistent results for Types Ic and Id, with Kappa values of 0.01 and 0.15, respectively (Table 2). The Traditional Test had an effectiveness rate of 93%, whereas the Gangata Test and Mishra's Test II had effectiveness rates of 85% and 88%, respectively.
The PL is one of the most variable muscles in the body. In Koreans, the prevalence of an absent PL varies from 0.6% (n=192) [5] to 4.3% (n=1000) [12]. The prevalence (4.1%) in our study was similar with previous studies in an East Asian population (Korean, 4.3%; Chinese, 4.6%; Japanese, 5.6%) [10, 12, 13]. Compared to a non-Asian population like the Turks or Europeans [14], the prevalence of an absent PL is low in East Asian populations, including the Korean population.
Many tests for detecting the PL tendon have been introduced, such as the Traditional Test, the Gangata Test, Mishra's Test II, etc. [3, 8, 9]. A previous study examined the effectiveness and consistency of the various methods used to test for the absence of the PL [11]. Considering that the PL shows differing characteristics depending on the population looked at, we investigated the effectiveness of these methods when used on a Korean population, the first racially homogenous population to be investigated in this way. High consistency of the kappa values for the three tests was found for Types Ia, Ib, IIa, and IIb. However, the Ic and Id Types showed low consistency. Our results demonstrated that Types IIa and IIb showed high consistency (1 on both tests) when the various tests were compared, with the high consistency for Type IIa being in agreement with a previous result (0.98). However, Type IIb showed a different consistency compared to a previous result (0.33) [11]. Also, Types Ic and Id showed low consistency. These differences may arise due to the subjective nature of the judging by the examiner. Types Ic, Id, and IIb were associated with a prominence of the FCR. Their low consistencies may be due the FCR being located below the retinaculum, thereby generating confusion about the presence of the FCR.
A previous study showed that Mishra's Test II was the most effective, followed by the Gangata Test and Traditional Test [11]. However, in our study, the Traditional Test was the most effective, with Mishra's Test II and Gangata Test following. These differences were thought to be due to the fact that both Mishra's Test II and the Gangata Test involve thumb abduction, whereas the Traditional Test does not. It seems that the results obtained by using each of these clinical tests is dependent on the extent to which the muscle in question is involved in a particular movement required for the execution of the test. For example, the Gangata Test is likely to reveal the presence of both the PL and the FCR as this test involves resisting flexion of the wrist, which requires a contribution from these two flexors. Other factors, such as the thickness of the tendons as well as the amount of subcutaneous fat may contribute to the differing interpretations of the presence of the PL and FCR.
A recent study suggested that unilateral PL tendon absence was more common in the non-dominant hand [15]. However, our study showed no relation between hand dominance and PL absence (data not shown).
We examined the frequency of the absence of the PL in the Korean population, and the effectiveness of tests for detecting its absence in the same population. In a Korean population, the frequency of PL absence was low, and the traditional test was the most effective test for detecting the PL. This muscle, although of little functional use to the human upper limb under normal circumstances, assumes great clinical importance in tendon transfer or transplant. Therefore, knowledge about the frequency of its absence and the most effective test for detecting its absence may be highly relevant in the preoperative workup, especially when surgical intervention involving the forearm, and in particular, tendon transfer, is being considered. And it may help clinicians to avoid making a misdiagnosis, and assist in reducing complications that arise during surgical interventions of the upper limb.
Figures and Tables
References
1. Yildiz M, Sener M, Aynaci O. Three-headed reversed palmaris longus muscle: a case report and review of the literature. Surg Radiol Anat. 2000. 22:217–219.
2. Reimann AF, Daseler EH, Anson BJ, Beaton LE. The palmaris longus muscle and tendon. A study of 1600 extremities. Anat Rec. 1944. 89:495–505.
3. Schaeffer JP. On the variations of the palmaris longus muscle. Anat Rec. 1909. 3:275–278.
4. Sebastin SJ, Lim AY, Bee WH, Wong TC, Methil BV. Does the absence of the palmaris longus affect grip and pinch strength? J Hand Surg Br. 2005. 30:406–408.
5. Ahn DS, Yoon ES, Koo SH, Park SH. A prospective study of the anatomic variations of the median nerve in the carpal tunnel in Asians. Ann Plast Surg. 2000. 44:282–287.
6. Ceyhan O, Mavt A. Distribution of agenesis of palmaris longus muscle in 12 to 18 years old age groups. Indian J Med Sci. 1997. 51:156–160.
7. Hiz Ö, Ediz L, Ceylan MF, Gezici E, Gülcü E, Erden M. Prevalence of the absence of palmaris longus muscle assessed by a new examination test (Hiz-Ediz Test) in the population residing in the area of Van, Turkey. J Clin Exp Invest. 2011. 2:254–259.
8. Gangata H. The clinical surface anatomy anomalies of the palmaris longus muscle in the Black African population of Zimbabwe and a proposed new testing technique. Clin Anat. 2009. 22:230–235.
9. Mishra S. Alternative tests in demonstrating the presence of the palmaris longus. Indian J Plast Surg. 2001. 34:12–14.
10. Sebastin SJ, Lim AY. Clinical assessment of absence of the palmaris longus and its association with other anatomical anomalies: a Chinese population study. Ann Acad Med Singapore. 2006. 35:249–253.
11. Ndou R, Gangata H, Mitchell B, Ngcongo T, Louw G. The frequency of absence of palmaris longus in a South African population of mixed race. Clin Anat. 2010. 23:437–442.
12. Won CH, Chang BS, Chung MS. Palmaris longus in Korean. J Korean Orthop Assoc. 1994. 29:1561–1563.
13. Ito MM, Aoki M, Kida MY, Ishii S, Kumaki K, Tanaka S. Length and width of the tendinous portion of the palmaris longus: a cadaver study of adult Japanese. J Hand Surg Am. 2001. 26:706–710.
14. Kose O, Adanir O, Cirpar M, Kurklu M, Komurcu M. The prevalence of absence of the palmaris longus: a study in Turkish population. Arch Orthop Trauma Surg. 2009. 129:609–611.
15. Erić M, Koprivčić I, Vučinić N, Radić R, Krivokuća D, Lekšan I, Selthofer R. Prevalence of the palmaris longus in relation to the hand dominance. Surg Radiol Anat. 2011. 33:481–484.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download