Introduction
A through understanding of the anatomy of the lower eyelids and the surrounding structures is mandatory to achieve satisfactory surgical results and avoid potential complications.
The aim of this review is to familiarize the reader with the critical lower eyelid anatomy.
Lacrimal canaliculus in the lower eyelid
There has recently been a growing interest in epicanthoplasty in the oriental population. Diverse techniques are employed when performing epicanthoplasty. Most incisions are made near to the lower lacrimal punctum.
Referring to Gray's anatomy textbook, the lacrimal canaliculi (one in each eyelid) are about 10 mm long; they commence at the puncta lacrimalia. The inferior canaliculus at first descends and it then runs almost horizontally to the lacrimal sac (Williams 1995).
Whitnall stated that the total height of the vertical part is 1.5 mm to 2 mm, and 0.5 mm of which forms the infundibulum; the diameter of the punctum is 0.2 to 0.3 mm and the ampulla is 1 mm in diameter (Whitnall 1932). The horizontal portion (pars horizontalis) runs from the base of the vertical portion medially along the lid margin to the lacrimal sac; this part is not strictly horizontal, but it inclines towards its fellow of the opposite lid as it courses medially; the lower one is also slightly curved (Williams 1995).
In 1995 Mlu reported that the mean length of the vertical portion of the lacrimal canaliculi of the both upper and lower eyelids was 2 mm (range: 1.7 to 2.2 mm) and the length of the horizontal portion of the lower lacrimal canalicus was 10 mm (range: 7.0 to 13 mm) (Mlu 1995).
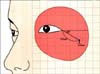
Hwang has recently reported that the depth and width (diameter) of the vertical portion were 2.58±0.24 mm and 0.44±0.07 mm, respectively. The vertical portion of the canaliculus was about 1 mm (1.11±0.16 mm) deep, and the horizontal portion was about 2~3 mm (2.08±2.74 mm) long 2 mm below the mucocutaneous junction, which is where an incision may be made in epicanthoplasty (Fig. 1) (Hwang et al., 2005).
Motor innervation to the lower orbiculis oculi muscle
Ectropion or sclera that shows as a result from weakness of the lower eyelids is not uncommon after lower blepharoplasty or midface lift via a blepha-roplasty incision (McGraw & Adamson 1991; Zarem & Resnick 1993). Such complications are usually secondary to excessive resection of the lower eyelid skin, denervation of the pretarsal orbicularis oculi muscle (OOM), scar contracture of the orbital septum (middle lamella) or failure of midface suspension (Stuzin 1999). Close clinical observation disclosed that the main cause may be the denervation of the pretarsal OOM (Stuzin 1999).
Ramirez (Ramirez & Santamarina 2000) reported that the traditional concept of innervation to the lower OOM should be discarded. Three to five twigs of the zygomatic branch of the facial nerve entered the OOM at a right angle. No nerve penetration was found lateral to the OOM. In a few cases we experienced limited ectropion to the lateral portion of the lower eyelid after an extended midface lift. This complication may be the result of injury of the zygomatic branch.
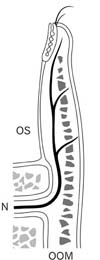
Hwang (Hwang et al., 2001) reported that all pretarsal and preseptal OOMs were innervated by five to seven terminal twigs of the zygomatic branches of the facial nerve that approached the muscle at a right angle. The medial portion of the lower OOM was innervated by one to two terminal twigs of the buccal branch, and the middle portion was innervated with two to three twigs of the zygomatic branch. The lateral portion of the lower eyelid was supplied by the uppermost zygomatic branch, which split into two to four twigs (Fig. 2A). The mean horizontal distance between the lateral canthus and the zygomatic branch was 2.31±0.29 cm (range: 1.7~2.7 cm) and the vertical distance was 1.20±0.20 cm (range: 0.8~1.5 cm). The critical zone was a circle with a 0.5 cm radius, and its center was located 2.5 cm inferolaterally (30 deg) from the lateral canthus (Fig. 3). Hwang (Hwang et al., 2001) emphasized that it is very important to understand the motor nerve innervation of the lower eyelid and the "critical zone" to avoid postoperative ectropion or weakness of the lower eyelid resulting from paralysis of the pretarsal or preseptal OOM.
Sensory innervation of lower eyelid skin
The loss of skin sensation or numbness following lower blepharoplasty is not uncommon (Klatsky & Manson 1981; Black et al., 2002).
Gray's Anatomy (Standring 2005) describes that "the lower eyelid skin is supplied principally by the infraorbital branch of the maxillary nerve and small branches of the lacrimal and infratrochlear nerves." However, the distribution pattern of each nerve is never clearly described, nor is the plane where the nerves course.
Hwang stated that the infraorbital nerve (ION) and zygomaticofacial nerve (ZFN) came out of the infraorbital foramen and zygomaticofacial foramen, respectively. They ran along superficial to the periosteum within and beneath the epimysium of the orbicularis oculi muscle (OOM) and then through the OOM perpendicularly, and they are distributed to the skin. The distal branch approached to the lower border of the tarsal plate (Fig. 4). The majority of the terminal branches (93.8%) of the ION were distributed to the medial to the lateral canthus. Only a few branches (6.2%) were lateral to the lateral canthus. Most (99.4%) terminal branches of the ZFN are distributed to lateral to the lateral canthus. Very few (0.6%) branches were medial to the lateral canthus (Fig. 5).
They insisted that the skin-muscle flap infringes less than the skin flap on the terminal branches of the ION and ZFN when surgically exposing the orbital floor as well as when performing lower blepharoplasty.
Retractor of the lower eyelid: capsulopalpebral fascia
Suturing of the capsulopalpebral fascia (CPF) to the periosteum of the orbital rim has been developed by de la Plaza for the treatment of palpebral bags (de la Plaza & Arroyo 1988). Mendelson has recently used and reported on this technique (Mendelson 2001).
A good knowledge of the anatomic relationship of the CPF with the orbital septum (OS) is essential for the technique of the above two authors. However, the relation of the two structures is absurd and controversial. Some authors reported that the CPF blended with the OS beneath the lower border of the tarsal plate (Hawes & Dortzbach 1982; Hornblass 1988; Bosniak 1990; Dortzbach 1994). Others contended there is no clear blending of the CPF and the OS (Ellis & Zide 1995; Lim et al., 2004; Standring 2005).
Hornblass described that the capsulopalpebral fascia proceeds anteriorly and superiorly to fuse with the orital septum approximately 5 mm below the lower tarsal edge, and above that a single fascial sheath passes upward to attach onto the lower border of the tarsus (Hornblass 1988). Hawes emphasized that the lower lid retractors fuse with the orbital septum approximately 5 mm inferior to the inferior tarsal border before inserting on the tarsal plate (Hawes & Dortzbach 1982). Dortzbach stated that the CPF fuses with the orbital septum 4 mm below the tarsal border and inserts on the tarsus as well as the orbicularis and skin (Dortzbach 1994). Bosniak said that the lower lid retractors insert at or slightly below the inferior tarsal border after fusing with the orbital septum. More inferiorly, the orbital septum is separated from the lower lid refractors by the preaponeurotic fat pad (Bosniak 1990).
All the above authors pointed out that the CPF fuses with the OS below the lower border of the tarsal plate (Hawes & Dortzbach 1982; Hornblass 1988; Bosniak 1990; Dortzbach 1994). In the above studies, the relationship of the CPF with the orbital septum might be searched for and measured on the midpupillary line (Hornblass 1988; Bosniak 1990; Dortzbach 1994). Hawes took the specimen between the midpupillary and lateral limbus line (Hawes & Dortzbach 1982).
Hwang (Hwang et al., 2006) stated that the head of the CPF splits open superiorly and inferiorly and it wraps around the inferior oblique muscle and meets anteriorly. The CPF inserted to the inferior border of the tarsus, and it merged in the anterior border of the inferior tarsal muscles. The OS blended with the CPF most closely at 3.7~5.4 mm beneath the lower tarsal border and differently at 3.7±0.7 mm on the medial limbus line, 4.3±0.8 mm on the midpupillary line and 5.4±1.0 mm on the lateral limbus line. The blending level is closer to the tarsus at the medial side than at the lateral side. The closest distance between the lower tarsal border and the first identifiable smooth muscle nuclei of the inferior tarsal muscle was 2.1~2.7 mm, and differently 2.7±0.7 mm on the medial limbus line, 2.7±0.7 mm on the midpupillary line and 2.1±0.9 mm on the lateral limbus line (Fig. 6).
Arcuate expansion
Mendelson introduced a procedure of replacing bulging infraorbital fat back into the orbit in lower blepharoplasty (Mendelson 2001). The technique involves approximation of the white line of mobile capsulopalpebral fascia (CPF) and the arcus marginalis along the inferior orbital rim and arcuate expansion. Manson stated that the arcuate expansion is a group of fascial strands extending to the orbital rim 10 mm below the insertion of the lateral canthal ligament (Manson et al., 1986).
Codner described that the arcuate expansion of Lockwood's ligament (Clifford's ligament) inserts into the inferolateral orbital rim and fuses with the interpad septum between the central and lateral fat compartments of the lower eyelid and it should be preserved during lower lid dissection to maintain lateral support (Codner & Hanna 2005).
The fascial sheath of the inferior retus is also sparse in the posterior part of the orbit, but anteriorly it is more fully developed and it divides into two layers: an upper layer that joins the capsule of Tenon and runs forward to be inserted into the sclera near the limbus, and a lower layer that contributes to the formation of the suspensory ligament of Lockwood (Duke-Elder 1961).
The lower eyelid has an analogous interior suspensory ligament called Lockwood's ligament. Lockwood's ligament arises from the medial and lateral retinaculum and fuses with the capsulopalpebral fascia inserting in the inferior tarsal border. The function of Lockwood's ligament is to stabilize the lower eyelid depression to increase the inferior visual field on downward gaze (Lockwood 1885; Codner & Hanna 2005).
Scobee described thin sheets of fascia attaching the sheath to the suspensory ligament of Lockwood (Scobee 1948; Duke-Elder 1961). We think this 'thin sheets of fascia' is the earliest description of the arcuate expansion (Scobee 1948).
Manson stated that the arcuate expansion is continuous with the inferior oblique fascia and Lockwood's extension far to the inferior rectus muscle. The length is 11 mm and the width 3 mm on the average (Manson et al., 1986).
The inferior oblique muscle separates the nasal and central fat compartments. The central and lateral fat compartments are also separated by an interpad septum as well as a fascial expansion from Lockwood's ligament, the arcuate expansion (Codner & Hanna 2005). The inferior oblique muscle is between the medial (nasal) and central infraorbital fat pad. Aggressive transposition of this fat by suturing, like a lasso, below to the orbital rim violates the IOM and may result in diplopia. A lateral extent of the lateral fat pocket includes the lateral retinaculum and lateral canthal tendon.
Tanaka recently introduced the 'anterosuperior transverse ligament' which arises from the posteroinferior part of the medial canthus that is fused to the inferolateral orbital rim. He thought that this ligament supports the lower eyelid and prevents downward displacement of the lower eyelid (Tanaka et al., 2008). It is thought that the 'anterosuperior transverse ligament' Tanaka (Tanaka et al., 2008) described is the same structure as Manson (Manson et al., 1986) and Codner (Codner & Hanna 2005) described as the 'arcuate expansion'.
Dutton (Dutton 1994) contended that the arcuate expansion serves to check the inferior rectus and inferior oblique muscles and it also prevents excessive backward displacement of Lockwood's ligament.
Hwang stated that the arcuate expansion (AE) was a fibrous band expanding from the inferolateral orbital rim to the medial canthal ligament. A sector (fan-shaped) of the AE originated in the angle of 5 to 80 degrees at the circumference of the inferolateral orbital rim circle, falling within the range of 3 to 5.5 o'clock, and then it tapered and attached to the inferior border of the medial canthal ligament (Fig. 7). The AE was located deep to the orbital septum and superficial to the inferior oblique muscle (IO). It overlapped the middle part of the IO as it crossed and connected to the capsulopalpebral fascia (Fig. 8).
The tensile strength of the 5 mm width of the AE at halfway and at orbital margin was 6.7±3.8 N and 5.4±2.7 N respectively. Hwang thought the AE prevents the protrusion of the eyeball and orbital fat and it functions as a pulley to hold over-contraction of the IO muscle.
Suborbicularis oculi fat (SOOF) in the lower eyelid
In the lower eyelid, the suborbicularis oculi fat (SOOF) has named as "the supraperiosteal submuscular fat excess situated over the zygoma" (Aiache & Ramirez 1995). For the location and the nature of the SOOF, it has been recognized that the bulk of SOOF is located below the lateral half of the infraorbital rim (Aiache & Ramirez 1995).
Plication of the SOOF and suspension of the midfacial tissue are effective in midfacial rejuvenation (Aiache & Ramirez 1995). SOOF is an elusive entity and can only be visualized from the suborbicularis space during a skin-muscle flap procedure in lower blepharoplasty (Aiache 2001).
In Hwang's recent paper (Hwang et al., 2007), the SOOF was observed in all specimens. The SOOF was located in the inferolateral side of the orbit within a range between medial +15 and lateral -89 degrees to a vertical midpupillary line. SOOF looks like a hockey stick head. SOOF is divided into two parts: the horizontal and vertical parts. The length of the SOOF horizontal part is almost equal to a transverse orbital dimension (a). The height of the SOOF vertical part was about three fourth (b×3/4) of the vertical orbital dimension (b) and the width of the vertical part was one fourth (a/4) of a transverse orbital dimension (a). Most of the SOOF vertical part was outside from the lateral orbital rim and the horizontal part was below the infraorbital rim (Fig. 9). Histologically, the SOOF were situated deep to the Orbicularis oculi muscle and superficial to the orbital septum and periosteum. The SOOF consisted more of a fibrofatty tissue than pure fat tissue like that of the orbital fat (Fig. 10).




 PDF
PDF ePub
ePub Citation
Citation Print
Print










 XML Download
XML Download